INTRODUCTION
Minimally invasive surgery (MIS) is characteristically performed through a small incision or no incision, and visualization is provided by endoscopes. Both laparoscopy and hysteroscopy are considered in this category. With laparoscopy, small abdominal incisions provide access to introduce an endoscope and surgical instruments into the abdomen. To increase operative space, a pneumoperitoneum is created. As such, laparoscopy provides a minimally invasive option for women undergoing intraabdominal gynecologic surgery. And, with its technology improvements, almost all major intraabdominal gynecologic procedures can now be performed with MIS.
Hysteroscopy uses an endoscope and uterine cavity distending medium to provide an internal view of the endometrial cavity. This tool permits both the diagnosis and operative treatment of intrauterine pathology.
FACTORS IN CHOOSING LAPAROSCOPY
In theory, laparoscopic surgery differs from laparotomy only by its mode of access to the operative field. However, inherent qualities can make some surgical steps more difficult. These include indirect palpation of tissue, counterintuitive motion, a finite number of ports for abdominal access, restricted movement, and replacement of normal 3-dimensional (3-D) vision by 2-dimensional (2-D) video images. In appropriately selected patients, the trade-off is a faster recovery, improved cosmesis, less postoperative pain, diminished adhesion formation, and at least equivalent surgical results (Ellström, 1998; Falcone, 1999; Lundorff, 1991; Mais, 1996; Nieboer, 2009). The decision to perform laparoscopy is based on several parameters. Primary among these are patient factors, availability of appropriate instrumentation, and surgeon skill.
Laparoscopy using a pneumoperitoneum is contraindicated in very few clinical conditions, but these include acute glaucoma, retinal detachment, increased intracranial pressure, and some types of ventriculoperitoneal shunts. Thus, laparoscopy is appropriate for many, although modifications are warranted for certain clinical situations. Several are discussed subsequently.
With laparoscopy, adhesive disease increases the risk of visceral and vascular injury during abdominal entry. Adhesions are also associated with higher conversion rates to laparotomy because long and tedious adhesiolysis may be completed by some surgeons more quickly with open surgical dissection techniques. Thus, during preoperative physical examination, a surgeon notes the location of previous surgical scars and ascertains the risk of possible intraabdominal adhesive disease (Table 41-1). Similarly, a history of endometriosis, pelvic inflammatory disease, or radiation treatment may predispose to adhesions. In addition, abdominal wall hernias or hernia repairs and any reparative mesh are identified and avoided during trocar insertion. If abnormal findings are found during this preoperative evaluation, plans for an alternative entry site are considered.
| Sample Size/Prior Surgery | No Prior Surgery | Prior Laparoscopy | Prior Low Transverse Incision | Prior Vertical Midline Incision (VML) | |
| Agarwala (2005) | 918/ surgery | — | 16% | 22% | 62% |
| Brill (1995) | 360/ laparotomy | — | — | 27% | 55% with VML below umbilicus 67% with VML above umbilicus |
| Audebert (2000) | 814/laparoscopy | 0.68% | 1.6% | 19.8% | 51.7% |
| Sepilian (2007) | 151/ laparoscopy | — | 21% | — | — |
Compared with traditional open laparotomy, laparoscopy produces several distinct cardiovascular and pulmonary physiologic changes. These result mainly from: (1) absorption across the peritoneum and into circulation of carbon dioxide (CO2) used for insufflation, (2) increased intraabdominal pressure created by the pneumoperitoneum, and (3) head-down Trendelenburg positioning. These changes are typically tolerated by those in generally good health but may be less so in those with cardiovascular or pulmonary compromise. Thus for patient safety, surgeons should be familiar with these physiologic alterations.
During laparoscopy, a pneumoperitoneum is created, in most cases with CO2. Absorption of this gas across the peritoneum can lead to systemic CO2 accumulation and hypercarbia. In turn, hypercarbia produces sympathetic stimulation that raises systemic and pulmonary vascular resistance and increases blood pressure. If hypercarbia is not cleared by compensatory ventilation, acidemia develops. From this, direct myocardial contractility depression and decreased cardiac output can follow (Ho, 1995; Reynolds, 2003; Sharma, 1996). Hypercarbia can also lead to tachycardia and arrhythmia. Less commonly, bradycardia can stem from vagal stimulation. This may follow pelvic organ manipulation, cervical stretching during uterine manipulator placement, or peritoneal stretching during pneumoperitoneum creation.
Insufflation of any gas elevates intraabdominal pressure. This increased pressure decreases flow in the inferior vena cava, causes blood pooling in the legs, and raises venous resistance. In sum, venous return to the heart is decreased, and thereby cardiac output is lowered. Increased intraabdominal pressure can also directly lower splanchnic blood flow.
Intraoperative pulmonary function may be challenged during laparoscopy. First, the diaphragm is displaced upward by intraabdominal pressure from the pneumoperitoneum. This can be accentuated by organs also being pushed cephalad against the diaphragm during Trendelenburg positioning. Moreover, insufflation pressures stiffen the diaphragm and chest wall. Together, these alterations lead to higher required airway pressures to achieve adequate mechanical ventilation. Also, as the diaphragm moves up, lung volume and functional residual capacity are diminished, which in turn reduces the reserve volume for oxygenation. Moreover, this lung volume decline favors a tendency for the lung to collapse, leading to atelectasis. This can create ventilation and perfusion mismatching and an increased alveolar-arterial oxygen gradient. In sum, all of these factors favor poorer oxygenation.
Urinary output commonly is diminished during laparoscopy. This may result from the lowered cardiac output, decreased splanchnic blood flow, direct renal parenchymal compression, or the release of renin, aldosterone, or antidiuretic hormone. Together, these lessen renal blood flow, reduce glomerular filtration rate, and diminish urine output. Importantly, renal function returns to normal following pneumoperitoneum decompression (Demyttenaere, 2007).
Several coexistent medical disorders are particularly relevant when considering laparoscopy. These include cardiac and pulmonary disease, intestinal obstruction, hemoperitoneum and hemodynamic instability, and pregnancy. As just described, in those with severe cardiac or pulmonary disease, elevated intraabdominal pressures and steep Trendelenburg positioning may not be tolerated, as they decrease venous return and pulmonary reserve. Unfortunately, with laparoscopy, these techniques are often required for adequate visualization and instrument manipulation. In addition, CO2 is used to distend the abdomen during laparoscopy. As noted, it is absorbed across the peritoneum into circulation, and hypercarbia may follow. Accordingly, in those with pulmonary or cardiovascular limitations, lowering intraabdominal pressures and flattening the degree of Trendelenburg are advantageous.
