2Genetic Medicine, St Mary’s Hospital, Manchester, UK
Overview
- The incidence of breast cancer in the world continues to increase
- The most significant risk factor for breast cancer is increasing age
- The variation in geographical rate is diminishing but is still threefold or fourfold between countries
- Breast density is an important factor in relation to breast cancer risk
- Approximately 5% of patients with breast cancer inherit a high-penetrance cancer-predisposing gene
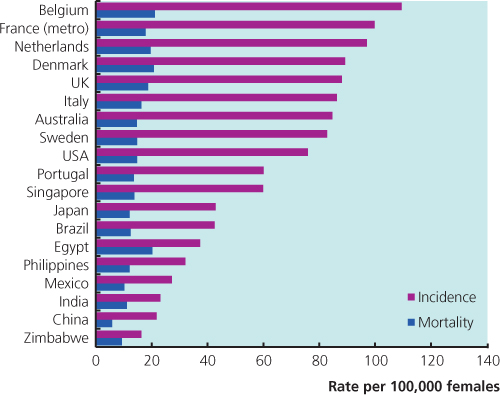
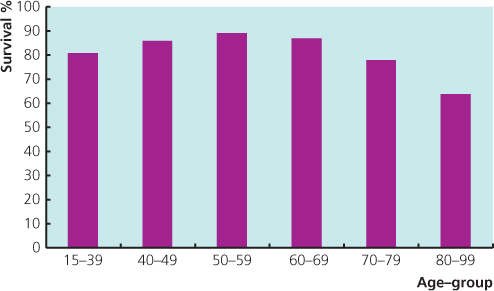
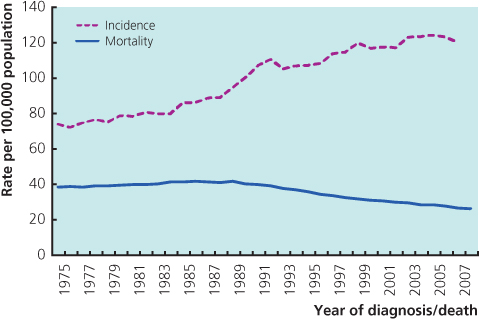
With over 1.4 million new cases in the world each year, breast cancer is the commonest malignancy in women and comprises 23% of all female cancers. In the United Kingdom, where the age-standardised incidence and mortality are among the highest in the world (Figure 5.1), the annual incidence among women aged 50 and over is almost 3 per 1000, rising to over 4 per 1000 at age 65–69. The disease is the commonest cause of death among women aged 40–50, accounting for about a fifth of all deaths in this age group. The introduction of the national screening programme in Britain in the late 1980s led to an increase in incidence as a pool of undiagnosed cancers was detected. Screening is offered every three years from age 50–70 and currently 8.1 per 1000 women screened are found to have cancer (including DCIS, ductal carcinoma in situ). Over the last 30 years the annual number of new cases of breast cancer in women has almost doubled. There are more than 12 000 deaths each year. Overall, in the last 10 years death rates from breast cancer have fallen by almost a fifth. Breast cancer survival rates vary by age at diagnosis (Figure 5.2), with those diagnosed in their 50s and 60s having higher survival rates than either younger or older patients.
Risk Factors for Breast Cancer
Age
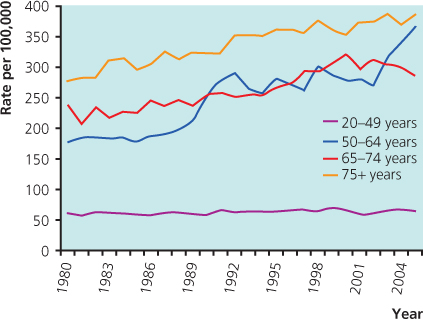
The incidence of breast cancer increases with age (Figure 5.3), doubling about every 10 years until the menopause, when the rate of increase slows dramatically. Compared with lung cancer, the incidence of breast cancer is higher at younger ages. In some countries there is a flattening of the age–incidence curve after the menopause (Figure 5.4).
Geographical Variation/Race
Breast cancer rates are similar around the world in premenopausal women, but there are striking differences after the age of 50 where the incidences in the Caucasian population in North America, Western Europe and Australia are higher than for most other regions (Figure 5.1). Age-adjusted incidence and mortality for breast cancer vary by up to a factor of five between countries. The difference between Far Eastern and Western countries is diminishing, but is still about threefold to fourfold. Studies of migrants from Japan to Hawaii show that the rates of breast cancer in migrants assume the rate in the host country within one or two generations, indicating that environmental factors are of greater importance than genetic factors (Figure 5.5).
Figure 5.5 Annual incidence of breast cancer in Japanese women in Japan, Hawaii and San Francisco and in white women in San Francisco.
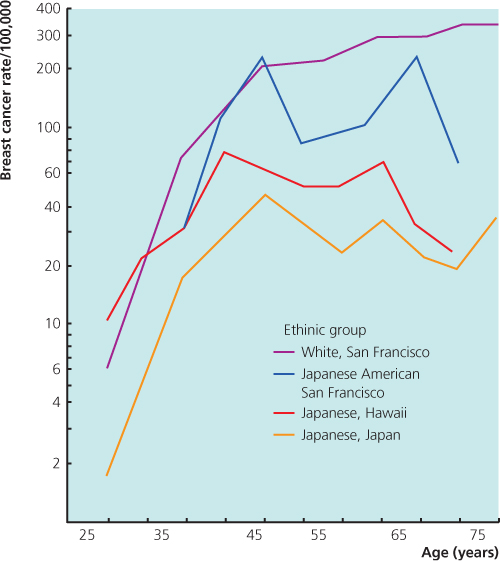
Overall, breast cancer rates are lower in the Asian and African population after the age of 50, but similar prior to age 50 when compared to Caucasian women. In the United States, non-Hispanic whites have the highest incidence of breast cancer, whereas Asian Americans have the lowest rate. Among those aged 40–50, African American women have a higher incidence compared with non-Hispanic white women. African American and Hispanic women have also the highest death rate from breast cancer. This is at least partly due to a younger age at onset, where prognosis is generally poorer, but other factors may contribute to these variations, such as lifestyle differences, access to primary care and socioeconomic factors.
Breast Density
Breast density constitutes the single largest population-attributable risk among known risk factors for breast cancer. Density of the breast decreases with age, but the increased risk in women with the most dense breasts is apparent for both pre- and postmenopausal women. Breast density is reduced in tamoxifen users, is increased with hormone replacement therapy use and is higher in nulliparous women and those with atypical hyperplasia. A meta-analysis of over 14 000 cases of breast cancer and 226 000 non-cases from 42 studies showed that the increase in relative risk of breast cancer was fourfold to fivefold comparing women with high-density versus low-density breasts.
Age at Menarche and Menopause
Women who start menstruating early in life or who have a late menopause have an increased risk of developing breast cancer. Women who have a natural menopause after the age of 55 are twice as likely to develop breast cancer as women who experience the menopause before the age of 45. At the other extreme, women who undergo bilateral oophorectomy before the age of 35 have only 40% of the risk of breast cancer of women who have a natural menopause.
Age at First Pregnancy
Nulliparity and late age at first childbirth both increase lifetime incidence of breast cancer. The risk of breast cancer in a woman who has had her first child after the age of 30 is about twice that of a woman who has had her first child before the age of 20. The highest-risk groups are those who have a first child after the age of 35; these women appear to be at even higher risk than nulliparous women. An early age at birth of a second child further reduces the risk of breast cancer.
Family History
Approximately 5% of breast cancer in Western countries is due to a strong genetic predisposition. Breast cancer susceptibility is generally inherited as an autosomal dominant with limited penetrance. This means that it can be transmitted through either sex and that some family members may transmit the abnormal gene without developing cancer themselves.
The last 20 years have seen first the development and second an expansion of genetic risk assessment and ‘family history’ clinics to deal with the ever-increasing demand for management of women at increased risk of breast cancer due to their family history. These clinics were originally centralised in a few major units, but the demand is such that management of moderate-risk women needs to be carried out in local units. A system of triage has developed, with ‘average’-risk women being reassured in primary care, moderate-risk women receiving assessment in local units and high-risk women being referred to regional genetics centres. While mammography and MRI screening continue to be evaluated in the moderate- and high-risk categories, genetic testing for BRCA1 and BRCA2 is now routine in high-risk women and surgical risk-reduction options have gained validity. Much research is still necessary to improve risk prediction and early detection and to develop non-surgical means of prevention.
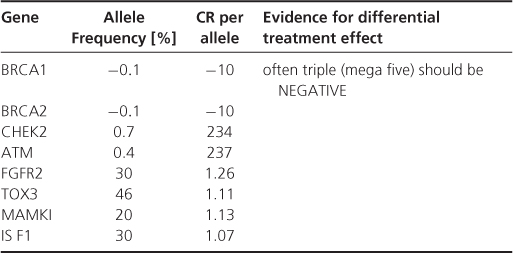
Although 5% of breast cancer is thought to be due to inheritance of a high-risk dominant cancer-predisposing gene, hereditary factors may play a part in a proportion of the remaining 95%+ of breast cancers (estimated as being important in up to 27% of breast cancers from twin studies); these have been hard to delineate (Table 5.1). Lower-risk genes have been identified from association studies. There are no external markers of risk (no phenotype) to help identify those who may carry a faulty gene, except in very rare cases such as Cowden’s disease where there are skin lesions and skull abnormalities. To determine the likelihood of there being a predisposing gene in a family, it is necessary to assess the family pedigree. Inheritance of a predisposing gene results in breast cancer development at a young age and often involving both breasts. Certain gene mutations give rise to susceptibility to other cancers, such as ovarian cancer (BRCA1/2) or sarcomas and brain cancer (TP53). Multiple primary cancers in one individual or related early-onset cancers in a pedigree are suggestive that a predisposing gene may be responsible.
Table 5.1 Genes predisposing to breast cancer.
The risk of breast cancer almost doubles if a first-degree relative (mother, sister or daughter) has had breast cancer and triples if two relatives have (Table 5.2). The risk is higher when the relative’s cancer occurred at a young age and when the woman herself is young. For example, a woman whose sister developed breast cancer aged 30–39 has a cumulative risk of 10% of developing the disease herself by age 65, but that risk is only 5% (close to the population risk) if the sister was aged above 50 at diagnosis. The risk increases by between four and six times if two first-degree relatives develop the disease. For example, a woman with two affected relatives, one who was aged under 50 at diagnosis, has a 25% chance of developing breast cancer by the age of 65.
Table 5.2 Established risk factors for breast cancer.
| Factor | Relative risk | High risk group |
| Age | >10 | Aged >55 |
| Genetic | 10 | BRCA1, BRCA2 carriers |
| Previous benign disease | 4–5 | Atypical hyperplasia or LCIS* |
| Geographical location | 4 | Developed countries |
| Mammographic density | 4 | >75% of film opaque |
| Exposure to radiation | 3 | Very high exposure in females aged 10–25 |
| Family history | ≥2 | Breast cancer in first-degree relative when aged 50 or younger |
| Combined hormone replacement therapy | 2.3 | Current use |
| Age at menopause | 2 | After age 54 |
| Age at first full pregnancy | 2 | First child >30 years or nulliparous |
| Weight | 2 | Body mass index >30 in postmenopausal women |
| Alcohol consumption | 1.3 | Excessive intake |
| Oral contraceptives | 1.3 | Current use |
*LCIS, lobular carcinoma in situ (see Chapter 16).
The important features in a family history are the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree