Fig. 23.1
An example of an offset cystoscope. The working channel is straight so that the injection needle is not bent
The ideal injectable material for the urinary tract is nonmigrating, durable, biocompatible, nontoxic, noncarcinogenic, nonteratogenic, easily injectable, and affordable. The first injectable material used to treat urinary incontinence was Teflon (PTFE-polytetrafluoroethylene) in 1985 [3], but it is now not in use due to risks of distant particle migration and granuloma formation. After Teflon, glutaraldehyde cross-linked bovine collagen (Zyplast, Contingen), silicone particles (polydimethylsiloxane) (Macroplastique), dextranomer particles in 1 % sodium hyaluronan solution (Deflux), synthetic calcium hydroxyapatite particles in glycerine, and sodium carboxymethylcellulose (Coaptite) have been developed for injection.
Transurethral injection of the male bladder outlet is technically easier than the female outlet, primarily due to the differential urethral length. The short female urethra makes stabilizing a cystoscope and simultaneously positioning and injecting the bulking agent somewhat challenging. To address this issue, a non-endoscopic periurethral injection device was created for adult females, called the Zuidex system (Q-Med, Uppsala, Sweden) [4–7]. The Zuidex system consists of a special implacer, which is a device that mounts four 21 G needles and four syringes of Zuidex (gel of dextranomer microspheres and nonanimal stabilized hyaluronic acid (NASHA)). The implacer has four lateral holes for the insertion of four needles. A protective sheath covers the needles during sheath insertion into the urethra. Once in the midurethra, the sheath is retracted, exposing the needles and permitting lateral needle movement. Each needle and syringe is individually positioned submucosally and the Zuidex is injected. One short-term report on three females suggests its usefulness in girls as well [8], but the system has been withdrawn from the market due to its low efficacy and periurethral abscess formation resulting in urethral obstruction requiring multiple surgeries for a satisfactory voiding [9–11]. A recent review has noted that the success rate of a blind midurethral paraurethral bulking agent injection is less than the success rate of cystoscopically guided proximal urethra or bladder neck injection [12].
Operative Technique
Multiple approaches have been described, depending on (1) from where the leakage is occurring (transurethral leak or continent catheterizable stoma leak) and (2) the postsurgical anatomical configuration (open versus closed bladder neck or presence versus absence of continent catheterizable channel). Three basic options include (1) the retrograde transurethral approach, (2) the antegrade approach via a catheterizable channel, or (3) the suprapubic access approach (Figs. 23.2 and 23.3). Perineal paraurethral approaches for transurethral leaking have basically been abandoned.
Fig. 23.2
Potential operative approaches to the child with transurethral urinary incontinence due to bladder outlet intrinsic deficiency
Fig. 23.3
Potential operative approaches to the child with urinary incontinence via catheterizable stoma
Transurethral Leak
Retrograde Transurethral Approach
The patient is in the dorsal lithotomy position. The lubricated cystoscope is introduced into the urethra and bladder, inspecting for additional anomalies and bladder neck appearance. In males, the needle is inserted submucosally at the level of verumontanum and advanced to the bladder neck [13]. Recently, injection below the verumontanum is also advocated [14]. In females, the scope is positioned in the midurethra, and the needle injection occurs submucosally from bladder neck to the midproximal urethra. Circumferentially, the injection sites may be at two symmetrical points [15], at three points [16], or at multiple points [13]. Regardless of the injection number, the aim is to see complete coaptation of the bladder neck and proximal urethra (Fig. 23.4).
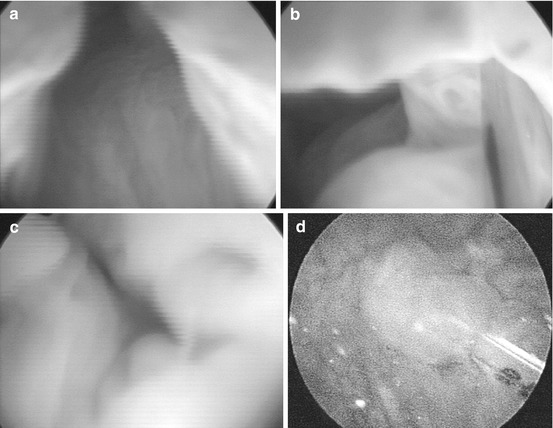
Fig. 23.4
Bladder neck injection for urinary incontinence. (a) Transurethral view of incompetent keyhole bladder neck. (b) Via the transurethral cystoscope, Deflux was injected into the bladder neck area. (c) After transurethral bladder neck injection, the urethral mucosa appears coapted. (d) A cystoscope was passed into the appendicovesicostomy, and the bladder neck injection site is viewed
Antegrade Approach
This approach is performed via the continent catheterizable channel. With the patient in the supine position, the lubricated cystoscope is introduced into the catheterizable tunnel with careful manipulation not to harm the continent channel. The bladder neck and posterior urethra are inspected. The injection needle is introduced submucosally at the bladder neck and advanced towards the verumontanum if it can be seen in males and towards the midurethra in females.12 Injection can be done at two [17], three, or four points to obtain a well-coapted bladder neck.
Antegrade Suprapubic Access Approach
This is an alternative and adjunctive technique to gain temporary suprapubic puncture access to the bladder via a 2 mm laparoscopic trocar. The injection needle is inserted into the laparoscopic trocar, and antegrade bladder neck injection is observed via a cystoscope in the continent catheterizable channel [18]. Injection is done as described above. Since the procedure is done through a laparoscopy port, it has been reported to be performed at the same session with laparoscopic antegrade continence enema with no additional complications [19].
Leak via Catheterizable Channel
Catheterizable Channel Injections
These injections can be approached and performed in a similar fashion as that for transurethral leaking [20]. It is convenient to position the patient in the lithotomy position to permit simultaneous access to the channel and the urethra.
Antegrade Approach via Continent Catheterizable Channel
With the cystoscope in the channel, the walls and opening of the channel into the bladder are inspected. The needle is introduced submucosally 2–3 cm from the orifice and advanced to the orifice at the bladder. Injection is slowly performed until the whole proximal channel wall is elevated including the orifice at the bladder. Injection can be repeated at multiple locations circumferentially until the whole intramural channel is coapted [21].
Retrograde Transurethral Approach
With the cystoscope placed transurethrally, the orifice of the catheterizable channel in the bladder is inspected. The needle is placed into either the patulous channel at 6 o’clock position or a few millimeters below the orifice and advanced further along the intramural channel. Injection is continued until the orifice elevates and is coapted.
Antegrade Suprapubic Access Approach
If a cystoscope cannot be passed via urethra (impassable urethral strictures or closed bladder neck), the suprapubic access approach as described above can be performed temporarily.
Urine should be continuously diverted by an indwelling catheter for 7–14 days postoperatively. However, it should not be placed via the site of injection so as to avoid molding of the injection mound. Thus, a suprapubic tube may be necessary.
Postoperative Management
Bladder outlet injection is an outpatient procedure. Continence is expected to be regained or improved right after the injection, or sometimes it may take a few months until the bladder grows under increased bladder outlet pressure. The length of follow-up after a successful bladder neck injection is variable. Long-term duration of implant is different for every material. The published series with the longest follow-up period reported is 13 years (mean 7 years); they observed the highest recurrence of incontinence within first year [14, 22], particularly in the first 6 months (79 % vs. 56 %) [23]. They concluded that failure after 1 year is significantly related to deterioration of bladder dynamics and requires urodynamic investigations. [24] VCUG can be done to detect de novo VUR after increased bladder outlet resistance in case of febrile UTIs [25].
Complications
Since different materials have different material-specific complications such as migration of implanted particles to lungs and brain for Teflon, teratogenicity of silicone particles, and complete volume loss of collagen, only common complications of bladder neck injection will be covered in this section.
A recent report has demonstrated an interesting complication of submucosal calcifications in 4 of 31 children who underwent bladder neck injection with glutaraldehyde cross-linked collagen as the bulking agent. They found that calcifications at the bladder neck or urethra appear more than 7 years after very high volume injections (mean 21 cc) [26]. A similar complication has been reported from the periurethral injection of hyaluronic acid and dextranomer particles. Severe periurethral abscesses obstructing the bladder outlet have occurred following periurethral injection with Zuidex leading to its withdrawal from the market. However, a similar complication has not been reported yet following bladder neck injections that are performed with cystoscopic guidance [9].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


