Bubbly Bone Lesion
Christopher G. Anton, MD
DIFFERENTIAL DIAGNOSIS
Common
Nonossifying Fibroma (NOF)
Less Common
Aneurysmal Bone Cyst (ABC)
Unicameral Bone Cyst (UBC)
Fibrous Dysplasia (FD)
Langerhans Cell Histiocytosis (LCH)
Enchondroma
Primary Sarcoma or Metastatic Disease
Rare but Important
Osteoblastoma
Giant Cell Tumor (GCT)
Chondroblastoma
Chondromyxoid Fibroma (CMF)
ESSENTIAL INFORMATION
Helpful Clues for Common Diagnoses
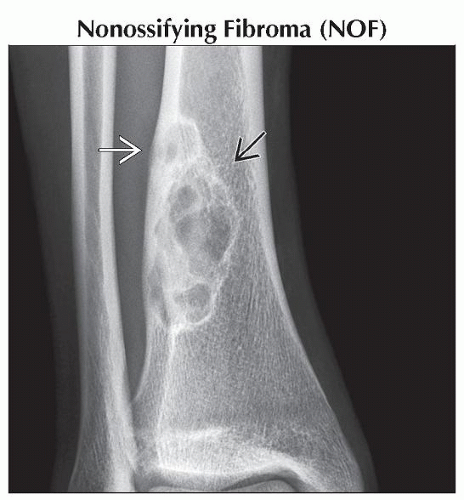
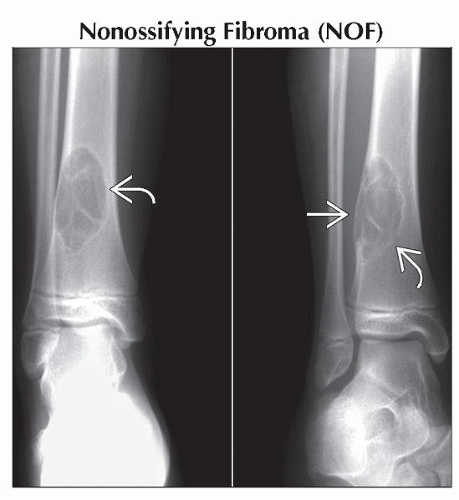
Nonossifying Fibroma (NOF)
a.k.a. fibroxanthoma, fibrous cortical defect (FCD)
Developmental defect, usually discovered as incidental finding on radiograph or MR of knee
Age: 2-20 years
M:F = 2:1; 30-40% of all children
Diametaphyseal of long bones
Femur (38%), tibia (43%), knee (55%), fibula (8%), humerus (5%)
Eccentric, multiloculated, subcortical; no mineralized matrix; cortex may appear absent; scalloped sclerotic margin
Size differentiates FCD and NOF
FCD: < 2 cm, within cortex
NOF: > 2 cm, extends into medullary cavity
T1WI: Hypointense with hypointense rim (sclerotic margin)
T2WI: Low to intermediate intensity with hypointense rim (sclerotic margin)
T1 C+: Enhances
Jaffe-Campanacci syndrome
Café-au-lait lesions, mental retardation, hypogonadism, ocular and cardiovascular abnormalities
Usually asymptomatic and requires no treatment
Most spontaneously regress with time, progressive ossification
Curettage and bone grafting if lesion is > 50% diameter of weight bearing bone; increased risk of pathologic fracture
Helpful Clues for Less Common Diagnoses
Aneurysmal Bone Cyst (ABC)
Not true neoplasm: Intraosseous AVM
Thin-walled, blood-filled cystic cavities
Age: 10-30 years; rare in ≤ 5 years old; slight female predominance
Primary (1°) or secondary (2°) in preexisting lesion in 1/3 of cases
1°: No recognized preexisting lesion
2°: GCT, chondroblastoma, fibrous dysplasia, osteoblastoma, chondromyxoid fibroma, NOF
2°: Osteosarcoma (e.g., telangiectatic variant), chondrosarcoma, malignant fibrous histiocytoma
Typically metaphyseal, most commonly around knee
Tubular long bones (70-80%), lower leg (29%), pelvis (5-10%), clavicle and ribs (5%), spinal posterior elements (16%)
Geographic eccentric expansile lucent lesion ± multiloculated, markedly thinned cortex (may need CT to see) ± periosteal reaction (if fractured)
MR: Characteristic fluid-fluid level (blood products) containing cavities of differing signal intensity; hypointense rim surrounds ABC
Enhancement of cyst walls and septations without enhancing cyst contents, “honeycomb”
Treatment: Curettage and bone grafting with 20% recurrence rate
Unicameral Bone Cyst (UBC)
a.k.a. simple or solitary bone cyst
Age: 10-20 years; ˜ 2/3 present with pathologic fracture
Proximal humerus and femur in up to 80-90%
Central metaphyseal, well defined, lucent, lacks periosteal reaction unless fractured
Hint: Pathognomonic, fallen fragment sign
Pathologic fracture with cortical bone fragment floating dependently with UBC
MR: May contain fluid-fluid level if traumatized; no solid enhancing component
Fibrous Dysplasia (FD)
Age: 5-20 years, peak 10-20 years
Monostotic (70-80%) or polyostotic
Expansile, ground-glass, lucent, sclerotic (skull base lesions), no periosteal reaction, bowing
Associations
McCune-Albright: Female predominance, polyostotic, unilateral FD, precocious puberty, hyperthyroidism, café-au-lait spots
Mazabraud syndrome: Polyostotic FD with intramuscular myxoma, rare
Langerhans Cell Histiocytosis (LCH)
Age: 50% < 10 years
Lytic, sharply demarcated lesion without sclerotic margin unless healing
Skull (50%), axial skeleton (25%), proximal long bones (15%)
Enchondroma
Age: 10-30 years
Lucent, scalloped endosteum; ring and arc calcified matrix
Small bones of hand and wrist; metadiaphysis of long bones
Primary Sarcoma or Metastatic Disease
Telangiectatic osteosarcoma: Radiographically, lytic lesion could look like ABC
Helpful Clues for Rare Diagnoses
Osteoblastoma
Age: 80% < 30 years old
1-10 cm in size, > 1.5 cm osteoblastoma, < 1.5 cm considered osteoid osteoma
Lytic, expansile, sclerotic margin, variable central calcification, radiolucent nidus
Spine (40%), long bones (30%), hands and feet (15%), skull and face (15%)
May present with painful scoliosis
Extensive inflammatory change can mimic malignancy or infection
Giant Cell Tumor (GCT)
Occurs after growth plate closure
Metaepiphyseal, eccentric, lytic, nonsclerotic margin, extends subarticular bone ± periosteal reaction
Long bones (75-90%), around knee (50%)
Pathologic fracture (30%)
Chondroblastoma
Eccentric, epiphyseal, expansile; periosteal reaction in 50%
Immature skeleton
Most commonly around knee and proximal humerus
Long bones (80%), hands and feet (10%)
Thin sclerotic margin with chondroid calcification in 1/3
MR: Solid with no fluid-fluid levels
T1WI: Low to intermediate
T2WI: Intermediate to low with surrounding edema
Chondromyxoid Fibroma (CMF)
Eccentric, lucent with sclerotic margin
Male predominance; CMFs present with pain
Treatment: Curettage, recurrence in 25%
Image Gallery
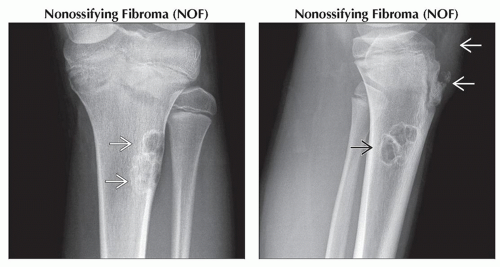 (Left) Anteroposterior radiograph shows an eccentric lucent lesion
 with a thin sclerotic scalloped margin within the proximal lateral aspect of the tibia. NOFs are most commonly seen about the knee. (Right) Lateral radiograph in the same child shows the NOF with a thin sclerotic scalloped margin within the proximal lateral aspect of the tibia. NOFs are most commonly seen about the knee. (Right) Lateral radiograph in the same child shows the NOF  , which was discovered incidentally in this patient presenting with knee pain. Notice the Osgood-Schlatter changes , which was discovered incidentally in this patient presenting with knee pain. Notice the Osgood-Schlatter changes  with fragmented anterior tibial apophysis & thickening of the patellar tendon. with fragmented anterior tibial apophysis & thickening of the patellar tendon.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|