Care of the Newborn With Ichthyosis
ICHTHYOSIS/MENDELIAN DISORDERS OF CORNIFICATION
Clinical Findings
Dermatologic dogma suggests differentiation of Mendelian disorders of cornification (MeDOC) subtypes is difficult in the neonatal period. However, neonates with MeDOC may often be classified into specific clinical groups that can guide initial workup and treatment1:
1. Exuberant vernix (EV): Affected infants are born with a thickened white covering resembling excessive vernix caseosa. They do not have a collodion membrane.
2. Collodion baby (CB): Affected infants are born encased in a taught, clear, shiny membrane of variable thickness. Fissures may develop, and constriction of limbs or digits may occur. Ectropion or eclabium are often noted along with ear abnormalities. Restriction of movement and occasionally breathing may be noted.
3. Harlequin fetus (HF)/Harlequin ichthyosis (HI): Affected infants are born with grossly distorted features caused by thick plate-like scales with deep fissures and pronounced ectropion/eclabium. Movement and breathing may be highly restricted.
4. Ichthyosiform erythroderma (IE): These infants are born as “red, scaly babies” with diffuse erythema and skin peeling.
5. Bullous ichthyosis (BI): Affected infants exhibit blistering of the skin in the newborn period, and the blistering can be diffuse and severe. The ichthyosis may be mild or subtle in the neonatal period but accentuates with time.
6. Other: Some disorders of cornification show few, if any, skin changes in the newborn period. These include the most common form of MeDOC, ichthyosis vulgaris (IV), as well as the second most common form, recessive X-linked ichthyosis (RXLI).
Confirmatory/Baseline Tests
The following are confirmatory/baseline tests (ie, laboratory tests, radiologic examinations, electroencephalography [EEG], etc) for the specific clinical groups:
1. EV: Sensorineural hearing testing (after clearing the auditory canals of keratotic debris) is mandatory in the newborn period. Infants with ichthyosis prematurity syndrome (IPS) may raise concern prior to birth because of abnormal opacity of the amniotic fluid detected on prenatal ultrasound.2 This may occur in other forms of EV but is not as clearly described. In patients with suspected keratitis, ichthyosis, deafness (KID) syndrome, close monitoring for systemic infection is paramount.3 If epidermolytic ichthyosis (EI) is suspected, skin biopsy can be confirmatory.4
2. CB: Baseline lab evaluation is performed to screen for hemoconcentration/electrolyte abnormalities. Follow-up lab frequency is determined by clinical severity and the presence/absence of abnormalities on initial screening.5
3. HF: If intervention is employed, meticulous monitoring for electrolyte abnormalities and systemic infection is paramount.6 Affected infants may be detected with high-resolution ultrasound in the prenatal period.7
4. IE: Close monitoring is needed for electrolyte abnormalities (especially) and infection. There is a high risk of hypernatremic dehydration, especially in conditions such as Netherton syndrome (NS).8
5. BI: Monitor for electrolyte abnormalities/infection. Skin biopsy can be confirmatory in this subtype of MeDOC and can differentiate patients with EI from those with epidermolysis bullosa (EB).9
6. Other: Male infants with RXLI may be detected in the prenatal period because of abnormally low estriol levels on the standard triple-screen test during pregnancy.10
Differential Diagnosis/Diagnostic Algorithm
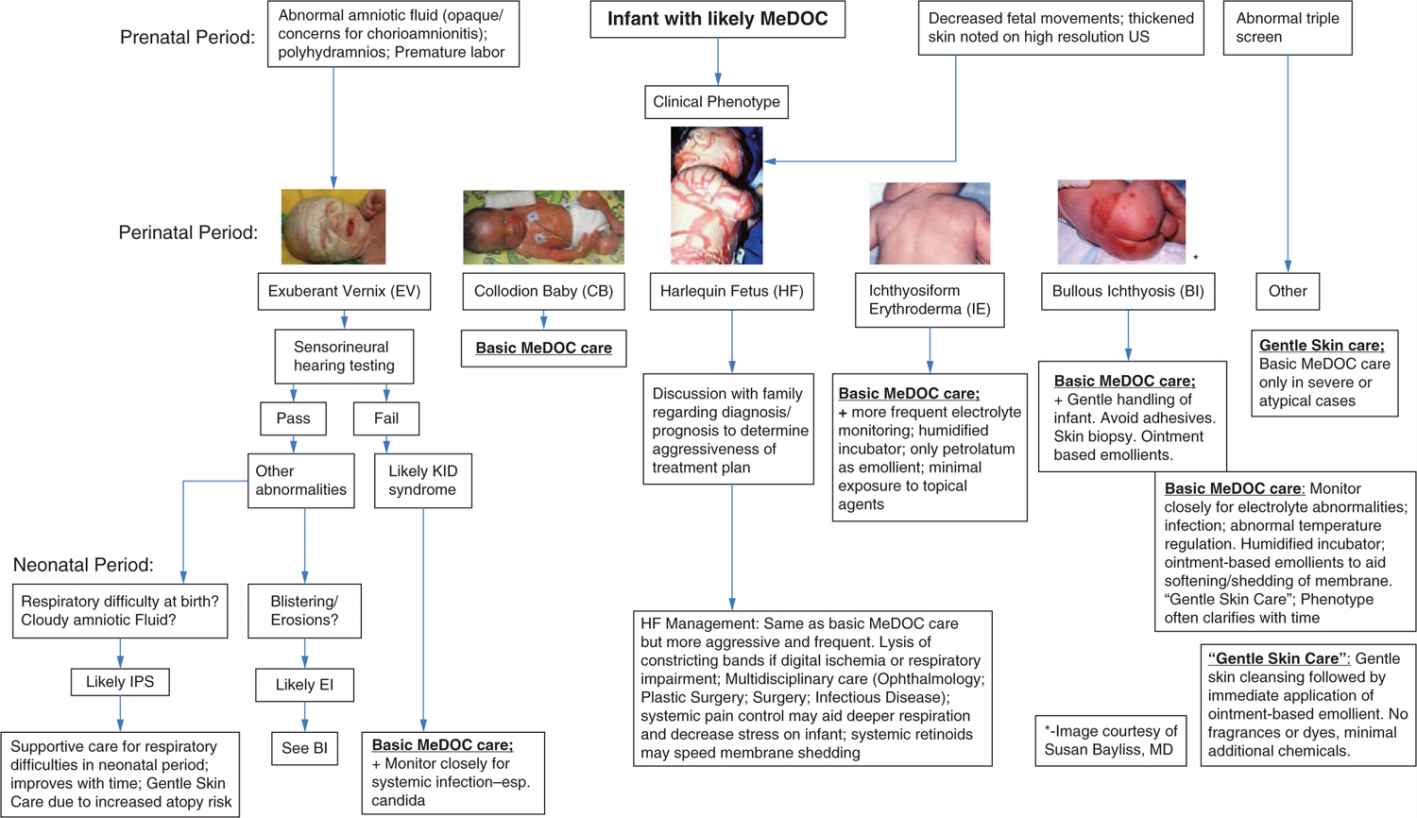
Figure 122-1 provides an algorithm for differential diagnosis.
FIGURE 122-1 Differential diagnosis algorithm. EI, epidermolytic ichthyosis; IPS, ichthyosis prematurity syndrome; KID, keratitis, ichthyosis, deafness; MeDOC, Mendelian disorders of cornification; US, ultrasound.
1. EV: Several forms of MeDOC may present with this phenotype. Congenital deafness favors KID syndrome. Normal hearing in a premature infant with polyhydramnios and abnormal amniotic fluid favors IPS. Patients with ABCA12 mutations as well as those with EI may exhibit this neonatal phenotype. Although not clearly reported in the literature, ichthyosis follicularis-atrichia-photophobia (IFAP) syndrome could present with this phenotype.
2. CB: Numerous forms of MeDOC have been reported presenting as CB in the neonatal period. Most commonly, these are autosomal recessive (AR) MeDOC (see Table 122-1).5
3. HF: The differential is limited. Most are caused by severe truncating mutations in ABCA12. Neu-Laxova syndrome may have a severe phenotype similar to HF but also exhibits a variety of dysmorphic features and is typically lethal in the newborn period. Restrictive dermopathy may resemble HF, but fissuring is typically less.
4. IE: A variety of AR MeDOC may exhibit IE if a full collodion membrane does not develop. NS may exhibit neonatal IE. In addition, congenital reticular ichthyosiform erythroderma (CRIE), peeling skin disease, and males with X-linked recessive (XLR) ectodermal dysplasia can present with IE in the neonatal period.11
5. BI: Neonatal blistering can resemble EB; skin biopsy can aid differentiation.
Table 122-1 Collodion Baby (CB): Differential Diagnosis: