Brain Tumor in Newborn/Infant
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
Anaplastic Astrocytoma
Teratoma
Medulloblastoma (PNET-MB)
Supratentorial PNET
Supratentorial Ependymoma
Choroid Plexus Papilloma
Less Common
Subependymal Giant Cell Astrocytoma
Desmoplastic Infantile Ganglioglioma
Desmoplastic Infantile Astrocytoma
Glioblastoma Multiforme
Rare but Important
Choroid Plexus Carcinoma
Atypical Teratoid-Rhabdoid Tumor
Neurocutaneous Melanosis (Melanoma/Melanocytoma)
Pineoblastoma
Brainstem Glioma, Pediatric
Medulloepithelioma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Newborn/infant brain tumors
Typically large, bulky, inhomogeneous
Supra- > infratentorial (infratentorial more common in older children)
Helpful Clues for Common Diagnoses
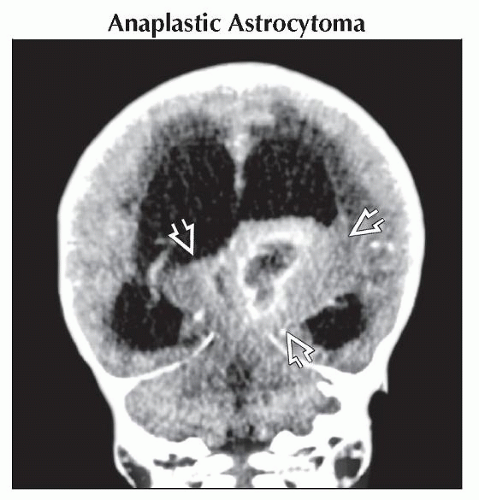
Anaplastic Astrocytoma
Infiltrating mass, predominantly white matter (WM)
Hemispheric WM (frontotemporal)
Ca++ rare; heterogeneous on MR
No or variable enhancement
Ring enhancement, bleed, necrosis, flow voids suggest GBM
Teratoma
Midline, supratentorial
Small lobular or holocranial
Contents
Ca++, cysts, fat
Enhancing soft tissue
Look for associated congenital brain anomalies
Medulloblastoma (PNET-MB)
4th ventricle mass with hydrocephalus
Restricts on DWI (best MR clue)
Sparse Ca++ ≈ 20%
Enhancement usual (may be late/slow)
Hemorrhage rare
Hypercellularity reflected on imaging
Hyperdense (NECT), hypointense (T2)
Medulloblastoma with extensive nodularity
Subtype with expanded lobular architecture
Grape-like enhancement
Better prognosis
Supratentorial PNET
Large complex mass
Restricts on DWI (differentiates from ependymoma)
Heterogeneous signal, enhancement
Ca++ more common than in posterior fossa PNETs
Hemorrhage, necrosis common
Hemispheric
Mean diameter 5 cm
Especially newborn/infants
Minimal peritumoral edema
Suprasellar
Early neuroendocrine, visual disturbances
Pineal (pineoblastoma)
Hydrocephalus, Parinaud syndrome
Supratentorial Ependymoma
Peri/extraventricular > intraventricular
Periventricular ependymal rests
Large, bulky
Ca++ ≈ 50%
Variable necrosis, hemorrhage
Choroid Plexus Papilloma
CPP: Lobulated intraventricular mass
Lateral > 4th > 3rd
NECT: Iso- to dense
Iso- to slightly hyperintense on T2WI
Vividly enhancing
Hydrocephalus common
Helpful Clues for Less Common Diagnoses
Subependymal Giant Cell Astrocytoma
Enhancing mass near foramen of Monro
Found in tuberous sclerosis complex
Look for
Subependymal Ca++ nodules
Tubers (best on FLAIR)
Desmoplastic Infantile Ganglioglioma
Desmoplastic Infantile Astrocytoma
Similar to (but rarer than) DIG
Glioblastoma Multiforme
Bulky irregular enhancing tumor
Peritumoral edema, mass effect
Hemorrhage, central necrosis, cysts
↑ glucose metabolism, avid FDG accumulation on PET
Helpful Clues for Rare Diagnoses
Choroid Plexus Carcinoma
Similar to CPP PLUS
Brain invasion
Ca++, cysts, bleed
Ependymal, subarachnoid space seeding (can be seen with both CPP, CPC)
Atypical Teratoid-Rhabdoid Tumor
PNET-MB-like PLUS
Metastases at diagnosis more common
Cysts, hemorrhage more common
Cerebellopontine angle cistern location more common
Neurocutaneous Melanosis (Melanoma/Melanocytoma)
Giant or multiple cutaneous melanocytic nevi PLUS
Melanosis: Bright T1 amygdala, cerebellum
Melanoma: Melanosis + diffuse leptomeningeal enhancement
Pineoblastoma
Large heterogeneous pineal region mass
Peripheral Ca++
Small cysts
Inhomogeneous enhancement
Invades adjacent structures
Corpus callosum, thalamus, midbrain, vermis
Hydrocephalus usual at diagnosis
Brainstem Glioma, Pediatric
Imaging appearance, prognosis vary with tumor type, location
Tectal
Pilocytic astrocytoma
Clinically indolent course (may cause obstructive hydrocephalus)
Variable enhancement/Ca++
Focal tegmental mesencephalic
Pilocytic astrocytoma
Cyst + nodule
Surgery, radiation, or chemotherapy
Patients generally do well
Diffuse pontine glioma
Diffusely infiltrating fibrillary astrocytoma
Nonenhancing early in course
Enhancement with malignant progression
Survival generally poor
Medulloepithelioma
Rare malignant embryonal brain tumor
Young children (< 5 years)
Histologic differentiation varies
Neuronal, astrocytic, ependymal, melanotic, etc.
Imaging appearance reflects variable differentiation
Image Gallery
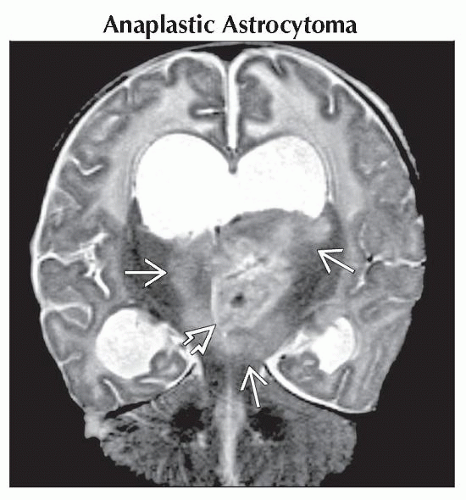 Coronal T2WI MR in same case shows the mass
 is extensively infiltrating, with bithalamic and upper midbrain hyperintensity is extensively infiltrating, with bithalamic and upper midbrain hyperintensity  , causing obstructive hydrocephalus with transependymal CSF migration. , causing obstructive hydrocephalus with transependymal CSF migration.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|