Blood Pressure Support
GENERAL CONCEPTS
Physiology of Blood Pressure in the Neonate
Neonatal Blood Pressure Support and Physiology of Blood Pressure
Caring for a critically ill neonate often requires the provider to consider the physiology, goals, complications, and pharmacologic methods of increasing a newborn patient’s blood pressure. Although various methods and medications are available to increase systemic blood pressure, few human data convincingly support the common practices for blood pressure support in adult intensive care unit, pediatric intensive care unit, or neonatal intensive care unit (NICU).1–11 This chapter describes the physiology of systemic blood pressure in the neonate, defines the pharmacologic target receptors, and presents the medications most commonly used to raise blood pressure.
Cardiac Output, Systemic Vascular Resistance, and Blood Pressure
Systemic blood pressure is determined by the product of cardiac output and systemic vascular resistance (SVR). Cardiac output is determined by the product of heart rate and stroke volume; stroke volume is determined by the preload, afterload, and contractility of the myocardium. Derangements in any of these parameters can produce hypotension in the neonatal patient. It should be noted, however, that simply increasing the blood pressure may not achieve the desired physiologic effect if the goal is to increase organ blood flow and oxygen delivery. Blood pressure and systemic blood flow are poorly correlated in the newborn,12,13 reflecting the importance of SVR in the neonate. Importantly, the neonate has unique physiology that must be understood when considering systemic blood pressure. Because of a relatively noncompliant myocardium, neonates are more dependent on heart rate to generate cardiac output than adults.14–17 Also unique to neonates are the transitional circulation immediately following birth, less-functional cerebral autoregulation mechanisms, the potential state of prematurity, and the ongoing maturation of the myocardium and vascular bed.18–20
Defining Neonatal Hypotension
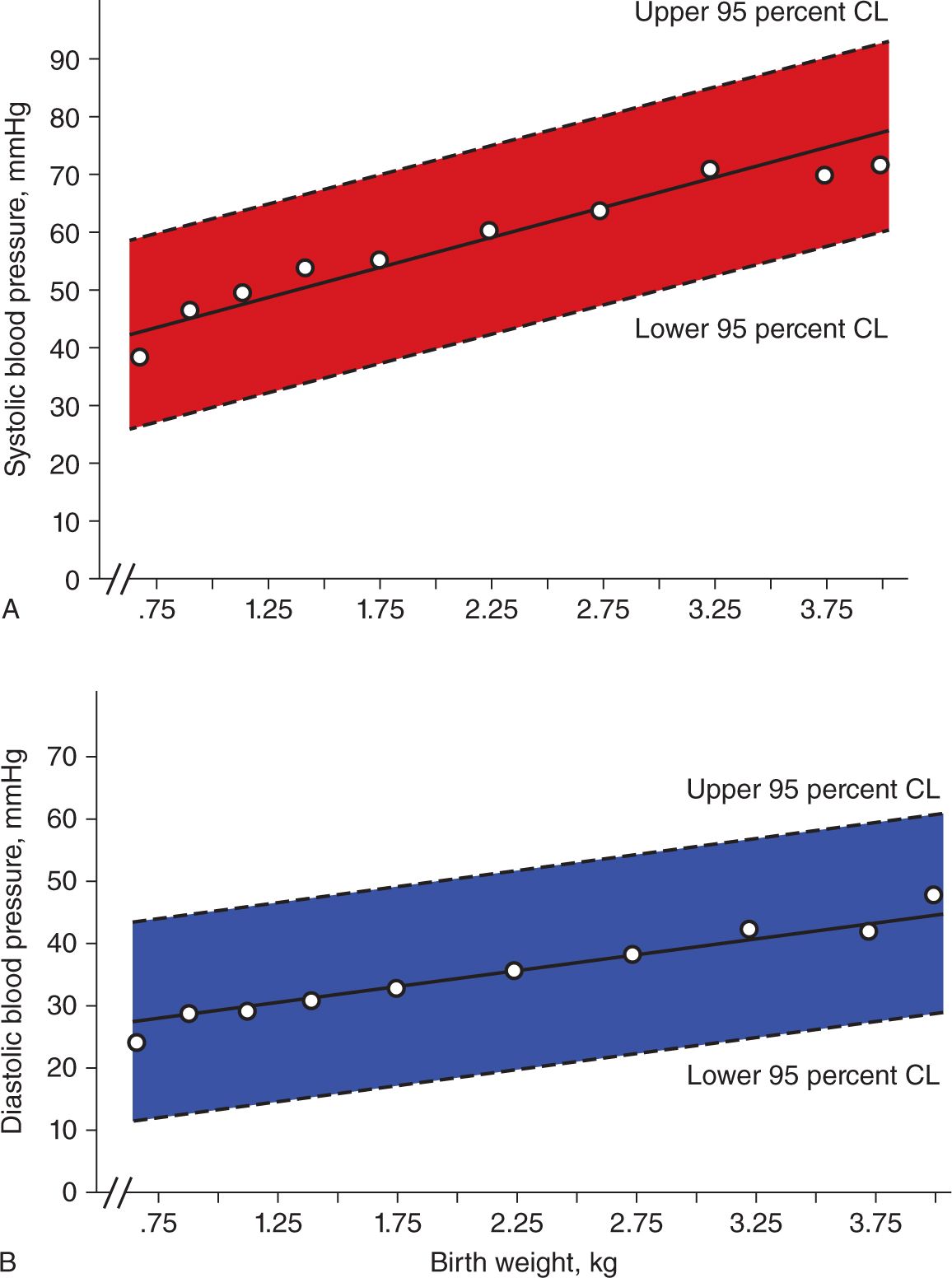
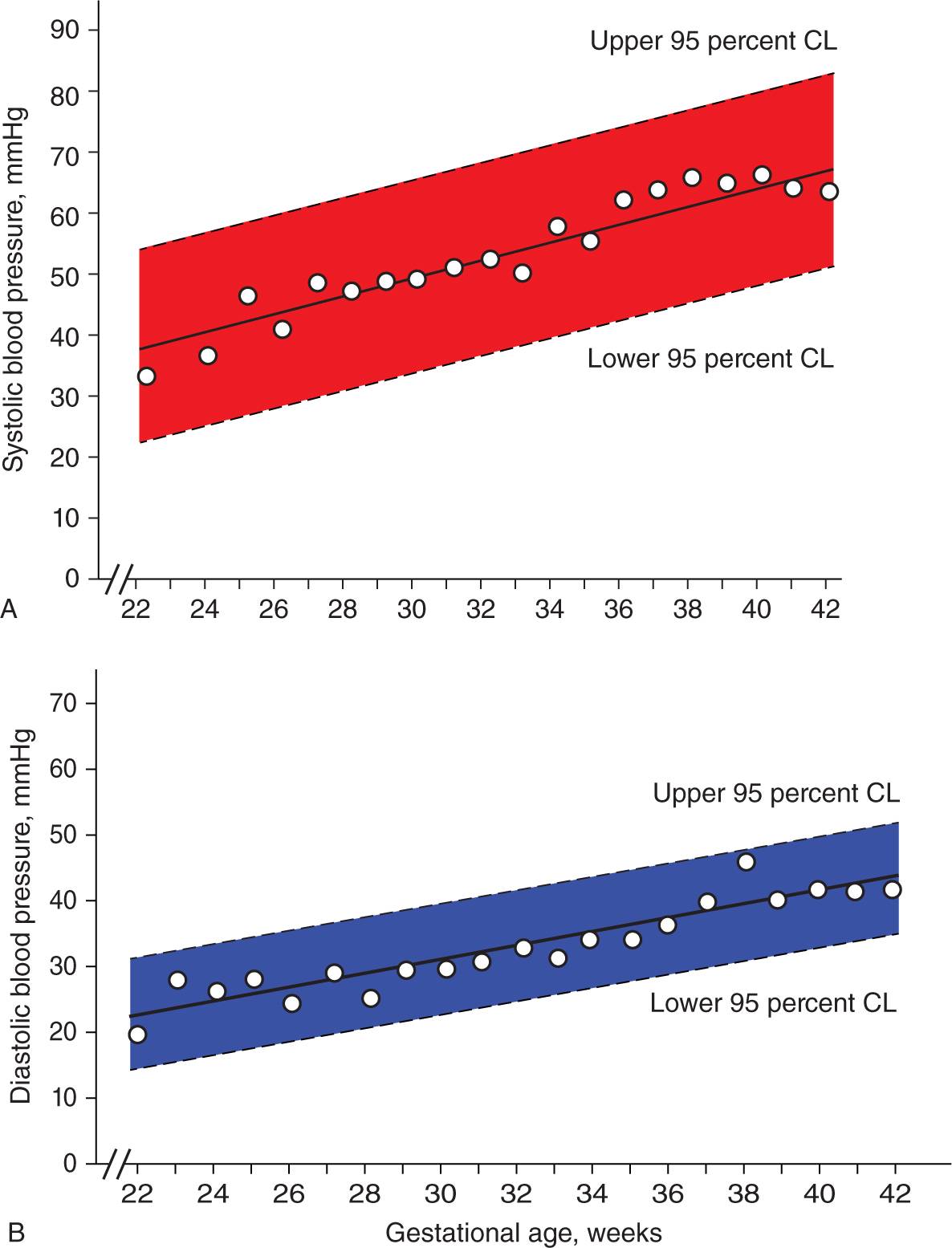
The definition of hypotension in the newborn continues to challenge the clinician. “Mean arterial pressure greater than or equal to gestational age” frequently is touted as a guideline for minimum acceptable blood pressure for a neonate, but few data exist to support this practice.21–27 Clinicians often use both gestational age and birth weight as guidelines for estimating expected blood pressure in a neonate (Figures 82-1 and 82-2). In principle, the blood pressure must be adequate to deliver oxygen to the tissues and support delivery of nutrients to the organs (most importantly the brain and heart) while removing toxic waste products from cells. The inability to achieve adequate tissue oxygen delivery and waste removal defines neonatal shock. Blood pressure is clearly inadequate if organs are poorly perfused (eg, leading to acute kidney injury or necrotizing enterocolitis [NEC]) or if biochemical markers indicate inadequate perfusion (eg, elevated lactate or base deficit on blood gas analysis).
FIGURE 82-1 Linear regression of mean systolic (A) and diastolic (B) blood pressure vs birth weight in 329 newborns admitted to the neonatal intensive care unit on day of life 1. CL; confidence limit. (Reproduced with permission from Zubrow et al.25)
FIGURE 82-2 Linear regression of mean systolic (A) and diastolic (B) blood pressure vs gestational age in 329 newborns admitted to the neonatal intensive care unit on day of life 1. (Reproduced with permission from Zubrow et al.25)
The goal of managing neonatal hypotension should be to maximize oxygen delivery and minimize oxygen consumption, thereby providing the optimal oxygen supply/demand ratio. A detailed discussion of oxygen content, delivery, consumption, and extraction ratio is beyond the scope of this chapter.18,28 Although defining hypotension is difficult, data in the premature neonate have correlated hypotension with intraventricular hemorrhage, poor neurodevelopmental outcomes, and death, thus highlighting the importance of adequate tissue perfusion in these patients.1,27,29–34 Further study of neonatal blood pressure and cerebral blood flow using superior vena caval flow measurement or near-infrared spectroscopy (NIRS) may help define what an “adequate” blood pressure is for a given newborn.26,35
Differential Diagnosis of Neonatal Hypotension
The differential diagnosis of inadequate tissue perfusion (including “hypotension” and “low-output states”) in the newborn is broad and varies based on the gestational age of the patient. The most common causes of shock and hypotension are hypovolemia (including placental hemorrhage or organ hemorrhage in the perinatal period); infection (sepsis, NEC); extreme prematurity; perinatal asphyxia; severe pulmonary disease (often with pulmonary hypertension); adrenal crisis/insufficiency; large left-to-right shunts (most commonly a large patent ductus arteriosus); and poor cardiac function (because of pump failure, arrhythmias, and obstructive congenital cardiac lesions, among others).6–9,11,22
Echocardiography is a noninvasive tool to assess cardiac structure and function in the hypotensive neonate. Cardiac pathology, such as left-sided obstructive lesions, a large patent ductus arteriosus, and poor myocardial contractility, can be delineated by an echocardiogram. These findings may lead the clinician to initiate inotropic agents sooner or modulate blood pressure in other ways when appropriate (eg, initiating prostaglandins in a ductal-dependent lesion such as critical aortic stenosis).
