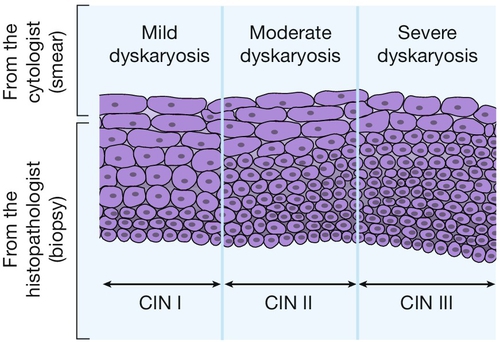
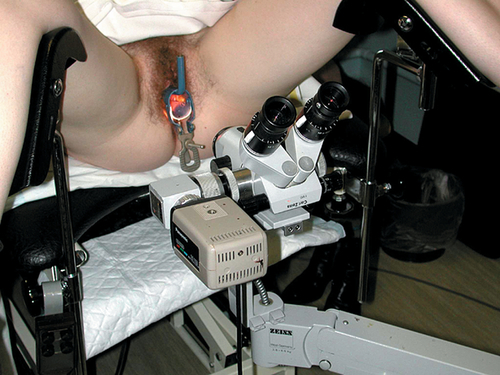
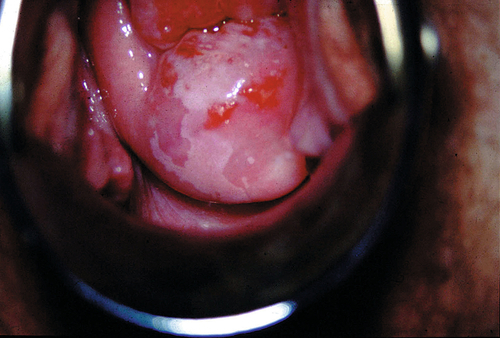
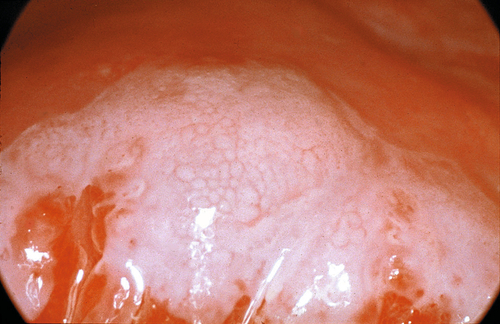
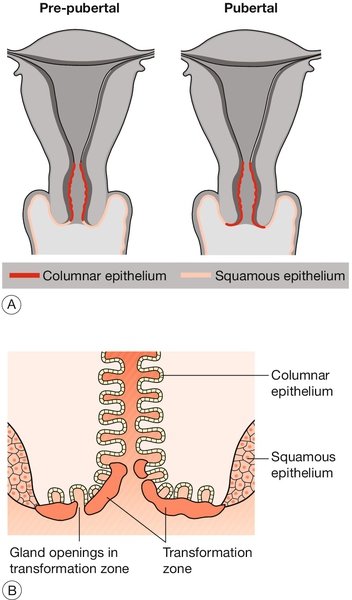
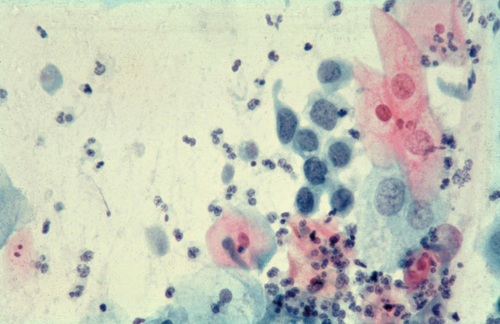
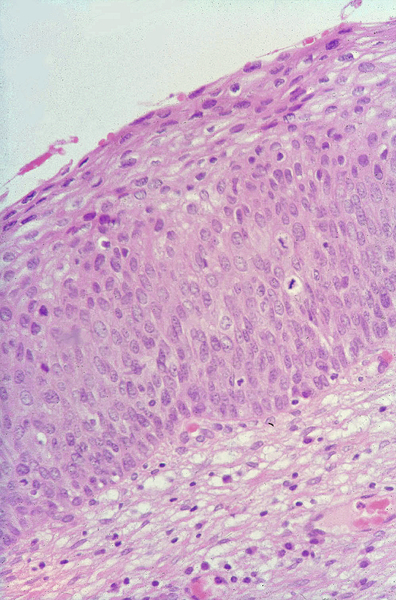
20 Cervical cancer is the most common cancer among women in many developing countries, and worldwide, there are over 450 000 cases each year. The overall lifetime risk is about 5% in parts of Africa, India and Latin America, compared with 1% in Europe and North America. About 3400 cases of cervical cancer are presently diagnosed each year in the UK, and 1300 of these women will die from the disease. In the UK, cervical cancer is relatively uncommon, representing around 2% of female cancers. It is however the most common cancer in young females. Fortunately, cervical cancer has a premalignant phase and many of the criteria for a suitable screening programme are fulfilled. The aim of this screening is to detect premalignant cervical disease by means of a ‘smear test’ and treat the premalignant disease before invasion occurs. Both the incidence and mortality have fallen considerably since the introduction of this screening programme. Cervical intraepithelial neoplasia (CIN) develops in the transformation zone of the cervix. Understanding the transformation zone is the key to understanding cervical cancer screening. The endocervix is lined by columnar epithelium and the ectocervix by squamous epithelium. Under the influence of oestrogen, part of the endocervix everts, thereby exposing the columnar epithelium to the chemical environment of the upper vagina (Fig. 20.1). The change in pH, along with other factors, causes the delicate columnar epithelium cells to transform into squamous epithelium through the process of metaplasia. CIN can develop in this transformation zone and it is this area which is sampled cytologically. Fig. 20.1The transformation zone. (A) The cervix everts at puberty, exposing the columnar epithelium of the endocervical canal. (B) This epithelium, referred to as the transformation zone, gradually undergoes metaplasia to squamous epithelium. Cells shed from the surface may be sampled by a variety of devices, so that cells from both the endocervix and ectocervix can then be examined microscopically for cytological abnormalities. Cellular abnormalities are classified into different degrees of ‘dyskaryosis’. Although dyskaryosis is a cytological diagnosis (Fig. 20.2), the degree of dyskaryosis correlates to some extent, with the degree of cervical intraepithelial neoplasia, which is a histological diagnosis (Figs 20.3 and 20.4). The difference being that cytology looks at individual cells, whereas histology examines the cells as a tissue and therefore has architecture. As well as examining the desquamated cervical cells, cervical smear reports may also identify infection such as candidal, trichomonal or wart virus infection. Rarely, they may identify cells from other parts of the genital tract, such as malignant endometrial or ovarian cells. Fig. 20.2Slide prepared from a cervical smear. There is moderate dysplasia with hyperchromasia, irregular nuclei and multinucleation. This slide also shows Trichomonas vaginalis, leucocytosis and a spermatozoon. Fig. 20.4CIN II in a biopsy specimen. There are abnormal cells arising from the basal layer, but not extending to the full thickness of the epithelium. The precise rates of progression and spontaneous resolution of the disease are unknown. Roughly one-third of lesions will progress to the next stage (CIN I–II, CIN II–III, etc.), a third will remain unchanged and a third will regress. The duration of progression to invasive carcinoma is variable, but the average is perhaps around 10 years. In the UK, there is an organized systematic computerized screening programme with national recommendations to screen from the ages of 20–65 years. Different regions, however, have different protocols, and England has recently recommended screening from the age of 25 years. Significant dyskaryosis on a cervical smear is an indication for further assessment with colposcopy. This is a procedure by which the cervix is examined in more detail using a type of binocular microscope referred to as a ‘colposcope’ (Fig. 20.5). Although moderate and severe dyskaryosis are absolute indications for colposcopy, controversy exists as to whether it is required for mild dyskaryosis. Some believe it is important, while others are concerned it may lead to over-treatment of lesions, which will often regress spontaneously. The indications for colposcopy are listed in Box 20.1. The patient is placed in the lithotomy position and a bivalve speculum is then inserted to allow visualization of the cervix. It is important to identify the squamocolumnar junction (SCJ). Abnormal epithelium, such as CIN, contains an increased amount of protein and lower levels of glycogen than normal epithelium. If acetic acid is applied to the cervix, the protein coagulates and the abnormal cells appear white: ‘aceto-white’ (Fig. 20.6). There may also be a ‘mosaic’ pattern with patches of aceto-white separated by areas of red vessels (Fig. 20.7). Some of the vascular patterns may appear ‘punctated’ if the vessels are viewed end-on. The inter-vessel distance increases with more severe lesions, and bizarre branching with coarse punctation and atypical vessels suggests invasive disease. Lugol’s iodine (Schiller’s iodine) stains glycogen mahogany brown, and the abnormal cells, which have less glycogen and therefore take up less iodine, can also be viewed in this way.
Cervical neoplasia
Introduction
Cervical intraepithelial and cervical cancer screening
Transformation zone
Screening recommendations
Colposcopy
Obgyn Key
Fastest Obstetric, Gynecology and Pediatric Insight Engine