Cyanotic Congenital Heart Disease
BACKGROUND
Epidemiology
Congenital heart defects (CHDs) are the most commonly reported major birth defect. Severe CHDs, the forms requiring early treatment at a cardiac center, have an incidence of approximately 3 per 1000 live births; the majority of these are cyanotic lesions. Although the overall incidence has climbed over the years, perhaps because of improved diagnostic methods such as echocardiography, the incidence of the major cyanotic types has remained fairly stable.
Etiology
The vast majority of CHDs are idiopathic. However, there are many known risk factors and associations.
1. Risk factors include
a. Maternal diabetes;
b. Maternal antihypertensive medications;
c. Maternal retinol/high-dose vitamin A intake;
d. Maternal lithium treatment (increased risk of Ebstein anomaly); and
e. Maternal rubella.
2. Genetic causes are numerous, with more added all the time, including
a. Trisomies;
b. Williams-Beuren syndrome;
c. DiGeorge velocardiofacial syndrome (deletion 22q11);
d. Turner and Noonan syndromes;
e. Alagille syndrome;
f. CHARGE (coloboma, heart defects, choanal atresia, mental retardation,
genitourinary and ear anomalies) association;
g. Costello syndrome; and others.
3. There are syndromes/sequences without known genetic markers, such as VACTERL (vertebral, anal, cardiac, tracheoesophageal, renal, and limb) association.
EVALUATION AND WORKUP
Pathophysiology
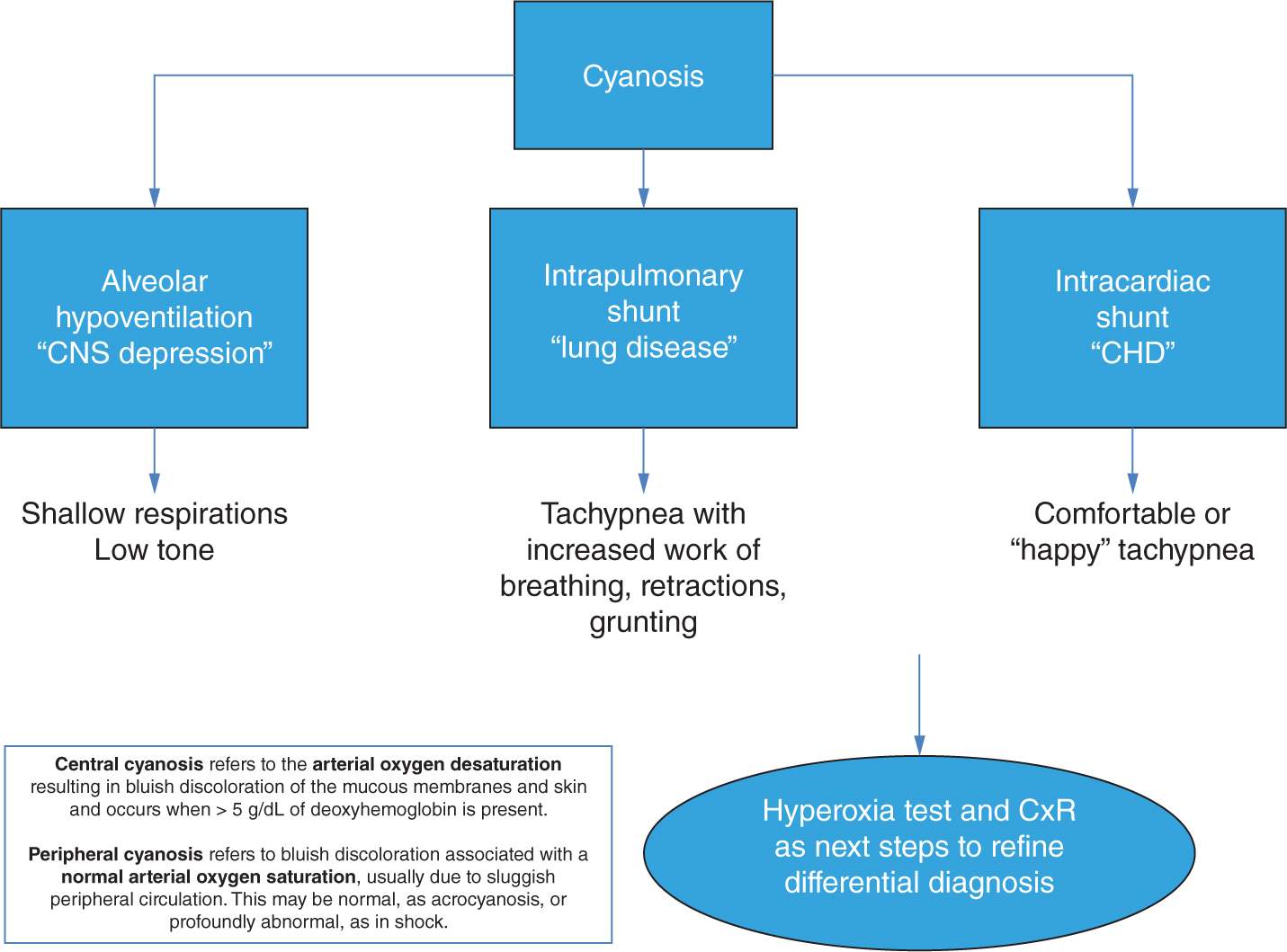
The differential diagnosis of the cyanotic neonate begins with a pathophysiologic question: Is the etiology intrapulmonary shunting, intracardiac shunting, or alveolar hypoventilation (Figure 80-1)?
FIGURE 80-1 Causes of central cyanosis in the neonate. CHD, congenital heart defect; CNS, central nervous system; CxR, chest x-ray.
1. A thorough physical examination (Table 80-1), chest radiograph (Table 80-2), and hyperoxia test can distinguish congenital heart disease from parenchymal lung disease and central nervous system depression as etiologies of central cyanosis (Figure 80-2).
Table 80-1 Physical Exam Pearls for Cyanotic Neonate With Congenital Heart Defect (CHD)
1. Distinguish central vs peripheral cyanosis.
2. The tip of the tongue is a good place to check for central cyanosis; circulation is not sluggish there and not affected by ethnicity.
3. With anemia, central cyanosis will be less prominent, whereas with polycythemia, central cyanosis is apparent at a higher arterial saturation.
4. Differential cyanosis upper vs lower body (examination, pulse oximetry) = right-to-left shunting at patent ductus arteriosus (PDA).
5. Systolic ejection murmur at LUSB suggests obstruction to pulmonary blood flow.
6. Four-extremity blood pressures are essential part of the examination.
Table 80-2 Chest X-ray Pearls for Cyanotic Neonate With Congenital Heart Defect (CHD)