For a clinically stable patient with hemoperitoneum, laparoscopy is not contraindicated. Thus, ruptured ectopic pregnancies or a ruptured bleeding ovarian cyst may be treated via MIS. Although an unstable patient was previously considered a contraindication to laparoscopic surgery, many skilled surgeons feel they can safely and quickly enter the abdomen laparoscopically. That said, the lowered venous return and cardiac output must be factored into the decision to select laparoscopy for such patients.
Concurrent intestinal obstruction and its associated bowel distention may increase risks for bowel injury during abdominal entry. In these situations, open entry to gain initial abdominal access may be beneficial. However, ischemic bowel may be poorly served by pneumoperitoneum-related diminished splanchnic blood flow.
In the past, obesity had been considered a relative contraindication for gynecologic laparoscopy. First, adequate ventilation may be difficult. In general, obese patients display reduced lung compliance that is proportional to their body mass index (BMI). Moreover, abdominal wall adiposity lowers abdominal wall compliance, which in turn elevates the pneumoperitoneum pressure required for surgery. Also, fattier omentum and mesenteric fat add to the bulk forced against the diaphragm in Trendelenburg position. Other limitations include a thick subcutaneous layer that encumbers laparoscopic instrument motion. It can also hinder abdominal entry, and trocar tunneling during insertion is common. Just patient girth relative to surgeon arm length may limit instrument manipulation.
As possible fixes, placement of an extra ancillary port for adequate manipulation of omentum and bowel out of the operative field can be helpful. Coordination with the anesthesia team to find a comfortable degree of Trendelenburg for both successful operative manipulations and adequate ventilation is essential. Longer “bariatric” instruments can overcome many length limitations.
As a result, with a skilled surgeon, obese patients may actually benefit from MIS. In studies, healthy obese patients experience less pain, quicker recovery, and fewer postoperative complications such as wound infections and postoperative ileus after laparoscopy compared with laparotomy (Eltabbakh, 1999, 2000; Scribner, 2002). That said, certain operative parameters may be adversely affected in obese patients undergoing laparoscopy compared with normal-weight patients. Higher conversion rates to laparotomy, longer operating times, and longer hospitalizations have been noted (Chopin, 2009; Heinberg, 2004; Thomas, 2006). However, this has not been found by all investigators, and overall outcomes may be superior to an open abdominal approach (Camanni, 2010; O’Hanlan, 2003; Shah, 2015).
Nonurgent conditions identified during pregnancy may often be delayed and addressed postpartum. However, laparoscopy may be performed during any trimester. Thus, familiarity with the superimposed physiologic changes of pregnancy can improve maternal and fetal safety (O’Rourke, 2006; Reynolds, 2003).
Perioperatively, a wedge can be placed beneath the mother’s back on the right to create a left-lateral tilt and displace the uterus. For second- or third-trimester pregnancies, this can minimize the decreased venous return that results from pneumoperitoneum and from an enlarged uterus compressing pelvic veins and inferior vena cava. Also, rates of venous thromboembolism (VTE) are increased during pregnancy due to gestational hypercoagulability. Placing sequential compression stockings can help lower this risk.
Intraoperatively, steps involve avoiding placement of intracervical uterine manipulators, limiting insufflation pressures to 10 to 15 mm Hg, maintaining maternal end-tidal CO2 levels between 32 and 34 mm Hg, moving trocar placement appropriately cephalad to avoid puncture of the gravid uterus, and limiting uterine manipulation (Pearl, 2011). Of note, the routine use of perioperative prophylactic tocolytics is not recommended in these cases. However, pre- and postoperative fetal heart rate assessment and contraction monitoring for more advanced gestations are typically implemented.
For adnexal masses, myomectomy, and supracervical hysterectomy, operative planning must address appropriate specimen removal. As discussed later, options include endoscopic bags, morcellation, colpotomy, or minilaparotomy incisions. To guide selection, specimen size and the risks for occult malignancy and abdominal tumor seeding are assessed. Importantly, for masses that are known or strongly suspected to be malignant, laparoscopy is avoided if patient outcome could be compromised by specimen rupture, seeding, or morcellation or by incomplete resection or staging.
In addition to patient factors, a surgeon must also consider environmental factors. The availability of appropriate anesthesia care, surgical nursing, support staff, and proper instrumentation influences procedure selection. Advanced operative laparoscopy is a coordinated team effort that requires multiple simultaneous activities, overseen and directed by the surgeon.
PATIENT PREPARATION
Randomized clinical trials have demonstrated that prophylactic antibiotics significantly reduce postoperative infectious morbidity rates following abdominal or vaginal hysterectomy. During laparoscopic hysterectomy, the vagina is similarly opened. Thus, preoperative antibiotics are recommended, and selection can be aided by American College of Obstetricians and Gynecologists guidelines (2014) found in Table 39-6. Antibiotics are generally given at the induction of anesthesia. For other types of laparoscopic procedures, data do not support antibiotic prophylaxis for clean surgical cases, that is, those that do not enter the vagina, bowel, or urinary tract (Chap. 3).
For thromboprophylaxis, the same principles used for other abdominal surgeries are applied to laparoscopic cases (American College of Obstetricians and Gynecologists, 2013). Specific to laparoscopy, pneumoperitoneum pressure may decrease venous return from the lower extremities (Caprini, 1994; Ido, 1995). Thus, for those in whom VTE prophylaxis is planned, preventative measures are administered early and prior to anesthesia induction. A complete list of VTE prophylaxis and guidelines for its use can be found in Table 39-8.
The benefits of routine mechanical bowel preparation are debatable, and thus plans for bowel preparation are individualized (Chap. 39). If the risk of bowel injury and stool spillage is increased because of pelvic adhesions or advanced endometriosis, then bowel preparation may limit fecal contamination at the surgical site. Moreover, if proctosigmoidoscopy is planned, an appropriate bowel preparation allows adequate visualization.
Laparoscopy can be completed using general or regional anesthesia. In most cases, general anesthesia with endotracheal intubation is selected to provide: (1) adequate patient comfort, (2) controlled ventilation to correct hypercarbia, (3) muscle relaxation, (4) airway protection from regurgitation due to increased intraabdominal pressures, and (5) orogastric tube placement. Some studies suggest that injection of local anesthesia at port sites may diminish postoperative pain (Einarsson, 2004).
Laparoscopy itself is usually associated with little associated morbidity. Of major complications, the most common is organ injury caused by puncture or by electrosurgical tools and is described later. If these occur or if surgery is hindered by bleeding or adhesions, conversion to laparotomy may be necessary. Overall, this risk of conversion is low, and logically, rates decline as surgeon experience accrues.
Minor complications of laparoscopy occur more frequently. These may include wound infection or hematoma, subcutaneous emphysema from CO2 infiltration, vulvar edema, and postoperative peritoneal irritation from retained intraabdominal CO2. Irritation stems from conversion of CO2 to carbonic acid, which can be a direct irritant.
Because sharp tools are used during laparoscopic entry, vessels and abdominal organs may be punctured. Risk factors have been identified and include intraabdominal adhesions, insufficient gastric emptying, full bladder, insufficient pneumoperitoneum, poor muscle relaxation, thin patient habitus, and unsuitable angle or force of tool insertion. As discussed later, several authors advocate an open entry method as a means to help lower puncture injury rates (Catarci, 2001; Hasson, 2000; Long, 2008).
The organ most frequently injured during laparoscopy is bowel, and rates of 0.6 and 1.6 per 1000 cases are reported (Chapron, 1999; Harkki-Siren, 1997). Women with previous laparotomy have a higher incidence of abdominal adhesions and are at greatest risk for this complication.
Unfortunately, bowel injury sustained during laparoscopy is often missed intraoperatively. For example, in an observational study by Chandler and coworkers (2001), nearly 50 percent of both small- and large-bowel injuries were unrecognized for 24 hours or longer. Typically, these patients present with fever, abdominal pain, nausea, and vomiting within 48 hours of surgery (Li, 1997).
In laparoscopic cases, decompression of the stomach with an orogastric tube prior to obtaining laparoscopic access can lower the stomach puncture risk. Moreover, in those with suspected abdominal adhesive disease, several preventative steps can help avoid bowel injury. These include: (1) introduction of a microlaparoscope to scout for adhesions, (2) preoperative sonography using the visceral slide test to exclude bowel adhered to the anterior abdominal wall, and (3) an alternative site for primary trocar entry, for example in the left hypochondrium (Palmer point), rather than at the umbilicus.
Bladder puncture is uncommon with laparoscopy. Bladder decompression prior to and during surgery and careful placement of secondary trocars under direct visualization will prevent many injuries. However, with increased rates of laparoscopic hysterectomy, rates of bladder and ureteral damage have concurrently risen. These occur at the same surgical steps associated with urinary tract injury during abdominal hysterectomy.
Major vascular injury associated with laparoscopy is rare and typically results during primary trocar insertion. Puncture rates are cited as 0.09 to 5 per 1000 cases, and characteristically, the terminal aorta, inferior vena cava, and iliac vessels, particularly the right common iliac artery, may be injured (Bergqvist, 1987; Catarci, 2001; Nordestgaard, 1995). Rarely, air embolism from gas insufflation following vessel puncture may occur.
Although infrequent, a significant number of deaths result from large vessel injury (Baadsgaard, 1989; Munro, 2002). Prevention may include use of the open entry technique or awareness of the angle and force of trocar entry. Despite these steps, if a large vessel is punctured, the wounding instrument is not removed because it may act as a vascular plug. Moreover, this tool is held stable to avoid extending the laceration. In most cases, laparotomy, direct manual pressure on the vessel, steps for hemodynamic resuscitation, and notification of a vascular surgeon should follow expeditiously.
In contrast, if the inferior epigastric artery is injured, several simple techniques can control hemorrhage. First, bipolar electrosurgical coagulation of the bleeding site may suffice in many cases. If this fails to control bleeding, a 14F Foley catheter can be threaded through the cannula of the wounding trocar or through the defect created by this trocar. The Foley balloon then is inflated and pulled upward to create direct pressure against the posterior surface of the anterior abdominal wall. At the skin surface, a Kelly clamp is placed perpendicular across the Foley catheter and parallel to the skin to hold the balloon firmly in place. The balloon and catheter can be removed approximately 12 hours later. Alternatively, sutures can be placed that traverse the skin, abdominal wall, and peritoneum; arch under the bleeding vessel; and exit the abdomen to directly ligate the vessel (Fig. 41-1). Similarly, the Carter-Thomason tool can be used to ligate both ends of this vessel.
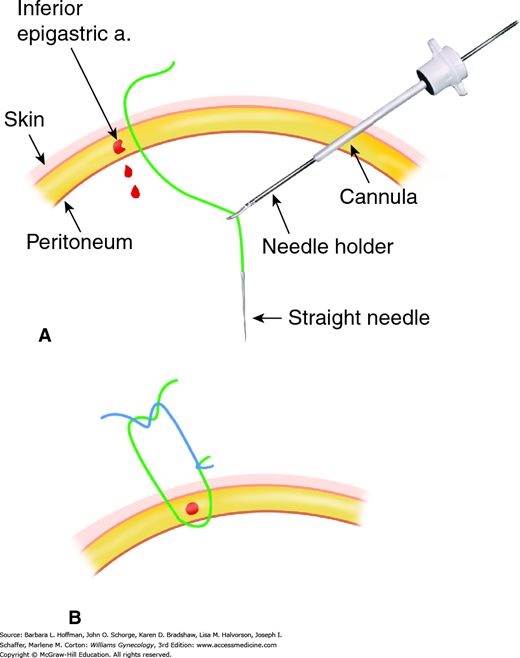
FIGURE 41-1
Ligation of lacerated inferior epigastric artery. A. Suture with an attached straight Keith needle is driven through the anterior abdominal wall lateral and caudal to the bleeding artery. This is performed using direct laparoscopic visualization to avoid organ injury. A laparoscopic needle driver regrasps the needle. B. The needle is then driven upward and through the anterior abdominal wall on the other side of the vessel. The suture loop is tied. This process is repeated cephalad to the bleeding vessel. This places sutures proximal and distal to the site of vessel laceration.
Nerve injury can follow in patients placed for extended periods in the dorsal lithotomy position with arms abducted. From this, injury to the common peroneal, femoral, lateral femoral cutaneous, obturator, sciatic, and ulnar nerves and to the brachial plexus is possible (Barnett, 2007). Specific injuries and prevention are described in Chapter 40. Attention paid to patient position and surgery duration prevent many of these complications.
Accidental burns may follow direct instrument contact or stray electric current. Fortunately, the risk of this complication is low. Prevention steps include keeping instrument tips within the visual field when electric current is applied, strict instrument maintenance to identify insulation defects, employment of bipolar coagulation or harmonic energy for hemostasis when feasible, and use of lower-voltage (cutting) current whenever possible to reduce the applied voltage (Wu, 2000).
Incisional hernias are a potential long-term consequence of laparoscopy. The incidence approximates 1 percent but may rise in the future with increased use of larger trocars for operative laparoscopy and single-port umbilical techniques. Approximately one fourth of hernias are umbilical, and the remainder develop at secondary trocar sites (Lajer, 1997).
A major risk for incisional hernia is use of large trocars measuring ≥10 mm in diameter or port sites from which larger specimens are extracted. Preventatively, smaller trocar use when possible and fascial closure of larger trocars wound sites is advocated. The use of trocars with conical rather than pyramidal tips can also lower this incidence (Leibl, 1999). Finally, peritoneal tissue is ideally not drawn into the superficial layers of the wound when removing the cannulas (Boughey, 2003; Montz, 1994).
Rates of trocar-site cancer metastasis are low, and this complicates the clinical course of approximately 1 percent of patients in whom gynecologic malignancy is identified. Similarly, port-site seeding of other tissues such as endometriosis has been reported. Metastases are more frequent with ovarian cancer than other malignancies, and higher rates are seen with more advanced disease (Abu-Rustum, 2004; Childers, 1994; Zivanovic, 2008). Although most trocar-site metastases are associated with advanced stages of disease, metastasis has followed surgery for tumors of low malignant potential. As a result, the steps of laparoscopy itself have been evaluated as a risk for tumor spread to the trocar sites (Ramirez, 2004). Currently, no evidence-based consensus addresses prevention of this complication. Thus, the careful tissue extraction techniques described on page 896 are encouraged.
OPERATING ROOM ORGANIZATION
In laparoscopy, tool movement is limited compared with laparotomy, secondary to instrument angle restrictions and fixed ports (Berguer, 2001). Thus, room organization is essential, and equipment is positioned before the procedure begins. Also preoperatively, all instruments are checked and tested to confirm proper functioning.
Although equipment positioning may vary based on surgeon preference, the following is suggested to optimize efficiency and safety. The operating room table is centered in the room, and surgical lights lie directly above the operative field. Prior to surgery, this bed is checked to ensure it moves up and down and into steep Trendelenburg position. Obese patients may require a larger bariatric operating table.
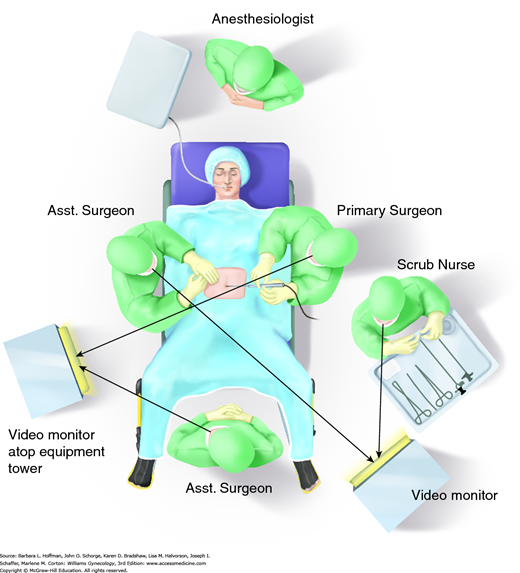
Video monitors may be fixed to the ceiling with articulating arms or may be placed on portable stands. One monitor may suffice for simple procedures, however, two monitors provide easy viewing by the surgeon and assistant. When operating in the pelvis, the monitor is placed directly in front of the surgeon, and the surgeon, forearm-instrument axis, and video monitor are aligned in a straight line. Thus, placement of the video monitor for most gynecologic surgeries is near the patient’s upper thigh (Fig. 41-2). For best surgeon ergonomics, monitor height is 10 to 20 degrees below eye level to prevent neck strain (van Det, 2009). Also, surgeons stand an appropriate distance and height relative to the operating table such that their arms are slightly abducted, their shoulders are inwardly rotated, and their elbows are extended from 90 to 120 degrees. This positioning can minimize surgeon fatigue. The scrub technician and Mayo stand generally are positioned on the side of the primary surgeon near the patient’s leg. Here, instruments can be easily passed to both surgeons. The Mayo stand is organized with frequently used handheld instruments.
A dedicated cabinet or “tower” houses the laparoscopic light source, gas insufflator, and image capture equipment. The tower is positioned on the side opposite the primary surgeon such that he or she has an unobstructed view of equipment display panels. All insufflation tubing, camera, and light cords ideally exit the operating field from the same direction and connect to the equipment tower. Similarly, electrosurgical equipment and pedals are organized so that all these cords are aligned in one direction to reach a separate cart that houses these electrosurgical units. Pedals are oriented appropriately for the primary surgeon to comfortably reach without adjusting his body or moving his eyes from the monitor.
This is another essential component of safe laparoscopy. Following anesthesia induction, a patient is placed in low dorsal lithotomy position with the legs in booted support stirrups (see Fig. 41-2). To aid proper leg positioning, the stirrup brackets, which holster the stirrups, are attached to the table at the level of the patient hips. To prevent femoral nerve injury, the hips are positioned without sharp flexion or marked abduction or external hip rotation. The knees are not flexed more than 90 degrees and are appropriately positioned and padded to avoid common peroneal nerve compression. To avert slipping when in steep Trendelenburg position and to minimize lower back pressure, a patient can be placed directly on an antiskid material such as egg-crate or gel pad. With these, patient skin directly contacts the padding (Klauschie, 2010; Lamvu, 2004). If uterine manipulation is needed, the buttocks are placed slightly past the edge of the table.
Patient arms are tucked to the side in military position. This allows improved patient access and prevents upper extremity hyperextension, which can result in brachial plexus injury. The arms may be tucked using an extended draw sheet, which is placed under the gel pad. This relationship limits arm slippage, which can generate pressure against the brachial plexus. Even in obese patients, the use of antiskid material and arm tucking is useful in preventing slippage for long periods in steep Trendelenburg position (Klauschie, 2010). The arms are padded to avert compression of the ulnar and median nerves. Fingertips are facing the thighs, well-padded, and positioned away from the moving foot of the bed to prevent unintentional amputation. During arm positioning, finger oxygen monitors and intravenous access should not be dislodged.
Shoulder braces are padded brackets that are placed on the cephalic side of the operating room bed and arch around to the patient’s acromion. Their goal is to brace the shoulder and prevent the head from slipping off the bed when in Trendelenburg position. If shoulder braces are required, we recommend tucking the arms in addition to using well-padded braces. However, due to the risk of nerve injury, the use of shoulder braces in general should be limited. Specifically, brachial plexus injury complicates 0.16 percent of gynecologic laparoscopic procedures. When shoulder braces are used, compression over the acromion may apply pressure that stretches the plexus. Moreover, lateral compression by braces may compress the humerus against the plexus. Both predispose to brachial plexus injury (Romanowski, 1993).
LAPAROSCOPIC INSTRUMENTS
Successful laparoscopic surgery relies on the use of appropriate surgical instruments. Most surgeons have designated preferences for certain types of graspers, dissectors, and cutting instruments. Many of these have been adapted and modified for laparoscopic surgery and undergo frequent updates. Moreover, new designs further aid retraction and dissection, thereby increasing the number of procedures that can be performed laparoscopically.
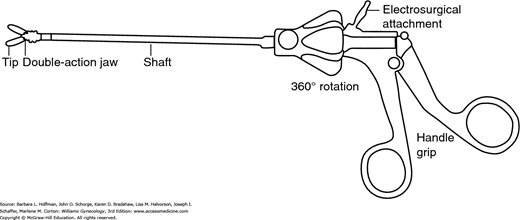
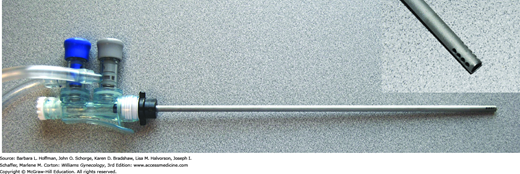
The components of a laparoscopic instrument include the hand grip, shaft, jaw, and tip (Fig. 41-3). In general, an instrument tip’s diameter is concordant with its shaft diameter, and standard sizes fit through 5-mm or 10-mm diameter cannulas. Additionally, 3-mm, 8-mm, and 15-mm instrument diameters are available for many tips. The tip defines instrument function. Jaws may be double action or single action. With a single-action jaw, one tip is fixed, lies in the same axis as the shaft, and offers greater stability during the action performed. Double-action jaws have tips that move synchronously, and this jaw offers a wider angle in which to perform its function. Some jaws are now modified by a compression feature that allows full-length scissor blades to secure the tissue in the tip crux and then cut tissue with greater stability and precision.
Important instrument qualities are comfort and ease of use, which stem primarily from the hand grip shape, the instrument length, and its locking capability. Most laparoscopic instruments have a standard 33-cm length. Due to the popularity of bariatric MIS, extended instruments are now available for procedures in obese patients. Specifically, long Veress needles and trocars and longer instrument shaft lengths offer improved manipulation through a thickened pannus. Although permitting better access, these longer instruments are often more difficult to manipulate due to altered operating angles caused by the extended length.
In the hand grip, a locking feature allows a surgeon to hold tissue without maintaining constant pressure against the grip. This decreases hand fatigue. The ability to rotate an instrument tip 360 degrees is now preferred. This versatility allows access to additional anatomic spaces and decreases the need for uncomfortable surgeon hand or arm rotation.
Many laparoscopic instruments are available in both reusable and disposable forms, each having its own advantages. The main advantage to reusable instruments is lowered expense. Analyses demonstrate that disposable instruments add significant cost compared with reusable ones (Campbell, 2003; Morrison, 2004). The main advantage to disposable instruments is the consistent tool sharpness and avoidance of lost instrument parts. For example, dull scissors may lead to longer operating times and ineffectual surgical technique. Corson and associates (1989) showed that reusable trocars, although sharpened at regular intervals, still required twice the force for entry compared with disposable trocars. As a compromise, modified trocar systems combine the strength of these two features. Namely, the cannula is reusable, whereas a disposable inner trocar offers a consistently sharper tip.
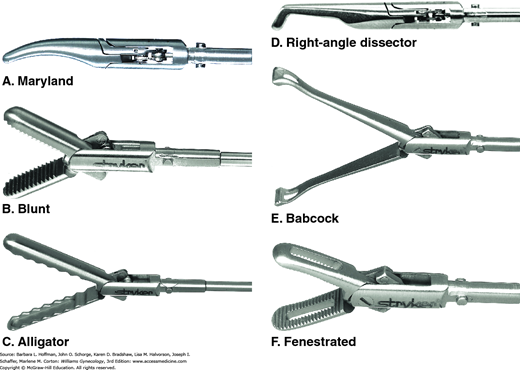
During laparoscopic surgery, abdominopelvic organs may be elevated, retracted, or placed on tension (Fig. 41-4). Most current instrument designs have incorporated safety considerations to minimize organ trauma yet allow effective manipulation. Of these, the blunt probe has an end that is modified to decrease the perforation risk to retracted tissues. It is used for exploration and retraction and is a preferred tool during diagnostic laparoscopy. Most blunt probes are stainless steel and are conductive of electric current. However, disposable probes constructed of nonconductive materials are available.
Graspers are divided into two main categories, atraumatic and those with toothed or serrated tips. Atraumatic graspers are used for exploration, gentle traction, and delicate tissue handing. The 5-mm diameter is a popular size, although 3-mm and 10-mm sizes are available. Most of these graspers have a double-action jaw, and the hand grip is typically nonlocking. Their gradually tapering curved tip permits the surgeon to define and separate tissue planes and is generally preferred for blunt dissection.
The Maryland clamp is an example of a curved blunt tip used for dissection and grasping. It compares to the pean, hemostat, or munion, which are used in open surgery. Additionally, it can double as a needle driver if needed. Although technically considered atraumatic, this clamp may crush delicate tissues such as the fallopian tube or bowel.
The alligator clamp is a blunt grasper with a long, wide tip that handles delicate tissues with minimal crush-injury risk. It is useful for manipulating bowel, larger vessels, or reproductive organs or for exploration of vascular compartments that may be easily punctured or lacerated. However, its ability to retract tissues under tension is limited due to its atraumatic characteristics.
The Babcock clamp is another atraumatic tip that handles delicate tissues with minimal crushing. Its surgical role is similar to that in open techniques. However, as with the alligator clamp, its ability to retract or grasp during applied tension is poor due to slippage.
Ideally, all of these clamps are included in a general laparoscopic surgical tray for most laparoscopic procedures. Figure 41-4 shows additional tips with similar characteristics. As seen, some tips have window openings and are described as fenestrated. These are useful for tissue elevation or retraction or for passing sutures during vessel ligation.
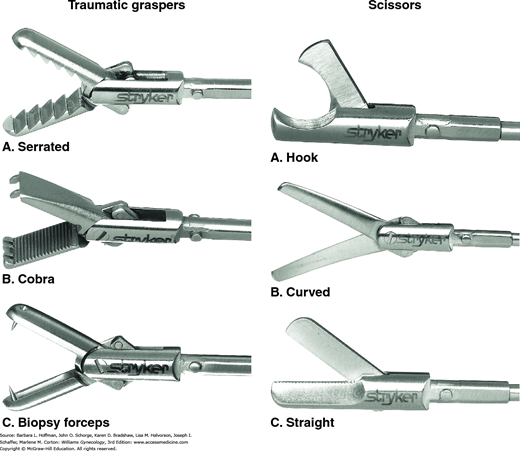
Graspers with tips that are serrated or toothed are used in procedures that involve resection and tissue approximation (Fig. 41-5). Generally, such tissues are placed on tension, and a strong hold is required. In addition, a locking hand grip is typically preferred to keep grasped tissues secured. Most of these instruments have double-action jaws to allow a wide tissue purchase. In situations in which greater grip and tension strength is required, however, a tip with a single-action jaw and locking hand grip may be preferred.
Toothed graspers have teeth at their tip’s end. These are superior for tissue manipulation but function poorly as graspers for sutures or needles. One example is the laparoscopic tenaculum. Single-tooth and double-tooth tenaculums are both available and effectively hold and retract dense, heavy tissue. The single-tooth tenaculum usually has a double-action jaw, whereas the double-tooth tenaculum is available with either a single- or double-action jaw. Both usually offer a locking hand grip. A tenaculum is traumatic and thus is generally used only on tissue to be resected or repaired. One common use is to grasp and remove tissue during morcellation.
The cobra grasper is a toothed instrument with a double-action jaw. It has short teeth on each side and is excellent for tissue retraction due to its strong grip strength. It is considered a traumatic grasper and is not used on delicate tissues.
Some of the toothed instruments are designed with less traumatic teeth and are selected when less tissue crushing is desired. For example, ovarian biopsy forceps provide adequate grasp with minimal tissue crushing. An appropriate setting might be ovarian cyst resection and subsequent ovarian repair. An Allis grasper has blunter teeth for grasping and holding tissue during resection. However, it provides less gripping strength than the cobra.
Serrated graspers are considered traumatic but are less damaging than toothed graspers. They offer a secure grip with minimal tissue damage and generally are used in repairs or tissue approximation. Because of their variety, a surgeon should be familiar with their grips and tissue effects to select the one that best fits the planned procedure. Serrated graspers may be fenestrated or nonfenestrated, may offer a locking hand grip, and may have single-action or double-action jaws.
A corkscrew tip probe is frequently used for marked retraction of more solid masses such as leiomyomas. It offers superior grip and strength but is limited by the trauma created as it is screwed into the tissue to be held. Additionally, surgeons are mindful of the tip location when advancing it, as the downward force required to spiral the corkscrew tip may inadvertently perforate adjacent tissues. Despite this risk, this tool can be invaluable when manipulating solid, bulky leiomyomas or uteri.
Newer, small, 2-mm and 3-mm accessory manipulators have a trocar built around the instrument shaft. These can be placed percutaneously to augment surgical manipulation yet leave only a tiny residual abdominal wall scar. Of the two available designs, one is fully disposable and the other is reusable.
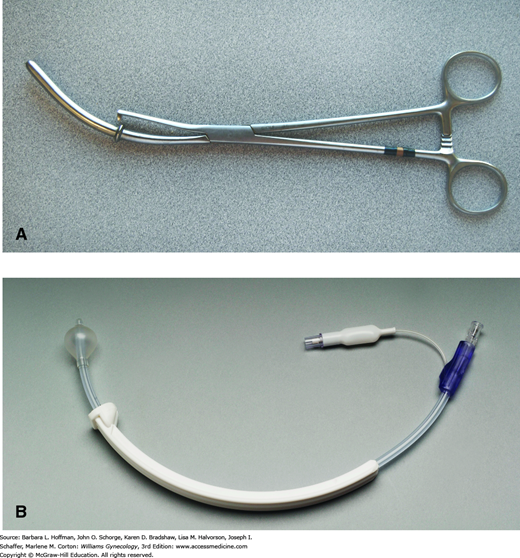
These devices were originally designed to offer manipulation of the uterus to create tension, expand operating space, or improve access to specific parts of the pelvis. The Hulka and the Sargis uterine manipulators are reusable stainless steel instruments that contain the following: a stiff blunt tip for insertion into the endocervical canal, a toothed tip that affixes to the cervical lip for stabilization, and a handle for vaginal placement (Fig. 41-6). For these manipulators, the cervix should to be patent to allow entry into the lower uterine cavity.
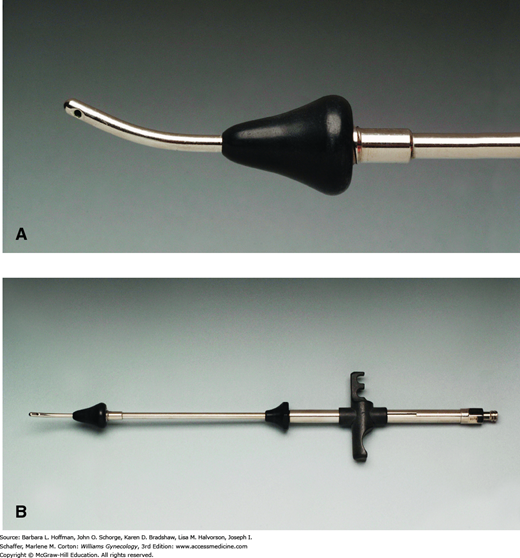
Uterine manipulators have become increasingly versatile and offer additional functions. The Cohen cannula manipulator has a hard-rubber conical tip with a patent cannula for dye injection into the uterus, such as with chromotubation (Fig. 41-7). For placement, a single-tooth tenaculum is placed on the anterior cervical lip. The manipulator’s conical tip wedges firmly against the cervix and thereby minimizes retrograde dye egress back through the os. The distal end of the Cohen manipulator then articulates with the crossbar that extends between the tenaculum’s finger rings. Although commonly used, its range of motion is hindered by its straight shaft. Thus, the ability to dramatically flex a uterus anteriorly or posteriorly may be limited. The Rubin cannula manipulator is similar, with the same disadvantages. Greater flexion may be offered by the Hayden and Valtchev uterine manipulators. These have tip options, either conical or longer blunt intrauterine probes, which attach to a wristed joint at the distal end of the instrument shaft. This joint permits improved anteflexion and retroflexion. All of the manipulators just described affix to the cervical lip for stability. Thus, the risk of cervical trauma, although usually minimal, is disadvantageous.
FIGURE 41-7
Cohen cannula. This device is used in conjunction with a separate tenaculum. The tenaculum is placed horizontally on the anterior cervical lip. A. The narrow cephalad tip of the cannula fits into the endocervical canal. The conical head abuts the external cervical os and limits insertion into the endometrial cavity. B. The caudad portion contains a crossbar into which the ratcheted handle of the cervical tenaculum fits.
Disposable uterine manipulators such as the Harris-Kronner Uterine Manipulator Injector (HUMI) or the Zinnati Uterine Manipulator Injector (ZUMI) also have a cannula for introducing dye to assess uterine and tubal patency (see Fig. 41-6). Rather than affixing to the cervix, an intracavitary balloon at the manipulator’s uterine end is expanded similar to a Foley balloon once the manipulator is placed. This prevents the device from dislodging. Due to the length and firmness of the material used, these devices are advantageous for oversized uteri.
At times, a vaginal sponge stick is a practical manipulator for elevation and identification of pelvic structures. This may be selected by an advanced surgeon who wishes to eliminate the manipulator or chosen in cases in which the uterine fundus is absent. Last, newer manipulator designs have emerged to complement laparoscopic hysterectomy and are illustrated in Chapter 44.
These are integral to most laparoscopic procedures and are available in reusable and disposable models. Scissor tips vary depending on the type of dissection or resection needed (see Fig. 41-5). Scissors preferred for dissection commonly have a curved, somewhat blunted, tip that tapers similar to Metzenbaum scissors. This shape allows a surgeon to use standard techniques for tissue separation and resection with minimal trauma to the surrounding tissues (Chap. 40). These curved blades may be smooth or slightly serrated. A serrated edge tends to hold tissue and minimize slippage prior to cutting. A smooth blade is preferred for sharp dissection, such as with adhesiolysis.
Straight scissors also come with smooth or serrated blades. They are used more for cutting and are less desired for dissection. Many straight scissors are designed with a single-action jaw, and some surgeons feel this offers better control.
Hooked scissors have a rounded, blunt tip and hooked blades. When initially approximated, the blades close around the tissue without cutting and then cut from the tip toward the hinge. This offers a controlled transection and is useful for partial transection of tissues. Moreover, its design allows a surgeon to confirm optimum placement before cutting. This type of scissors is commonly used for suture cutting.
Successful laparoscopy requires a clear visual field. Thus, an effective and efficient suction and irrigation system is integral to procedures that require fluid or smoke removal (Fig. 41-8). Older systems were extremely slow and thereby prolonged operative time or failed to adequately clear a field with brisk bleeding. Newer motorized systems provide faster irrigation and evacuation, and motors usually have two speeds, which can be manually adjusted. The suction tips are available in 3-, 5-, and 10-mm diameters, thereby tailoring instrument capability to the clinical setting. The latest generation systems also permit additional instruments to be placed through the hollow suction tip for concurrent monopolar electrosurgery. Newer models also have attachments to fluid management systems to monitor infused and extracted volumes.
When using a suction irrigation system, all of the suction holes are ideally submerged in the fluid to be removed. This avoids inadvertent insufflation gas removal, which then collapses the operative field. Additionally, the probe may cause suction damage to viscera, especially delicate structures such as tubal fimbria and bowel epiploica. To avoid damage, suction is used when there is a safe distance from vulnerable structures and with the assistance of another instrument to move these structures away from the suction tip.
These tools cut excised tissues into smaller pieces, which can then be extracted. Available morcellators use either thin cutting blades or pulsatile kinetic energy. Bladed morcellators consist of a hollow large-bore shaft that contains razorlike blades to shave tissues into thin strips. One of these, the Storz Rotocut, is reusable but houses disposable stainless steel blades that are efficient in cutting through dense masses. Although bulkier and heavier than others, it is among the fastest and most effective. The Lina Morcellator has a built-in battery pack, is slower but more ergonomic, and is disposable. The MOREsolution morcellator offers a 2-cm-diameter blade, which is currently the largest and may be helpful for large masses. Another device, the Gynecare Morcellex, is currently unavailable due to a voluntary suspension of worldwide sales. Each mechanical morcellator has its advantages, and familiarity with these allows selection of the most suitable instrument for a given tissue.
Another morcellator, the PKS PlasmaSORD Bipolar Morcellator, is bladeless. Instead, it uses plasma kinetic energy, which is a form of pulsatile bipolar energy. It works well for hysterectomy and myomectomy specimen morcellation. However, it produces a large smoke plume, which reduces visibility and thereby increases operative time. Accordingly, cases with larger specimens may have extended operative times with this instrument compared with bladed instruments. However, no randomized studies support the superiority of one morcellator over another.
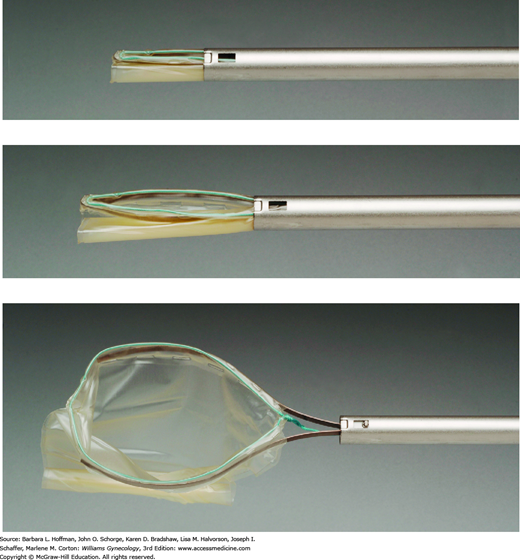
Endoscopic bags for tissue retrieval vary in size and vinyl strength. Some are free-standing sacs designed for manual introduction into the abdominal cavity through cannulas and are preferred for larger and denser masses. Once loaded, the sac is simply lifted through an appropriately sized abdominal wall incision.
Other types are manufactured as pouches attached to support arms at the end of a laparoscopic shaft to create a self-contained unit. As shown in Figure 41-9, the support arms open the sac. Once the mass is bagged, the arms and pouch are retracted and removed through the cannula. The cannula is then removed, bringing the bag to the incision where it is extracted. With either sac type, if a specimen does not compress or cannot be drained, the incision may require enlargement.
Designed to complement MIS, nonmetal self-retaining retractors consist of two equal-sized plastic rings connected by a cylindrical plastic sheath. One ring collapses into a canoe shape that can be threaded through the incision and into the abdomen. Once inside the abdomen, it springs again into its circular form. The second ring remains exteriorized. Between these rings, the plastic sheath spans the thickness of the abdominal wall. To hold the retractor in place, a surgeon everts the exterior ring multiple times until the plastic sheath is tight against the skin and subcutaneous layers. This form creates 360-degree retraction. These disposable retractors maximize incision size because of their circular shape and by eliminating thick metal retractor blades within the wound opening. Brands include the Alexis and Mobius retractors, and available sizes range from extra small to extra large. In some studies, these retractors provide wound protection and lower wound infection rates (Horiuchi, 2007; Reid, 2010).
For MIS cases, these devices offer several functions. First, they retract minilaparotomy incisions to aid large specimen removal. Moreover, certain procedures, such as laparoscopic myomectomy, can also be completed through these incisions (Section 44-8). Second, concern about tissue dissemination has prompted development of retrieval bags that are coupled with these self-retaining retractors. For this, the retrieval bag is initially placed into the abdomen. The bag containing the excised specimen is then brought to the surface and is fanned open outside and around the minilaparatomy incision. The self-retaining circular retractor is then placed into the bag’s interior and simultaneously opened within the incision. This creates a closed environment in which the specimen can be sharply morcellated manually with scissor or knife. Long-term data on safety and efficacy of this enclosed approach are not yet available.
Understanding principles and correct use of electrosurgical instruments is essential to safe laparoscopy. The same principles of electrosurgery in open surgery apply to laparoscopy (Chap. 40). However, special considerations are necessary in a closed, minimally invasive environment. For example, the entire length of an instrument may extend past a surgeon’s visual field, thus risking unintended electrosurgical burns. Fortunately, advances in instrumentation mitigate many of the physical constraints inherent to MIS.
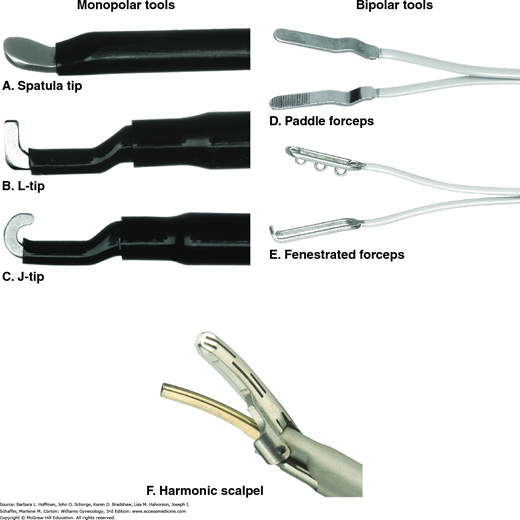
Monopolar instruments may be useful for tissue cutting, dissection, vaporization, and desiccation. Delivery of this energy is usually through scissors or needle point tip. Of these, monopolar scissors coagulate tissues within its jaws prior to incision. This is typically used for thin tissues and small vessels. In addition, closed blade tips can act simultaneously to cut tissue and achieve hemostasis. Monopolar energy delivered though a needle point tip is used for functions ranging from ovarian drilling to development of peritoneal planes during hydrodissection.
Unintended thermal injuries form the main risk with this energy type. With monopolar instruments, insulation failures, direct coupling, or capacitative coupling may each result in unintended, potentially serious electrosurgical burns. First, insulation failures are breaches in an instrument’s insulation. This break provides an alternate pathway for current flow. When a monopolar instrument is activated, electric current may travel from the electrode through the insulation breach and discharge to any tissue in contact with this breach. This current flow may cause thermal damage to surrounding visceral and vascular structures without the surgeon ever being aware. Accordingly, before electrosurgical tools are used, systematic inspection should look for insulation cracks throughout their length, for aberrant or loose cord connections, and for assurance that a grounding pad is correctly placed on the patient.
Another monopolar effect is direct coupling, which occurs when an activated electrode contacts another metal object—either intentionally or unintentionally. This technique is frequently used during open surgery to achieve hemostasis of small vessels, such as when the electrosurgical blade tip is touched to a hemostat around a small vessel. However, in laparoscopy, unintentional direct coupling may occur when a metal instrument or object (such as a metal cannula) contacts an active monopolar instrument and thus provides an alternate and undesired current flow to surrounding viscera.
Another hazard with monopolar instruments is the risk of capacitative coupling. A capacitor is defined as two conductors separated by a nonconducting medium. During laparoscopy, an “inadvertent capacitor” can be created when a conductive active electrode (e.g., monopolar scissors) is surrounded by a nonconducting medium (insulation around the scissors) and is placed through another conductive medium (a metal cannula). This capacitor creates an electrostatic field between the two conductors. When current is activated through one of the conductors, this in turn will induce a current in the second conductor. Capacitative coupling occurs when this system discharges current into other surrounding conductive material. In the case of an all-metal cannula, current can be dissipated throughout the abdominal wall. With hybrid cannula systems, in which a metal cannula is anchored by a plastic sleeve or collar, the capacitor that is created has no place to discharge. Stray current can then exit to adjacent tissue that is in contact with the metal portion of the cannula, thereby damaging nearby vascular or visceral structures. This risk can be reduced by avoiding hybrid cannulas and by selecting bipolar instruments. Moreover, the addition of an integrated shield on the electrode shaft of some monopolar instruments, which monitors for stray current, can prevent this complication.
Bipolar energy is mainly used in laparoscopy for tissue desiccation and hemostasis. Many types of bipolar forceps are available for various uses (Fig. 41-10). The 3-mm paddle forceps are used for tubal coagulation during sterilization procedures. Flat-tip forceps desiccate larger vessels and tissue pedicles. Fine-tip, “microbipolar” forceps aid hemostasis near or on vulnerable structures such as the ureter, bowel, and fallopian tubes. Burns are less of a concern with bipolar energy because the currents used are typically lower. Currents, for the most part, also stay confined between the two closely approximated electrodes.
For hemostasis, energy is delivered to denature collagen and elastin in vessel walls and thus seal the vessel. During this process, the bipolar device uniformly compresses the tissue and provides internal monitoring to adjust energy delivery. When evaluating these devices, important considerations include thermal spread, ability to provide desired tissue effects, consistency of results, time required to achieve results, plume produced, and maximum vessel diameter that can be securely sealed (Lamberton, 2008; Newcomb, 2009).
Currently used advanced bipolar devices such as the LigaSure, Plasmakinetic (PK) Gyrus, and Enseal are multifunctional tools that can be used for both tissue desiccation and dissection. Each of these devices employs a low voltage to deliver energy to tissue and carry impedance feedback to the electrosurgical unit to locally regulate thermal tissue effects. These adaptations allow for reduced collateral injury from thermal spread, an improved tissue seal, less plume production, and diminished tissue sticking. Whereas the LigaSure delivers a continuous bipolar radiofrequency waveform, the PK delivers energy in a pulsed waveform. The Enseal system has a temperature-controlled feedback mechanism at its tip, which “locally” modulates energy delivery.
The Harmonic scalpel, also known as an ultrasonic scalpel, uses ultrasonic energy, which is converted to mechanical energy at the active blade. Seen as the lower blade in Figure 41-10F, the active blade vibrates to deliver high-frequency ultrasonically generated frictional force, whereas the inactive upper arm holds tissues in apposition against the active blade. Alternatively, the active blade may be used alone. Either cutting or coagulating effects can be achieved, and a balance between these two is created by controlling several factors: power levels, tissue tension, blade sharpness, and application time. Higher power level, greater tissue tension, and a sharp blade will lead to cutting. Lower power, decreased tissue tension, and a blunt blade will create slower cutting and greater hemostasis. Limitations of the Harmonic scalpel include limited ability to coagulate vessels larger than 5 mm and the requirement for the surgeon to balance the factors listed above (Bubenik, 2005; Lamberton, 2008).
Lasers were widely used in laparoscopy in the 1980 through 1990s and include the CO2, argon, KTP (potassium titanyl phosphate), the Nd-YAG (neodymium:yttrium-aluminum-garnet) lasers. These are generally used through an operative channel on the laparoscope or via a separate port. These lasers can cut, coagulate, and vaporize tissues and are employed for lysis of adhesions, tubal surgery, and endometriosis fulguration or resection. In the hands of skilled surgeons, lasers offer precision and control with minimal effect on surrounding tissue. Thus, a laser is able to work near or over sensitive structures such as bowel, bladder, ureters, and vessels. Disadvantages are its learning curve, expense, lack of portability, and smoke production.