Treatment of hypotension (ie, blood pressure support) necessitates understanding the physiologic abnormality and the primary cause of the patient’s abnormal physiology. Maintaining intravascular volume (with saline or albumin infusions) is supported by physiologic principles, but it has not been shown to improve systemic blood flow compared to pharmacologic support.36,37 However, it is common practice to ensure adequate volume administration before initiating inotropes, and most inotropes and pressors require an adequate preload volume to augment blood pressure effectively. The remainder of this chapter focuses on the principles of pharmacologic management of hypotension.
PHARMACOLOGIC BLOOD PRESSURE SUPPORT
Inotropes and Vasopressors
The mainstays of pharmacologic treatment of neonatal hypotension remain inotropes and vasopressors, with the former defined as agents that increase the force of myocardial contraction and the latter defined as agents that increase blood pressure by constricting the arterial vasculature (ie, increasing SVR).2,3,9,10,38,39 (Vasodilators may also increase systemic blood flow, but they usually do not increase blood pressure and thus are not discussed here.) Inotropes are classified as sympathomimetics (eg, dopamine), phosphodiesterase inhibitors (eg, milrinone), and cardiac glycosides (eg, digoxin); their mechanism of action is to increase intracellular calcium concentration, thus increasing the force of myocardial contraction. Also frequently used are agents that increase heart rate (chronotropes), improve myocardial relaxation (lusitropes; phosphodiesterase inhibitors), and medications that work by other mechanisms to increase blood pressure (steroids, calcium, thyroid hormone). When initiating inotropes or vasopressors, the clinician must consider methods of monitoring intravascular volume status and the effectiveness of pharmacologic therapy. Blood pressure should be measured by an invasive arterial catheter (peripheral or umbilical) when a patient requires multiple interventions for the treatment of hypotension. Similarly, volume status should be measured with central venous access to confirm adequate cardiac preload.
Adrenergic Receptor Subtypes
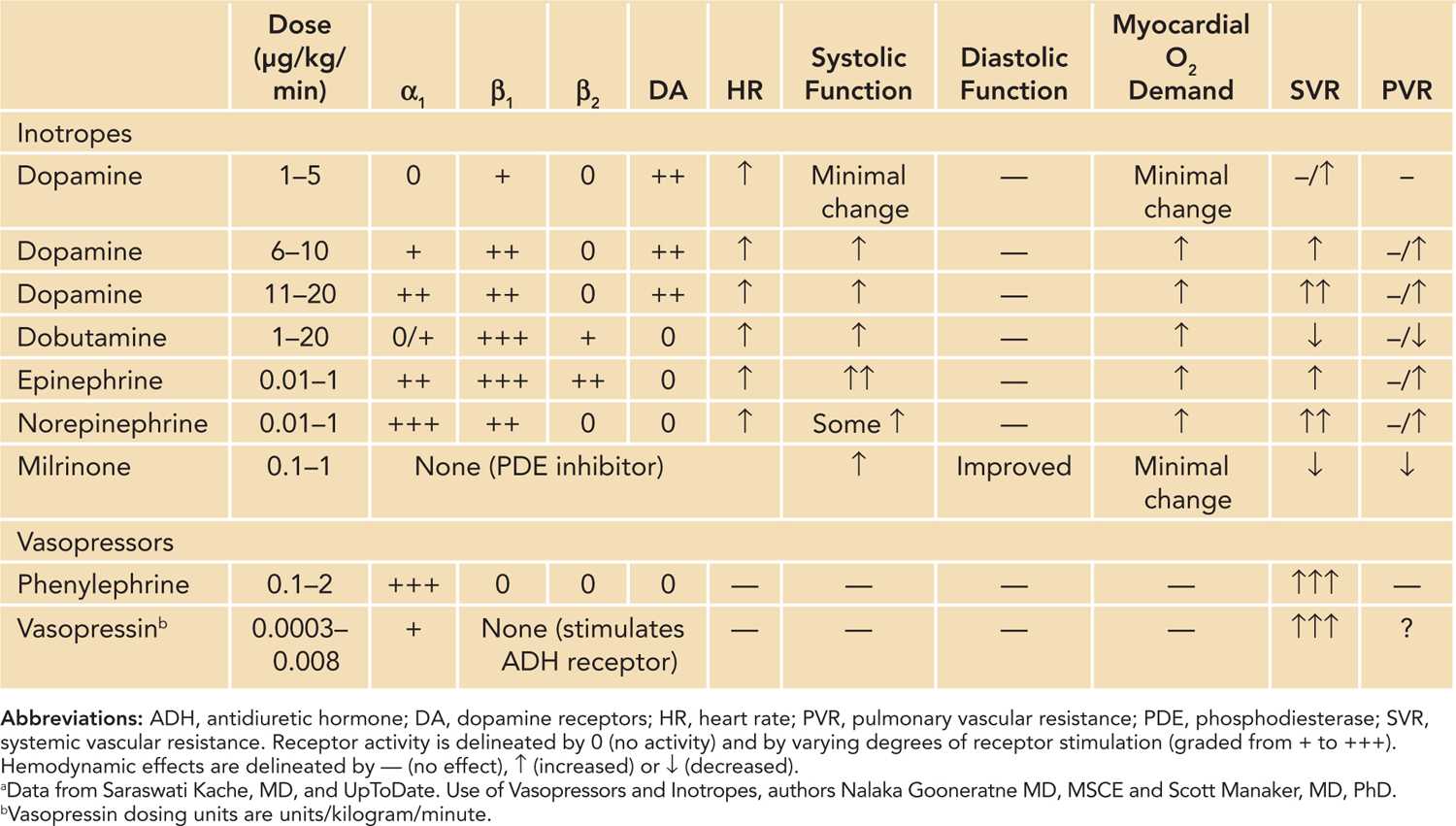
To understand the actions of these medications, it is critical that the provider recall the receptor subtypes which are activated on the cell membrane. The relevant subtypes are the α1, β1, and β2 adrenergic receptors and the dopamine receptors.9,39–41 The α1-adrenergic receptors, when activated in vascular walls, promote vasoconstriction; α1-stimulating medications elevate blood pressure by increasing SVR. The α1 receptor has also been found in the myocardium, and its activation increases cardiac contractility.42 Animal data also suggest that receptors in the right ventricle may differ from those in the left ventricle, thus promoting the specific targeting of right ventricular strain in clinical scenarios such as pulmonary hypertension.43 Activation of β1-adrenergic receptors promotes increased inotropy and chronotropy (without vasoconstriction); β1-stimulating medications increase blood pressure by increasing cardiac output. The β2-adrenergic receptors promote vasodilation in the cardiovascular system and bronchodilation in the lung. Dopamine receptor stimulation promotes dilation of the cardiac, gastrointestinal, and renal vascular beds via dopamine 1 (DA-1) receptors and of the peripheral vascular bed through dopamine 2 (DA-2) receptors. Stimulation of dopamine receptors can also induce norepinephrine release and act as a vasoconstrictor (see the discussion that follows). A summary of pharmacologic receptor subtype activity, mechanism of action, and hemodynamic effects for the most commonly used inotropes and vasopressors is included (Table 82-1).
Table 82-1 Inotropes and Vasopressors: Receptors and Hemodynamic Effects
SPECIFIC AGENTS FOR BLOOD PRESSURE SUPPORT IN THE NEONATE
The pharmacologic agents for blood pressure support have been studied in human neonates; however, controversy still exists regarding which inotrope or vasopressor is preferred for a given patient. The following is a description of the primary mechanism of action, indications, side effects, and physiologic properties of the most commonly used blood pressure medications. Not described in this chapter are steroids, which have been studied in neonatal septic shock44–51 and are included in the Surviving Sepsis Campaign and guidelines for the management of pediatric and neonatal septic shock.52,53
Dopamine
Dopamine is a drug commonly used in neonates to treat hypotension from a variety of medical or surgical causes (especially postoperative cardiac).10,11,54,55 Dopamine’s effect on blood pressure is mediated via direct stimulation of β1 receptors on the myocardium along with the indirect effect of increasing norepinephrine, which stimulates α1 receptors.56–58 In animal studies, neonatal myocardium has been shown to have more dopamine receptor sensitivity compared to adult myocardium.59,60
Frequently discussed is the dose-response curve of dopamine on the cardiovascular system.55,61 At doses of 1–3 μg/kg/min, the effects are primarily vasodilation of the cerebral, coronary, renal, and gastrointestinal vascular beds via stimulation of DA-1 receptors and dilation of peripheral vascular beds via DA-2 receptors. Doses in the range of 5–15 μg/kg/min are often referred to as “inotropic range” dosing because the stroke volume is increased with less effect on heart rate. As dosing increases in this range, there are increasing β1 (elevated heart rate) and α1 (elevated SVR) effects. Above 20 μg/kg/min, dopamine acts mainly on α1 receptors; it increases inotropy but may compromise blood flow by elevating vascular resistance in the kidney, periphery, and gastrointestinal system, among others.54,62–65
Dopamine can cause cardiac dysrhythmias (most commonly sinus tachycardia), vasoconstriction, tissue necrosis with extravasation, and immunosuppression with prolonged use. It has been shown to alter the production of prolactin by the hypothalamus.55 In select populations, dopamine has been shown to increase oxygen consumption more than oxygen delivery,66 and it may increase pulmonary artery pressure in premature newborns with a patent ductus arteriosus.67 Studies in premature and term neonates have compared dopamine to volume administration,68 dobutamine,35,65,69–73 epinephrine,74,75 phosphodiesterase inhibitors,76,77 and steroids.78 These data suggest that dopamine augments blood pressure and may increase renal and mesenteric blood flow. However, based on current data, it cannot be recommended for use over other agents.
A large adult study recently compared dopamine to norepinephrine for the treatment of shock; although no difference in mortality was detected, dopamine resulted in significantly more side effects, such as cardiac arrhythmias.79 These data suggest that dopamine is effective at increasing blood pressure,11,55,57,62,72,80 but whether it improves mortality, morbidity, or neurodevelopmental outcomes is unclear.11,13,35,37,81
Dobutamine
Dobutamine (1–10 μg/kg/min), a synthetic catecholamine, stimulates predominantly β1 receptors with very little α or β2 stimulation.2,3,6,7,10,11 Dobutamine, like dopamine, may exhibit a clinically significant dose-response curve. At doses less than 5 μg/kg/min in children, heart rate does not increase, but cardiac output and blood pressure increase, and left atrial pressure decreases. Heart rate increases at doses greater than 7.5 μg/kg/min.82 Dobutamine increases inotropy and heart rate and decreases SVR, thus increasing cardiac output and organ blood flow. Decreasing SVR may lower blood pressure; for this reason, dobutamine is mainly used for myocardial dysfunction without severe hypotension. Dobutamine also decreases ventricular filling pressure, pulmonary vascular resistance (PVR), and SVR more effectively than dopamine.83 Dobutamine does not stimulate norepinephrine release, which also differentiates it from dopamine.
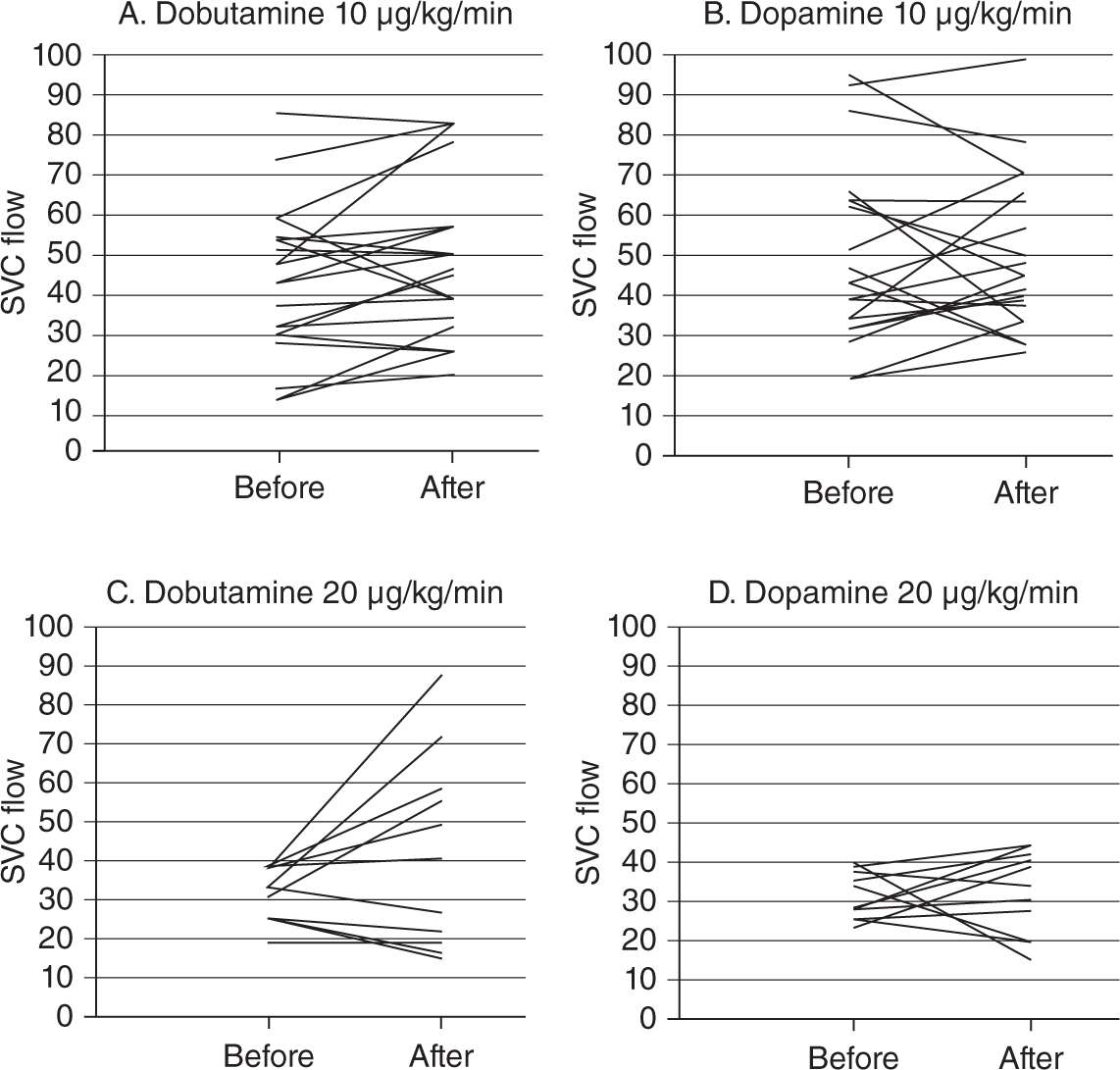
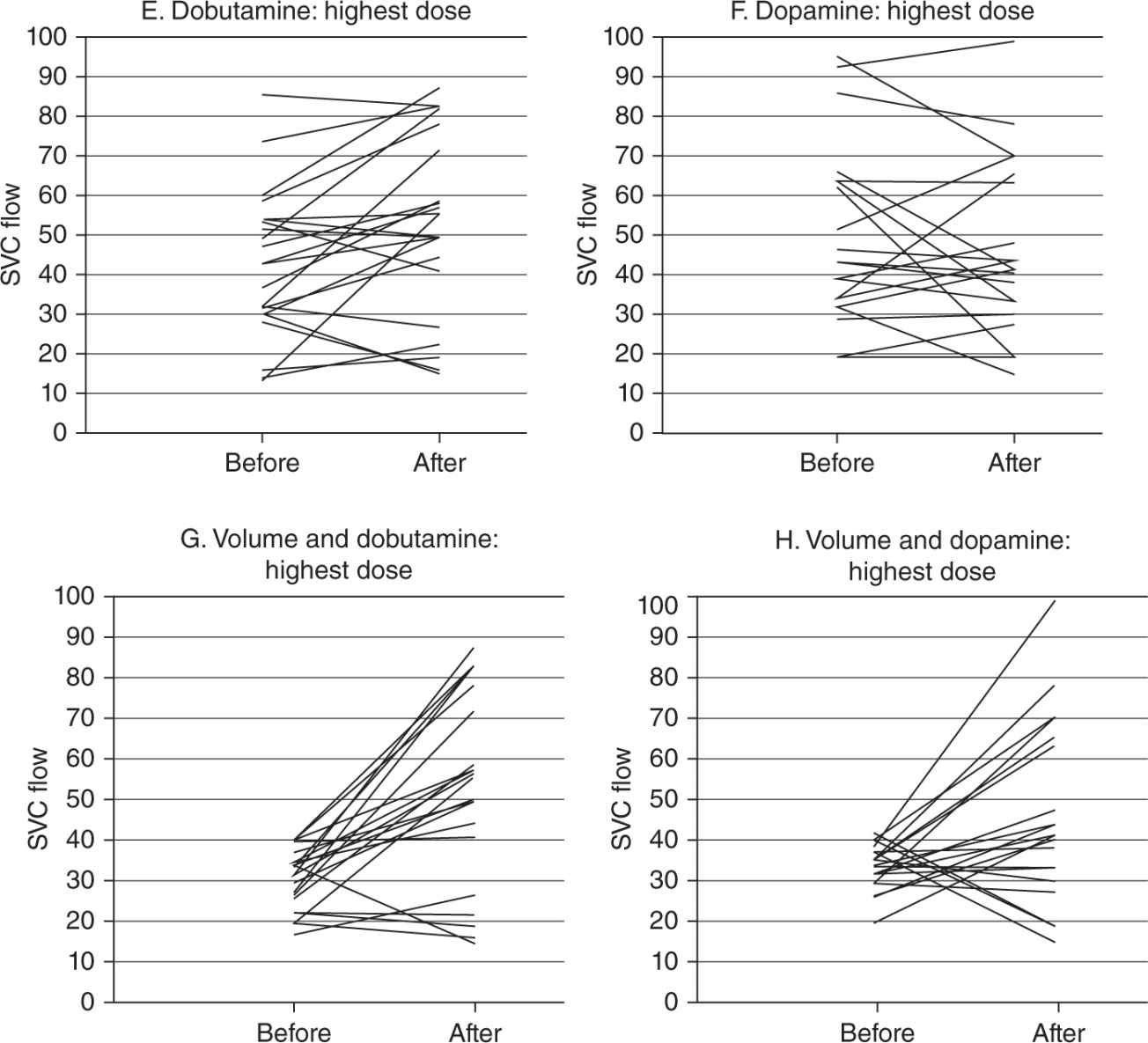
Intestinal perfusion in preterm neonates increases with dobutamine infusion.62 Data in preterm neonates suggest that dobutamine may be superior to dopamine in increasing systemic blood flow71,72 (Figures 82-3, 82-4), but conflicting data suggest that dopamine increases blood pressure more effectively.13,69–71 It remains unclear which inotrope is superior in the premature or term newborn in the NICU,7,13,71–73 and neurodevelopmental outcomes appear similar after blood pressure support with both agents.35 Because dobutamine does not stimulate β2 receptors and has less chronotropic effect, indications for use include patients with systolic dysfunction and normal blood pressure and who are at risk for dysrhythmias. A study in children after cardiopulmonary bypass (CPB), however, revealed little reduction in SVR and significant tachycardia.84
FIGURE 82-3 Superior vena cava (SVC) flow, a surrogate for oxygen delivery to the brain, as measured in neonates receiving dopamine vs dobutamine (each at lower and higher doses). Only higher-dose dobutamine increased SVC flow. (Reproduced with permission from Osborn et al.72)
FIGURE 82-4 Superior vena cava (SVC) flow, a surrogate for oxygen delivery to the brain, as measured in neonates receiving dopamine vs dobutamine, each at high doses (E, F) and then with volume administration (G, H). High-dose dopamine and dobutamine increased SVC flow when administered with volume, illustrating the need for adequate volume resuscitation with inotrope administration. (Reproduced with permission from Osborn et al.72)
Epinephrine
Epinephrine is a potent, endogenously produced adrenergic stimulator that strongly activates the β1 receptor and moderately activates the β2 and α1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree