FIGURE 21-1 The return of internal rotator strength before ER muscle activity leads to an imbalance about the glenohumeral joint. This can progress to deformity and dislocation.
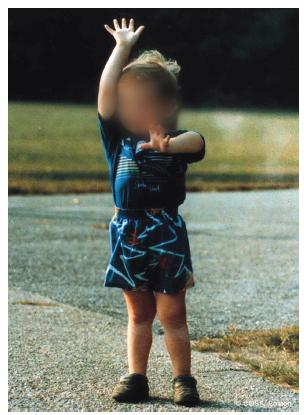
FIGURE 21-2 The affected left arm of this child with incomplete recovery reveals restrictions in ER and above horizontal shoulder function that is typical for these patients. He has to reach his mouth with his shoulder maximally abducted. He cannot reach the top of head and can only reach the left side by tilting his neck forward and to the side. His humeral head is dislocated.
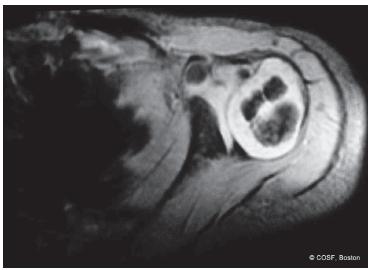
FIGURE 21-3 MRI of the affected glenohumeral joint reveals posterior subluxation of the humeral head and glenoid deformity with an early pseudoglenoid or biconcave joint. The humeral head is already beginning to change shape, and the position of the biceps insertion reveals the presence of an internal rotation contracture.
Etiology and Epidemiology
Between 10% and 40% of infants with BPBP will have an incomplete recovery. Some will have minimal deficits; others will have profound, permanent disability. The C5–C6 (–C7) children with an incomplete recovery are more at risk for glenohumeral dysplasia and dislocation4 than either the total plexus or the minimally affected patients. Publications on shoulder dislocations and deformity date back to Stimson and Fairbank and include many modern publications.5–7 Cumulative knowledge is now extensive. Glenohumeral dysplasia and dislocation are clearly high risk for children with continued imbalance and contracture.8 Close monitoring, evaluation, and treatment are required. Through the radiographic advances of MRI scans, confirmed by ultrasound and arthrograms, it is clear that deformity starts very early in life and is progressive if untreated.
Clinical Evaluation
Assessing individual muscle strength in an infant can be challenging. The Medical Research Council (MRC) muscle strength grading system (0 to 5) is too exacting, as infants and toddlers cannot follow verbal instructions for resistive testing. Recognizing that muscle strength has to be inferred from observed or stimulated movement in infants and children, Gilbert and Tassin modified that MRC system to a four-point gradation: (0) no muscle contracture, (1) muscle contracture without movement, (2) movement with gravity eliminated, and (3) complete movement against weight of extremity (Table 21.1). Other classification systems include the modified Mallet scale (Figure 21-4, Table 21.2) and the Hospital For Sick Children Active Movement Scale (Figure 21-5).9–11 These later systems have been shown to have inter- and intraobserver reliability.
Table 21.1 Gilbert and Tassin’s modified MRC classification for motor strength
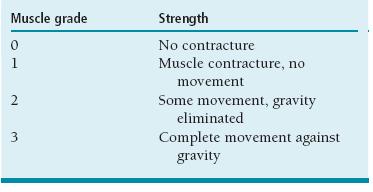
From Gilbert A, Tassin JL. Surgical repair of the brachial plexus in obstetric paralysis. Chirurgie. 1984;110(1):70-5.
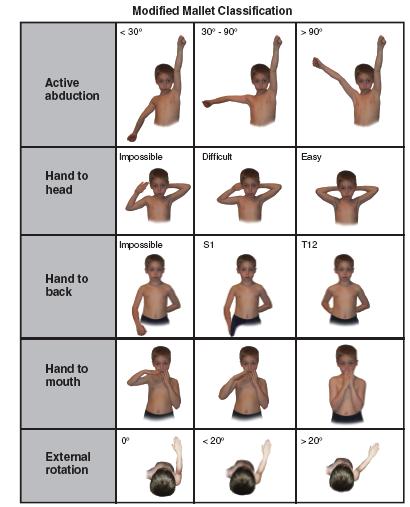
FIGURE 21-4 Modified Mallet classification for global abduction, ER, hand to neck, hand to spine, and hand to mouth. Each category is graded I to V with I, no function; V, normal function, and grades II, III, and IV depicted by illustration. Some children are not testable due to age and lack of cooperation at that particular visit. An aggregate Mallet score is a combination of the scores for all five categories, ranging 0 to 25.
Table 21.2 Modified Mallet classification
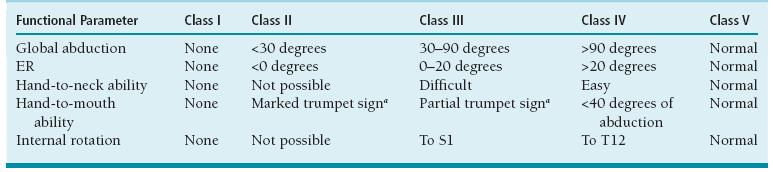
aA trumpet sign consists of abduction of the shoulder with simultaneous flexion of the elbow.
From Mallet J. Paralysie obstetricale du pexus brachial. Traitment des sequelles.
Rev Chir Orthop. 1972;55(suppl):8-166.
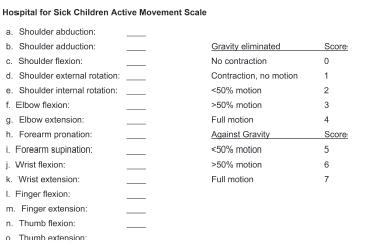
FIGURE 21-5 The Hospital For Sick Children Active Movement Scale grades each muscle movement from the shoulder to the hand by a score of 0 (no function) to 7 (normal function). A child must have full gravity-assisted function (score of 4) before antigravity scoring can be obtained.
Assessing passive range of motion is an essential part of comprehensive shoulder evaluation in these patients. Maintaining passive ER with scapular stabilization is integral to their therapy program. Conversely, those infants and children losing ER in adduction12 and/or abduction2 are most at risk for glenohumeral deformity (Figure 21-6). Before a fixed deformity develops, the shoulder instability can be palpated in the posterior soft spot with alternating internal (subluxation) and external (reduction) rotation. Later, the dislocated humeral head is palpable posteriorly with clear asymmetry to the opposite side anatomic situation (Figure 21-7). Scapular winging is present in all these children with muscle imbalance and contracture (Figure 21-8).

FIGURE 21-6 With the scapula stabilized, this patient has limited ER in adduction. The glenohumeral joint needs investigation for deformity.

FIGURE 21-7 View of the affected right shoulder with obvious posterior dislocation of humeral head.

FIGURE 21-8 Marked scapular winging in this patient with dysplastic glenohumeral joint and shoulder contractures.
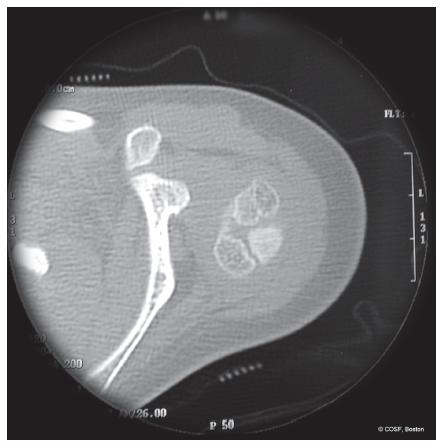
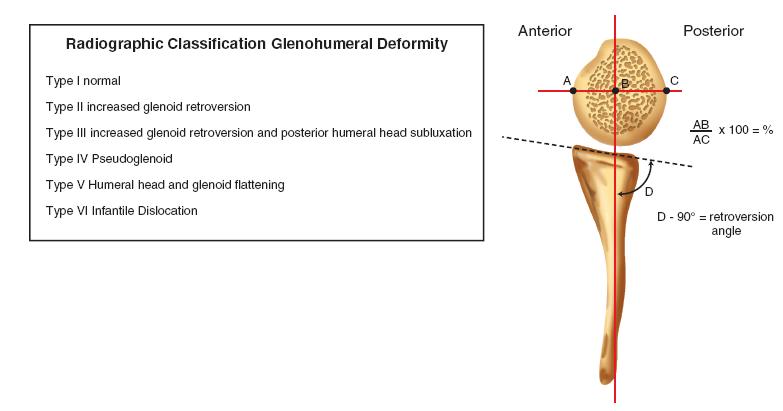
Advanced radiographic evaluation is now a significant part of treatment planning for these patients. Plain radiographs give limited information due to the major unossified areas about the shoulder at this age. Ultrasound in skilled hands provides definitive information on glenoid dysplasia and joint alignment similar to hip ultrasounds in developmental dysplasia. MRI scans are diagnostic (Figure 21-9).13 CT scans are faster, cheaper, and give comparable information as MRI scans but have high radiation dosing and do not show the unossified glenoid apophysis14,15 (Figures 21-10 and 21-11). Arthrograms also give comparable information16–19 (Figures 21-12 and 21-13). The clinical continuum of dysplasia at the glenohumeral joint progresses from anatomic alignment and symmetric development, increased glenoid retroversion, humeral head posterior subluxation, and biconcave or pseudoglenoid (Figure 21-14) to a frank dislocation with a flat humeral head and glenoid (Figures 21-15 and 21-16). The degree of deformity can guide the surgeon on timing and the type of operative intervention. MRI scans are more capable than physical examinations of revealing the presence and degree of glenohumeral dysplasia.
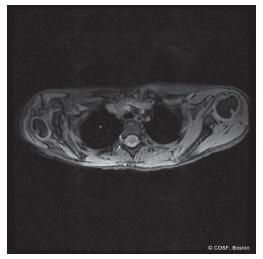
FIGURE 21-9 Obvious asymmetry between affected and unaffected glenohumeral joints by MRI scan. The affected side has marked glenoid deformity, posterior subluxation of the humeral head, and a pseudoglenoid. The unaffected side has anatomic alignment.
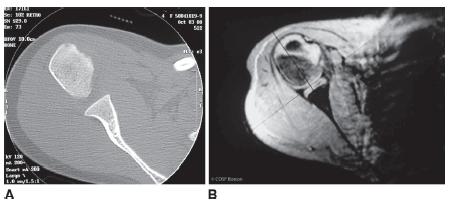
FIGURE 21-11 Normal glenohumeral joint with humeral head centralized and normal glenoid retroversion for age by CT (A) and MRI (B) (Type I glenoid).

FIGURE 21-12 Type II deformity with mild increased retroversion and the beginnings of humeral head subluxation.
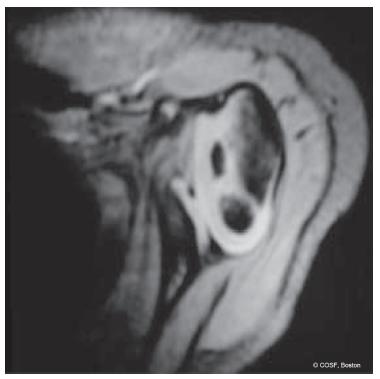
FIGURE 21-13 Type III deformity with increased retroversion and posterior subluxation of the humeral head.

FIGURE 21-14 Type IV deformity with humeral head dislocation and the development of a pseudoglenoid, or biconcave, joint.
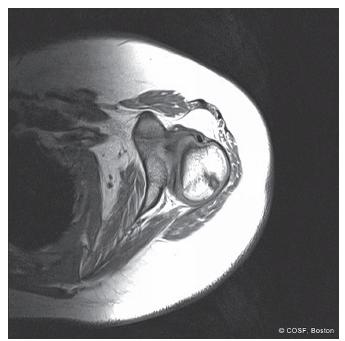
FIGURE 21-15 Type V deformity with flat glenoid, flat humeral head, and complete posterior displacement of humeral head.
Surgical Indications
Indications for surgery about the shoulder in these children include (1) infantile dislocation, (2) persistent internal rotation contracture despite maximal nonoperative treatment, (3) limitation of active ER and above shoulderlevel function with plateauing of neurologic recovery, (4) progressive or marked glenohumeral deformity, and (5) a combination of any or all of these (Figure 21-17). The age at intervention is dependent on the severity of the problem and when the patient presents for care. The spectrum can be from the first 6 to 12 months of life through adolescence. We advocate early intervention when indicated to prevent progressive deformity, allow for joint remodeling, and maximize function.
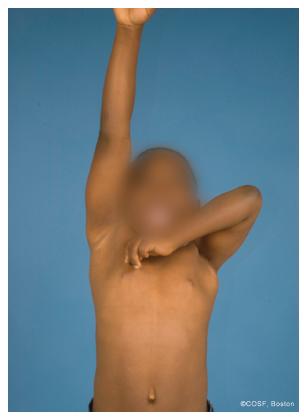
FIGURE 21-17 Typical patient with normal right arm elevation and affected left arm with multiple problems: internal rotation contracture, lack of ER and antigravity triceps strength, and a good hand.
Almost all publications over the past 100 plus years indicate the problem is a combination of muscle imbalance, soft tissue contracture, and bone and joint deformity. The interventions recommended in those papers, public presentations, and patient consultations are various ways of addressing those issues. Surgical guidelines that emerge are (1) in the young child (6 months to 2 years) with resistant contracture but potential ongoing ER and abduction recovery, intervention for contracture release alone (botulinum toxin A [Botox, Allergan Pharmaceuticals, Inc., Irvine, CA] injection, subscapularis slide, arthroscopic joint release, coracoacromial ligament release) is indicated20–23; (2) in the slightly older child (2 to 5 years), a combination of releases and tendon transfers is indicated since active ER recovery is no longer feasible15,24–27; (3) joint reduction is indicated if there is moderate-to-marked joint deformity in the younger child (6 months to 5 years) with remodeling potential28,29; (4) bony surgery, such as humeral osteotomy, is necessary in older children with severe deformity.30,31 Most of these methods achieve the same goal.32 We have outlined broad guidelines, and each patient may require a variation depending on the physical exam, MRI scan findings, and social situation to achieve a successful outcome.
SURGICAL PROCEDURES
You don’t suffer, kill yourself and take the risks I take just for money. I love bike racing.
—Greg LeMond, three-time Tour de France winner
 Physical Therapy
Physical Therapy
Supervising therapy and monitoring recovery are important aspects of treatment of these children. Since glenohumeral dysplasia can start very early in life, prioritizing fullshoulder passive range of motion from month 1 is important. Stabilization of the scapula with passive abduction, ER in adduction and abduction, and forward flexion should become a many times a day routine for the families. Since in the first 2 years of life, diapers are changed on average eight times a day, this is an excellent opportunity and reminder for therapy. Loss of passive motion clearly correlates with the risk of glenohumeral deformity and dislocation. If adduction and ER approach 0 degrees, or abduction and ER approach <90 degrees (straight vertical), then further intervention is warranted. Depending on the situation, this may be a trial of more supervised therapy; Botox injections in the subscapularis, teres major, and/or pectoralis major muscles; or an MRI scan to assess deformity and joint alignment.
Botox Injection
Botox injection may be indicated in patients who are failing to maintain passive ER and joint reduction in the first 2 years of life despite vigorous, supervised appropriate physical therapy.33 Since Botox is currently used off-label, proper informed consent must be obtained. The published beneficial effects of Botox injections in cerebral palsy muscle imbalance, and early, similarly positive results in BPBP, warrant its use in the suitable patient. Dosage is 1 to 3 U/kg, not to exceed 10 U/kg, injected in equally divided doses into the pectoralis major, subscapularis, and teres major. This is done under general anesthesia and sterile prep conditions. Percutaneous electrical stimulation can be used to isolate each muscle for injection. Following Botox injection, the shoulder is reduced and casted. A shoulder spica is applied with the shoulder adducted approximately 30 to 40 degrees and externally rotated approximately 60 degrees. The elbow is flexed and the forearm is supinated. Postreduction and spica ultrasound or MRI scan is obtained to confirm reduction. The spica is maintained for 4 to 6 weeks depending on the age of the patient. Therapy is reinitiated.
 Subscapularis Slide
Subscapularis Slide
Subscapularis release or lengthening to correct the internal rotation contracture and improve ER function dates back to Fairbank.7 Options for dealing with the contracted subscapularis have included tenotomy, Z-lengthening, and muscle slide. Muscle slide, as described by Carlioz and advocated by Gilbert, improves passive ER with less risk of losing internal rotation power or postoperative ER contracture.22 In the young child with a chance of ongoing muscle recovery (6 months to 2 years), this can be done in isolation. In older children with mild joint deformity, it is done in conjunction with extra-articular tendon transfers.
In a lateral decubitus position (this can also be done semiprone or prone) with the affected arm up, care is taken to softly pad all neurovascular structures (including opposite brachial plexus, peroneal and ulnar nerves) and bony prominences. The entire shoulder girdle and arm are prepped and draped to allow for surgical exposure of the medial scapula and measurement of passive ER. A longitudinal medial scapular incision is utilized. Dissection is carried down the anterior medial border of the scapula. Using a Bovie electrocautery (Bovie Medical Corp., Clearwater, FL) and then a broad elevator, the subscapularis origin is released off the anterior scapula. Throughout its proximal to distal length, the entire muscle belly is mobilized from medial to lateral. Passive ER of the arm in adduction facilitates the correction. Generally the arm is contracted at 0 degrees or less of ER in adduction; and the goal is to achieve 60 to 80 degrees intraoperatively without undo tension. Once achieved, the wound is closed in layers with absorbable suture. A shoulder spica cast is used to maintain the corrected adduction and ER position for 4 weeks followed by intensive therapy.
 Arthroscopic and Open Joint Releases
Arthroscopic and Open Joint Releases
Pearl introduced the use of arthroscopic techniques to achieve similar goals as open procedures.23 The difference is that arthroscopic releases start from the inside out, while the open procedures come from the outside in. In a complete release, the procedure can achieve the same results using different techniques. However, in a partial release, different anatomic structures will be involved. The outcome in terms of undercorrection or overrelease could be different (partial vs. complete subscapularis release; partial, complete, or no joint capsule and ligament release). In addition, the application of each technique requires different skill sets. Open releases and reduction require ease and expertise at dissecting around and near the brachial plexus nerves. Arthroscopic releases and reduction require technical prowess and familiarity with appropriate-sized arthroscopic equipment for a young child. So far, the published results indicate equivalency of joint remodeling and clinical outcome.
 Arthroscopic Release and Reduction
Arthroscopic Release and Reduction
This procedure is performed in a lateral decubitus position with the affected arm up. Care is taken to softly pad all neurovascular structures (including opposite brachial plexus, peroneal and ulnar nerves) and bony prominences. A beanbag is used to maintain body position throughout the procedure. Prepping and draping includes the entire arm and shoulder girdle region. Through the posterior soft spot, an appropriate-sized spinal needle is used to inflate the joint with injectable saline and age- and weight- appropriate diluted epinephrine. The posterior portal is distal and medial to the posterolateral acromion between infraspinatus and teres minor and can be palpated with your thumb during internal rotation and ER. Confirmation of the needle in the joint is seen by free backflow. Full distention of the joint allows for atraumatic placement of arthroscopic equipment by separating the humeral head and glenoid. This is particularly important in such a small joint. Visualization is performed from the posterior portal. Manual distraction of the joint is necessary, and this requires an attentive, able-bodied assistant applying longitudinal traction on the arm. At present, there is no commercially available shoulder/limb positioning device suitable for infants and young children.
The posterior subluxation of the humeral head and increased glenoid retroversion are evident and correlate with MRI findings. The anterior portal is then localized with an outside-in spinal needle in the rotator interval between the medial labrum, inferior subscapularis, and superior biceps tendon. The operative release is performed from this portal. Mayo scissors, rongeurs, arthroscopic biters, and lasers have all been used for the release. A hooked Bovie electrocautery device is our instrument of choice (Figure 21-18). The release is on the anterior-inferior edge and involves the capsule, inferior, and middle glenohumeral ligaments. The overlying subscapularis is partially released. A back and forth between release and measurement of passive ER and joint reduction is performed until more than 40 to 60 degrees of tensionfree ER with a reduced humeral head is achieved. Care is taken not to overrelease the joint or perform an entire subscapularis release due to concern about loss of internal rotation power and/or development of an ER contracture. Anterior-inferior glenohumeral instability can also occur with an extensive release. The axillary nerve is nearby and needs protection throughout the procedure. We identify the nerve beneath triceps and deltoid and protect it throughout its anatomic course. If the triceps fascia is impinging the nerve, we release the fascia to compress the nerve. At the conclusion, the portals are closed, and a shoulder spica cast is applied in adduction and ER to maintain reduction. The cast is discontinued at 4 to 6 weeks and therapy initiated.
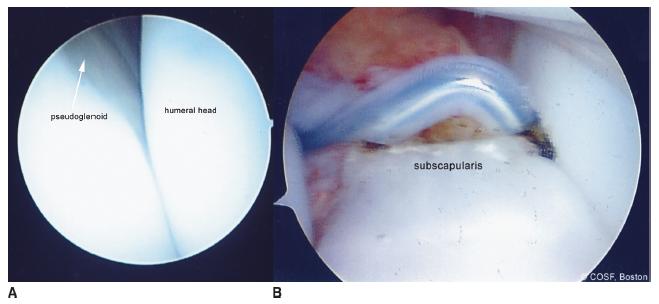
FIGURE 21-18 A: Arthroscopic view of glenoid deformity during partial reduction of the humeral head with maximum ER. B: Hooked Bovie electrocautery partial release of anterior capsule and subscapularis. You have to be careful not to overrelease with resultant loss of internal rotation movement and power.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree