Board Simulation: Infectious Diseases
Camille Sabella
QUESTIONS
1. Two days before delivering a term infant, the 20-yearold mother develops chickenpox. The most appropriate management plan is to:
a) Administer intravenous acyclovir to the infant at birth.
b) Administer both acyclovir and varicella-zoster immune globulin (Ig) to the infant at birth.
c) Administer varicella-zoster Ig to the infant at birth.
d) Administer varicella-zoster Ig to both the mother and the infant.
e) Administer varicella-zoster Ig to the infant if varicella develops.
View Answer
Answer
The answer is c. Varicella-zoster Ig is given to prevent or modify the course of varicella in susceptible individuals at risk for severe varicella infection. This includes neonates of mothers in whom varicella develops between 5 days before and 2 days after delivery. Neonates born within this time frame are at high risk for severe infection because they acquire the virus transplacentally, without the benefit of protective maternal antibody. Other individuals who are candidates for receiving varicella-zoster Ig when they have a significant exposure include:
Susceptible immunocompromised individuals
Hospitalized premature infants (≥28 weeks gestation) whose mothers lack a reliable history of varicella or serologic evidence of protection against varicella
Hospitalized premature infants who had <28 weeks of gestation or weigh 1000 g or less at birth
Susceptible pregnant women
Varicella-zoster Ig should be given as soon as possible after the exposure and within 96 hours of the exposure to be effective. It is not effective for the treatment of established infection. If varicella zoster Ig is not available, intravenous Ig can be substituted.
Acyclovir is an antiviral agent used to treat varicella in immunocompromised patients and occasionally in healthy individuals who may be at increased risk for complications of varicella) Acyclovir may be used for postexposure prophylaxis for immunocompromised patients when varicella zoster Ig or Ig are not available, or when >96 hours have elapsed since exposure, although data regarding the effectiveness of this practice are scant.
Questions 2-6
From the list of viruses, choose the one most likely to be involved in each of the clinical scenarios.
a) Parvovirus B19
b) Measles
c) Epstein-Barr virus (EBV)
d) Rubella virus
e) Human herpes virus 6
2. A 13-year-old in whom a confluent rash develops during inadvertent treatment with ampicillin
View Answer
2. The answer is c. A rash develops in approximately 80% to 90% of individuals with infectious mononucleosis caused by EBV or CMV who are inadvertently treated with ampicillin. The reason is unclear.
3. A school-aged child with a lace-like reticular rash on the extremities
View Answer
3. The answer is a. Parvovirus B19 is the cause of erythema infectiosum, also known as slapped cheek or fifth disease. An intense erythematous rash develops on the cheeks along with a systemic, lace-like eruption on the trunk and extremities (see Fig. 1.20). The eruption may be pruritic and is often evanescent.
4. An adolescent with a discrete maculopapular rash beginning on the face and with tender postauricular and postoccipital adenopathy
View Answer
4. The answer is d. Rubella, mostly an illness of adolescents and young adults in the postvaccine era, generally causes asymptomatic infection. The classic features, when present, include a discrete, often pinpoint rash that begins on the face and spreads to the trunk. Postauricular and postoccipital tender adenopathy is said to be most characteristic of rubella.
5. An infant with a maculopapular rash following 3 to 5 days of high fever
View Answer
5. The answer is e. Classic roseola is characterized by 3 to 5 days of high fever, often associated with toxicity, followed by defervescence and the appearance of a maculopapular rash. Human herpes virus 6 is the etiologic agent of roseola; it is also a common cause of febrile illness without rash in infants and children.
6. A child with a croup-like cough, high fever, and confluent maculopapular rash
View Answer
6. The answer is b. Measles is characterized by a prodrome manifesting with fever, cough, coryza, conjunctivitis, and Koplik spots, the pathognomonic feature of measles. A rash, accompanied by high fever, follows the prodrome. The respiratory symptoms of measles, especially the cough, are striking. The rash typically begins on the neck, head, and face and spreads to the trunk and extremities. As the rash spreads, it becomes confluent.
Answers
2. The answer is c. A rash develops in approximately 80% to 90% of individuals with infectious mononucleosis caused by EBV or CMV who are inadvertently treated with ampicillin. The reason is unclear.
3. The answer is a. Parvovirus B19 is the cause of erythema infectiosum, also known as slapped cheek or fifth
disease. An intense erythematous rash develops on the cheeks along with a systemic, lace-like eruption on the trunk and extremities (see Fig. 1.20). The eruption may be pruritic and is often evanescent.
disease. An intense erythematous rash develops on the cheeks along with a systemic, lace-like eruption on the trunk and extremities (see Fig. 1.20). The eruption may be pruritic and is often evanescent.
4. The answer is d. Rubella, mostly an illness of adolescents and young adults in the postvaccine era, generally causes asymptomatic infection. The classic features, when present, include a discrete, often pinpoint rash that begins on the face and spreads to the trunk. Postauricular and postoccipital tender adenopathy is said to be most characteristic of rubella.
5. The answer is e. Classic roseola is characterized by 3 to 5 days of high fever, often associated with toxicity, followed by defervescence and the appearance of a maculopapular rash. Human herpes virus 6 is the etiologic agent of roseola; it is also a common cause of febrile illness without rash in infants and children.
6. The answer is b. Measles is characterized by a prodrome manifesting with fever, cough, coryza, conjunctivitis, and Koplik spots, the pathognomonic feature of measles. A rash, accompanied by high fever, follows the prodrome. The respiratory symptoms of measles, especially the cough, are striking. The rash typically begins on the neck, head, and face and spreads to the trunk and extremities. As the rash spreads, it becomes confluent.
7. Mycoplasma pneumoniae is associated with which of the following?
a) Laryngotracheitis
b) Erythema multiforme
c) Pharyngitis
d) Pneumonia
e) All of the above
View Answer
Answer
The answer is e. M. pneumoniae is associated with many clinical manifestations. Atypical pneumonia in schoolaged children and adolescents is the most important of these. Indeed, M. pneumoniae is the most common cause of pneumonia in school-aged children. Pharyngitis as an isolated finding is rare but is common in conjunction with pneumonia. Approximately 2% to 4% of cases of croup are caused by this organism. M. pneumoniae and herpes simplex virus are the most common infectious agents of erythema multiforme/Stevens-Johnson syndrome. M. pneumoniae is also associated with bullous myringitis and otitis media, hemolytic anemia, and common gastrointestinal symptoms. Neurologic manifestations of infection with this organism include aseptic meningitis, encephalitis, Guillain-Barré syndrome, and transverse myelitis.
8. A 5-week-old infant presents with a 5-day history of tachypnea and dry cough. The mother notes that the infant had drainage from both eyes 2 weeks before the onset of symptoms. Physical examination reveals an afebrile, well-appearing infant who is mildly tachypneic and has rales bilaterally. Chest radiography reveals hyperexpanded lungs with bilateral interstitial infiltrates. The most likely etiologic agent is:
a) Group B streptococci
b) Chlamydia trachomatis
c) Staphylococcus aureus
d) Streptococcus pneumoniae
e) Chlamyophila (formerly Chlamydia) pneumoniae
View Answer
Answer
The answer is b. Pneumonia develops in approximately 10% to 20% of infants born to women with C. trachomatis infection. The illness usually presents in infants between 3 and 12 weeks of age, and 30% to 50% of them have a history of conjunctivitis. The clinical onset is insidious, with persistent cough, tachypnea, and rales as common clinical features. Fever is characteristically absent. Peripheral eosinophilia is common. Chest radiography reveals hyperinflation and interstitial infiltrates. Erythromycin for 14 days is the standard treatment for infants with Chlamydia pneumonia and conjunctivitis.
Chamydophila (formerly Chlamydia) pneumoniae does not cause pneumonia in young infants. The initial illness develops during the school age years and is associated with asymptomatic infection, pharyngitis, and atypical pneumonia. Pneumonia associated with group B streptococci most commonly accompanies early-onset disease and is uncommon in late-onset disease. S. pneumoniae and S. aureus cause in young infants severe, febrile pneumonia that is associated with an acute onset, toxicity, and focal infiltrates.
9. A 1-year-old previously healthy boy presents with a 6-day history of fever and swelling on the right side of the neck. Physical examination reveals an erythematous, tender, 4 × 4-cm fluctuant lymph node at the angle of the mandible. The most likely etiologic agent causing the adenitis is:
a) Group B streptococci
b) Mycobacterium avium complex
c) Bartonella henselae
d) S. aureus
e) Mycobacterium tuberculosis
View Answer
Answer
The answer is d. This infant has acute pyogenic cervical adenitis, which in most cases is caused by S. aureus, S. pyogenes, or anaerobic organisms. The adenitis is generally unilateral and occurs in children between the ages of 1 and 4 years. Infections with S. aureus can be difficult to distinguish from those with S. pyogenes, but in general, staphylococcal adenitis is more indolent although more likely to become suppurative (Fig. 51.1). Overall, 25% to 40% of infections with S. aureus become suppurative and require surgical drainage. Mycobacterial adenitis usually manifests as subacute or chronic lymphadenitis and is very rarely associated with fluctuance. B. henselae is the causative agent of cat scratch adenitis,
which characteristically has a subacute presentation. Group B streptococci can cause an adenitis-cellulitis syndrome, almost exclusively in neonates.
which characteristically has a subacute presentation. Group B streptococci can cause an adenitis-cellulitis syndrome, almost exclusively in neonates.
 Figure 51.1 Suppurative adenitis in an infant. The purulent material drained from this infant grew Staphylococcus aureus. (See color insert.) |
Questions 10-11
A 7-year-old child presents with a 4-week history of an enlarged, mildly tender submandibular lymph node. On physical examination, he is afebrile, nontoxic, and has a 4 × 4-cm mildly tender, nonfluctuant submandibular lymph node.
10. Appropriate management at this point would include:
a) Incision and drainage of the lymph node
b) Removal of the lymph node
c) Complete blood cell count and chest radiography
d) Placement of a double-strength (250-TU [tuberculin unit]) tuberculin skin test
View Answer
Answer
The answer is c. This child has subacute lymphadenopathy. Potential causes include:
Cat scratch disease
M. tuberculosis infection
Nontuberculous mycobacterial infection
Actinomycosis
Toxoplasmosis
Malignancy
Of the choices given, a complete blood cell count and chest radiography are reasonable given that malignancy and tuberculosis are included in the differential diagnosis. Incision and drainage of the lymph node are indicated if the node is fluctuant. Removal of the node is appropriate if the diagnosis of nontuberculous mycobacterial infection is thought likely and other causes have been excluded. A double-strength tuberculin skin test should never be utilized to assess previous exposure to tuberculosis or nontuberculous mycobacteria; a standard 5-TU skin test should be applied. Appropriate management before any invasive procedures are undertaken includes eliciting a detailed history, including tuberculosis and kitten exposures, and placing a 5-TU tuberculin test.
Further history reveals that the family has recently obtained a kitten with which the child has had close contact. The patient has no history of exposure to tuberculosis, and the result of a 5-TU tuberculin skin test is negative. On closer physical examination, you note a papule on the child’s face medial to the enlarged lymph node.
11. Appropriate management at this point would include:
a) Incision and drainage of the lymph node
b) Skin test with cat scratch disease antigen
c) Therapeutic trial with azithromycin
d) No active intervention
View Answer
Answer
The answer is d. This child most likely has cat scratch adenitis. Ninety percent of patients report exposure to cats or kittens, and 75% have a history of a cat bite or scratch. B. henselae is the organism that causes cat scratch disease, and confirmation of infection can be documented with commercially available serologic testing. A cat scratch skin test, which utilizes antigen derived from human sera, is not recommended. Subacute tender regional lymphadenopathy, most commonly involving the axillae and face, is the most common clinical finding. A macule or papule at the inoculation site is found in 60% of cases (Fig. 51.2). Systemic symptoms, such as fever, are found in <35% of cases. Atypical clinical manifestations of cat scratch disease include:
Parinaud oculoglandular syndrome, which includes:
Encephalitis and encephalopathy
Neuroretinitis
Hepatosplenic disease
 Figure 51.2 A child with cat scratch adenitis. Note the papular lesion, representing the site of the bite or scratch from a kitten. (See color insert.) |
The typical course of cat scratch adenitis is benign and self-limited. Therefore, antimicrobial therapy is not indicated in most cases. Antimicrobial therapy is commonly used for severe atypical disease, such as encephalitis, although no controlled trials have assessed the efficacy of such therapy.
 Figure 51.3 The conjunctival granuloma of Parinaud oculoglandular syndrome, a manifestation of cat scratch disease. (See color insert.) |
Questions 12-13
A 6-year-old girl with nephrotic syndrome presents with abdominal pain and fever. She is taking prednisone 30 mg/day. She has no diarrhea or vomiting. Her abdominal pain has gradually worsened during the day and is now severe. On physical examination, she has a temperature of 38.4°C (101°F), pulse rate of 140/minute, respiratory rate of 40/minute, and blood pressure of 90/60 mm Hg. She is ill-appearing and apprehensive. Her abdomen is distended, with guarding and rigidity. Bowel sounds are absent.
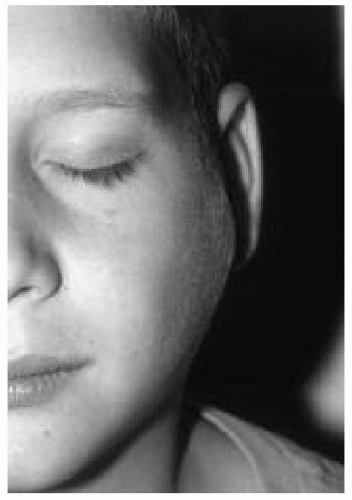 Figure 51.4 The preauricular lymphadenopathy of Parinaud oculoglandular syndrome, a manifestation of cat scratch disease. (See color insert.) |
White blood cell (WBC) count = 14,000/mm3
Hemoglobin = 9.0 g/dL
Platelet count = normal
Serum sodium = 130 mmol/L
Blood urea nitrogen = 23 mg/dL
Creatinine = 0.8 mg/dL
12. The most likely diagnosis is:
a) Acute appendicitis
b) Bacterial gastroenteritis
c) Spontaneous peritonitis
d) Bacterial pneumonia
e) Intussusception
View Answer
Answer
The answer is c. The history and clinical features are most consistent with primary spontaneous peritonitis. This entity is extremely rare in healthy children; it occurs in children with underlying ascites resulting from nephrotic syndrome, liver disease, or rheumatic disorders. Children receiving corticosteroid therapy, which may mask the clinical features of peritonitis, are at highest risk. The organisms most commonly reach the peritoneum by hematogenous spread. Paracentesis is the procedure of choice to confirm the diagnosis; a large number of polymorphonuclear cells (>250/μL), a protein level >1 g/dL, a glucose level <50 mg/dL, and the presence of only gram-positive organisms with Gram staining are features that favor a diagnosis of primary peritonitis.
13. Paracentesis confirms the presence of spontaneous bacterial peritonitis. Of the following, the most appropriate antibiotic regimen for this child is to administer:
a) Ampicillin
b) Gentamicin and metronidazole
c) Nafcillin
d) Ceftriaxone
e) Clindamycin
View Answer
Answer
The answer is d. E. coli and S. pneumoniae are the most common causes of primary peritonitis. Other, less common organisms include group A streptococci and Klebsiella pneumoniae. Anaerobes are not commonly isolated from the peritoneal fluid of patients with primary peritonitis, as they are present in secondary peritonitis. Therefore, antimicrobial therapy should include coverage against pneumococci and other streptococci in addition to coverage against gram-negative aerobes. Because a large percentage of E. coli organisms produce β-lactamases, ampicillin monotherapy is not adequate for initial therapy. The aminoglycosides provide good coverage against gram-negative aerobes but not against
pneumococci. Metronidazole is not required for initial therapy because anaerobes are not common pathogens in primary peritonitis. Nafcillin and clindamycin have no activity against gram-negative organisms. Ceftriaxone provides excellent activity against gram-negative aerobes and S. pneumoniae and should be sufficient even for penicillin-resistant strains of pneumococci.
pneumococci. Metronidazole is not required for initial therapy because anaerobes are not common pathogens in primary peritonitis. Nafcillin and clindamycin have no activity against gram-negative organisms. Ceftriaxone provides excellent activity against gram-negative aerobes and S. pneumoniae and should be sufficient even for penicillin-resistant strains of pneumococci.
14. Which of the following is a true statement regarding the treatment of acute otitis media (AOM) in infants and children?
a) Amoxicillin has the best activity of any oral β-lactam in treating nonsusceptible strains of S. pneumoniae.
b) Clindamycin is an appropriate choice for initial empiric therapy.
c) High dosages of amoxicillin are recommended to overcome resistance caused by β-lactamase-producing organisms.
d) The advantage of amoxicillin-clavulanate over amoxicillin is improved activity against nonsusceptible strains of S. pneumoniae.
e) Macrolide antibiotics, such as azithromycin and clarithromycin, are considered first-line agents.
View Answer
Answer
The answer is a. Appropriate antimicrobial therapy for AOM must take into account the pathogens involved and their resistance patterns. The three most common causes of AOM are S. pneumoniae, nontypable H. influenzae, and M. catarrhalis. H. influenzae and M. catarrhalis induce β-lactamases as their mechanism of resistance, which cannot be overcome by increasing the dosage of a β-lactam antibiotic agent. In contrast, resistance by the pneumococcus is mediated by altered penicillin-binding proteins, which is a stepwise process that can be overcome by increasing the dosage of β-lactams. On the basis of in vitro activity and achievable concentrations in the middle ear, amoxicillin is the most active of the oral β-lactams for the treatment of nonsusceptible strains of S. pneumoniae. The addition of clavulanate to amoxicillin adds a β-lactamase inhibitor to counter the effects of β-lactamases produced by H. influenzae and M. catarrhalis, but provides no added activity against S. pneumoniae. Although clindamycin has activity against S. pneumoniae and has been utilized to treat resistant pneumococcal infections, it does not have activity against H. influenzae and M. catarrhalis, and is therefore not recommended as initial empiric therapy. The macrolide antibiotics should not be used as first-line therapy for AOM, given the increasing rates of resistance against these agents, which is as high as 30% for strains of S. pneumoniae. These agents should be utilized as alternatives in patients who have severe allergies to β-lactam agents.
15. A 1-month-old girl presents with a 1-week history of upper respiratory symptoms, cough, recurrent episodes of gagging, and post-tussive emesis. On further questioning, the mother informs you that the infant often turns blue during the episodes of coughing and gagging. Physical examination findings are normal except for conjunctival hemorrhage. Complete blood cell count shows a WBC count of 38,000/mm3 with 85% small lymphocytes and a platelet count of 670,000/mm3. Which of the following is the most likely cause of the infant’s symptoms?
a) Group B streptococcal pneumonia
b) Cystic fibrosis
c) Bordetella pertussis infection
d) EBV infection
e) Cytomegalovirus (CMV) infection
View Answer
Answer
The answer is c. B. pertussis infection in young infants is associated with many of the features described in the case study. In neonates with pertussis, the classic paroxysmal cough may not be apparent, and the catarrhal stage is frequently absent or brief. These infants often present with feeding difficulties, recurrent episodes of gagging, apnea, bradycardia, and cyanosis. Apnea can follow episodes of coughing and gagging or can occur spontaneously during the course of the illness. Posttussive emesis is very common at all ages. Laboratory features of pertussis include a leukocytosis with absolute lymphocytosis, the degree of which parallels the severity of the illness. The lymphocytosis consists of small T and B lymphocytes (Fig. 51.5) rather than the atypical-appearing lymphocytes of infectious mononucleosis. Thrombocytosis is common in children with pertussis infection. The differential diagnosis of pertussis includes:
Adenovirus infection
Bordetella parapertussis infection
Viral bronchiolitis
Cystic fibrosis
Bacterial pneumonia
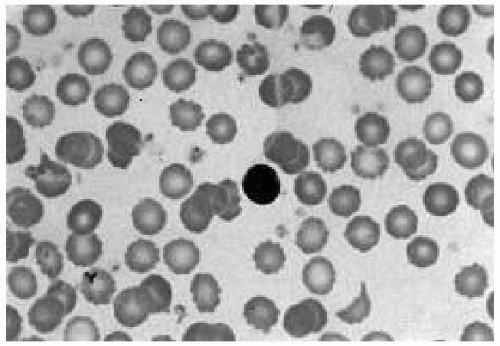 Figure 51.5 Blood smear of a child with Bordetella pertussis infection. The lymphocytosis of pertussis is characterized by normal small lymphocytes, whereas large atypical lymphocytes accompany infectious mononucleosis of viral causes. (See color insert.) |
16. A 12-year-old boy presents with a 2-week history of fever, sore throat, anterior and posterior cervical lymphadenopathy, and splenomegaly. You suspect infectious mononucleosis. Which of the following statements is true regarding infectious mononucleosis?
a) The presence of atypical lymphocytes is specific for EBV and not seen with other causes of infectious mononucleosis, such as CMV.
b) Heterophil-positive mononucleosis occurs with EBV infection but not with CMV infection.
c) Older children and adolescents are more often asymptomatic than younger children.
d) The presence of antibodies against Epstein-Barr nuclear antigen is indicative of acute infection.
View Answer
Answer
The answer is b. Heterophil antibodies are produced in EBV infection but not infectious mononucleosis syndromes with other causes, such as CMV or Toxoplasma, and in human immunodeficiency virus infection. The rapid spot tests (monospot slide tests) are highly sensitive and specific for EBV infection in older children. However, the antibodies may be absent in young children with EBV infection, and the diagnosis may require specific EBV serology. Absolute lymphocytosis with atypical lymphocytosis is not specific for EBV infection; it can be seen in infectious mononucleosis with other causes. Children <2 years are most commonly asymptomatic. Children, in comparison with adolescents, more frequently have nonspecific symptoms, such as fever, rash, abdominal pain, and upper respiratory symptoms. Older children and adolescents have more classic, mononucleosis-like symptoms. Antibodies to the nuclear antigen of EBV are produced 4 weeks after acute infection, are indicative of past infection, and persist for life. Immunoglobulin M (IgM) antibodies to the viral capsid antigen are produced early in the course of infection, are indicative of acute infection, and last for weeks to months. IgG antibodies to the viral capsid antigen are produced at the time of acute infection and last for life. Antibodies to the early antigen are produced acutely, disappear, and can reappear spontaneously.
17. Which of the following is true concerning the complications of infectious mononucleosis?
a) Severe thrombocytopenia occurs in approximately 50% of patients.
b) Cranial nerve palsies and encephalitis are the most common neurologic complications.
c) Corticosteroids are indicated for patients with neurologic or hematologic complications.
d) A clinically apparent hepatitis is evident in most patients.
View Answer
Answer
The answer is b. Facial nerve palsies and encephalitis are the most common neurologic complications of infectious mononucleosis. Others include Guillain-Barré syndrome and transverse myelitis. Mild thrombocytopenia occurs in up to 50% of patients with infectious mononucleosis. Mild autoimmune hemolytic anemia and granulocytopenia can also occur. Although mild subclinical hepatitis is common in infectious mononucleosis, severe hepatitis and liver failure are extremely rare and are seen in patients with X-linked lymphoproliferative disorder. Corticosteroid therapy for patients with infectious mononucleosis is indicated only in cases of severe airway obstruction secondary to tonsillar hypertrophy.
18. The organism responsible for the infection of the infant in Figure 51.6 is most likely to be recovered from which of the following?
a) Nasopharynx
b) Blood
c) Urine
d) Skin lesion
e) Cerebrospinal fluid (CSF)
View Answer




Answer
The answer is a. This infant has staphylococcal scalded skin syndrome (SSSS), a toxin-mediated process caused by circulating exfoliative toxins of S. aureus. The organism is very rarely recovered from the blood or bullous lesions because it is the toxin elaborated by the organism that is responsible for the epidermolysis. The organism most commonly is found in the nasopharynx, conjunctivae, umbilicus, or at the site of previous trauma or surgery, such as circumcision. SSSS is most common in infants and children <5 years. Malaise, fever, and tender skin are the first signs of infection, followed by diffuse erythema, a wrinkled appearance of the skin, circumoral erythema, and flaccid blisters. Facial edema and perioral crusting are common. Desquamation of the skin occurs 2 to 5 days after the onset of the erythema, representing cleavage of the stratum granulosum layer of the epidermis. The Nikolsky sign is separation of the epidermis by gentle shear force. The absence of a strawberry tongue in SSSS can help in differentiating this entity from systemic
skin infections caused by group A streptococci. Infants with SSSS generally appear well except for irritability likely caused by skin tenderness. Treatment with systemic antistaphylococcal antibiotics is indicated.
skin infections caused by group A streptococci. Infants with SSSS generally appear well except for irritability likely caused by skin tenderness. Treatment with systemic antistaphylococcal antibiotics is indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


