Bladder and Cloacal Exstrophy
The exstrophic anomalies, often referred to as the exstrophy–epispadias complex,1 are considered a spectrum of embryological abnormalities including:
• Epispadias—the least severe anomaly, in which the urethra is a partial or complete open plate on the dorsal surface of the phallus
• Classic bladder exstrophy (BE)—the most common of these anomalies, in which the bladder is an open plate on the lower abdomen and always includes epispadias
• Cloacal exstrophy (CE)—the bladder and the ileocecal junction of the bowel are an open plate on the lower abdomen. This condition, commonly associated with other defects, is also known as the omphalocele/exstrophy/imperforate anus/spinal defect (OEIS) complex
• Exstrophy variants—partial manifestations are seen of the above anomalies, and commonly lack symmetry in the sagittal plane.
Bladder Exstrophy
Classic BE occurs in one per 10,000–50,000 live births,2,3 with a male to female ratio of 3–6 : 1.4,5 CE is even more rare with an incidence of 1 in 200,000–400,000,6 but is more common when stillborns are included in the data (1 in 10,000 to 1 in 50,000).7 The natural history of BE is well known; the anomaly is nonlethal although it is associated with significant morbidity. Since the 19th century, various efforts to manage BE have been described. As the condition is rare, these approaches were empiric and usually unsuccessful. Until the 20th century, there was no effective surgical technique.
BE results from an anterior herniation of the developing bladder and urethra with subsequent herniation of posterior developing structures, preventing the normal development of the lower abdominal wall and anterior fusion of the pelvis. The result is a flattened pelvis with wide diastasis of the symphysis pubis. This anomaly has been described as ‘if one blade of a pair of scissors were passed through the urethra of a normal person; the other blade were used to cut through the skin, abdominal wall, anterior wall of the bladder and urethra, and the symphysis pubis; and the cut edges were then folded laterally as if the pages of a book were being opened’ (Fig. 58-1).8 Children with BE typically have an anteriorly located anus. Also, the female genital anatomy is altered with a more vertically oriented vaginal opening following repair and a wider and shorter vagina than normal. The anterior component of the penis is also foreshortened in males compared to the general population. Classic BE, however, is rarely associated with other organ system malformation.
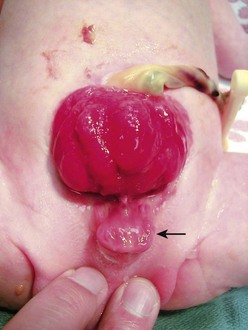
FIGURE 58-1 Bladder exstrophy in a male. The urethral mucosa is marked with the arrow. The corporeal bodies lie posterior to the urethral mucosa.
Diagnosis
BE can be diagnosed antenatally, although many affected fetuses are not identified before birth.9 Ultrasound (US) can reliably detect BE before the twentieth week of gestation.10,11 Absence of the bladder is the hallmark. Other ultrasound findings include:
• A semisolid mass protruding from the abdominal wall12
• A lower abdominal protrusion
• An anteriorly displaced scrotum with a small phallus in male fetuses
• Normal kidneys in association with a low-set umbilical cord13
Subtle findings such as low umbilical cord insertion and the location of the genitalia will only be seen if the fetus is examined in a sagittal alignment with the spine.14 As exstrophy affects the external genitalia, the diagnosis is easier to make in males than females. Iliac crest widening can also be seen during the routine prenatal evaluation of the lumbosacral spine to evaluate for myelomeningocele. The iliac angle will be about 110° rather than the usual 90°.14 Since urine production is normal in these fetuses, amniotic fluid levels are normal.
Prenatal diagnosis allows for prenatal counseling, optimal perinatal management, and the chance to be delivered near a pediatric center trained to treat these babies. This counseling should include the expertise of an experienced pediatric urologist or surgeon. The overall prognosis for these children can be good if treated at medical centers with experience with this disorder.15
In many areas of the developing world, early treatment remains problematic due to the lack of healthcare infrastructure and resources to care for these patients. Management of these patients often includes significantly delayed time to closure and adds another level of challenge to achieve optimum outcomes in this patient group. A recent overview from South Africa highlighted this problem: 58% of the patients presented in a delayed fashion and mortality rates approached 42% due to concomitant medical conditions and poor primary health care.16
Pathogenesis
In the prescientific era, the cause of BE was attributed to trauma to the unborn child causing ulceration of the abdominal wall and subsequent bladder herniation. Today, we know that the developing human embryo does not normally pass through a stage that corresponds to exstrophy. This knowledge excludes arrested development and implicates an error in embryogenesis involving the cloacal membrane.17 This membrane serves to separate the coelomic cavity from the amniotic space in early development and can be identified by two to three weeks of gestation. By the fourth gestational week, it forms the ventral wall of the urogenital sinus with the unfused primordia of the genital tubercles sitting cephalad and lateral to it. With further development, the primordia grow and fuse in the midline, and mesoderm grows toward the midline creating an infra-umbilical abdominal wall. Simultaneously, the urorectal septum develops medially and caudally to separate the cloaca into the urogenital sinus and rectum.18
One theory suggests a persistent cloacal membrane during fetal development.19 Persistence of this membrane could create a wedge effect that keeps the medially encroaching mesoderm from fusing in the midline.17 To further study this hypothesis, an animal model of CE was created using the developing chick embryo. By placing a plastic graft in the region of the tail bud, it was found that CE resulted, perhaps due to persistence of the cloacal membrane.17
Other experimental models implicate the cloacal membrane as well, but postulate that early disruption, rather than persistence, causes exstrophy. Another model of CE in the developing chick embryo, created by using a CO2 laser to create an early dehiscence in the tail bud caudal to the omphalomesenteric vessels, suggests that exstrophy may result from failure of the mesodermal ingrowth between the ectoderm and endoderm of the cloacal membrane which then later ruptures. It is hypothesized that such an event could be caused by early hypoxemic infarction in the region of the tail bud with subsequent cellular loss of the mesoderm followed by herniation of the developing bladder or cloaca.20 This type of ischemic injury has been implicated as the cause of gastroschisis and could explain the spectrum of the exstrophy/epispadias complex. Another possible mechanism resulting in a similar pathophysiology could be a defect in a genetic switch which results in premature senescence of the infra-umbilical membrane (analogous to an ischemic injury). This mechanism would imply an epigenetic basis for exstrophy.
Other proposed theories include caudal displacement of the paired primordia of the genital tubercles. Exstrophy is postulated to occur by this mechanism when the primordia of the genital tubercles fuse caudal to their usual location relative to where the urorectal fold divides the cloaca into the urogenital sinus and rectum.21 This theory readily explains the spectrum of variation seen in the exstrophy. However, it fails to explain the higher incidence of exstrophy compared to epispadias.8
A relatively new maldevelopment theory for CE is based on a suramin-exposed chick model.22 When chick embryos were examined at one or two days after pericardial injection of suramin, about 8% were noted to have a midline infra-umbilical opening into the cloaca and allantois, abnormal leg bud abduction, hypoplastic tail and allantois, a broad infra-umbilical pelvic region, and large aneurysmal dilation of the paired dorsal aorta at the level of the leg buds. The aortic dilation is transient, resolving on the second or third day after drug exposure. These authors implicate the aneurysmal paired dorsal aorta as the primary defects leading to CE in this animal model. Pelvic maldevelopment has also been implicated in the pathogenesis of exstrophy and explains both the bony abnormalities as well as soft tissue anomalies.23
The chick model to study BE has inherent limitations. Unlike primates, chickens possess a cloaca; thus this precludes the creation of BE versus CE. Other animal models to study BE have been difficult to create. In an exstrophy sheep model, a significant increase in the ratio of collagen-to-smooth muscle was noted in exstrophic versus normal control bladders (P < 0.05). These histological changes are similar in part to changes seen in human BE specimens.24,25
To date, the underlying cause of human exstrophy remains in question perhaps secondary to environmental exposure, an infectious pathogen, or other causes in genetically susceptible individuals. In fact, epidemiologic studies implicate a role for inherited susceptibility. As a result of the associated physical anomalies with this condition, patients with BE often have to overcome significant obstacles to reproduce. Men may need to resort to assisted reproductive techniques because of difficulty with sexual intercourse and ejaculation.26,27 Women with exstrophy are prone to uterine prolapse and miscarriage. Difficulty with conception and pregnancy are still a problem today despite in vitro fertilization and careful obstetric care.28,29 These issues combined may explain, in part, why familial patterns of inheritance of exstrophy–epispadias complex are noted infrequently. To date, 37 familial cases of BE have been reported, the most recent of which describes a mother and son with BE.30 Five cases of an affected parent–child pair have also been described.30–32 Another 18 cases with BE have been found in twins.30 However, in a study population of greater than six million births and 208 reported cases of exstrophy, no case had a positive family history for this anomaly.33
Current counseling recommendations about the risk of recurrence in a sibling of a patient with exstrophy cite an estimate of about 1% and a 1 : 70 chance of transmission to the progeny of an affected parent.31 A Florida population-based study found multiple births had a 46% increased risk of birth defects, with BE being the fifth highest adjusted relative risk.34 These findings support a multifactorial etiology with evidence for genetic predisposition. More recently, an epidemiologic survey of families with BE found no link between exstrophy and parental age, maternal reproductive history, or periconceptional maternal exposure to alcohol, drugs, chemical noxae, radiation, or infections. Periconceptional maternal exposure to smoking was noted to be significantly more common in patients with CE.35
Principles of Reconstruction
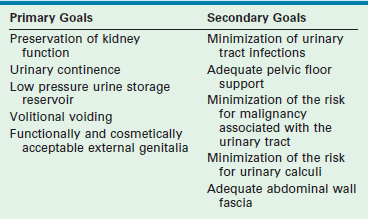
Modern objectives for exstrophy reconstruction are placed broadly into primary and secondary goals (Table 58-1).
While these goals are straightforward and often interconnected, their successful achievement can be elusive. Many of the secondary goals address complications that can arise from operations used to treat exstrophy. The goals have expanded since the first operations were attempted in the 19th century. These objectives address the primary pathophysiology of exstrophy and the problems associated with its management (Table 58-2).
TABLE 58-2
Primary Pathophysiology of Bladder Exstrophy and Complications that Occur in Relation to its Management
| Primary Pathophysiology (If Untreated) | Complications (Associated with Management of Exstrophy) |
| Malignancy (related to chronic exposure of the bladder plate) | Malignancy (related to the use of intestine in bladder reconstruction) |
| Pyelonephritis | Pyelonephritis |
| Kidney stones | Kidney and bladder stones |
| Total urinary incontinence | Stress or urge urinary incontinence |
| Chronic bladder irritation | Hydronephrosis |
| Pelvic floor insufficiency | Cystocele, uterine prolapse |
| Abnormal hip dynamics, back pain | Abnormal hip dynamics, back pain |
| Symphyseal diastasis, pelvic flattening | Urinary outlet obstruction |
| Abdominal wall defect | Absent umbilicus |
| Ventral and inguinal hernias | Incisional hernias |
| Severe penile shortening with dorsal chordee | Inadequate phallus in males with subsequent social and psychological sequelae |
Natural History and Early Attempts at Treatment
Children with BE can survive untreated and some untreated patients with BE have lived into their eighth decade.36 However, significant morbidity exists if these exstrophic conditions are left untreated, including total urinary incontinence, bladder and kidney infections, skin breakdown, and tumor development in the bladder plate. The surrounding skin around the exposed bladder is often inflamed secondary to urine contact dermatitis, loss of skin integrity from constant wetness, and secondary infection. Untreated inguinal hernias can be life-threatening and organ prolapse is especially challenging to manage later. In addition, these patients are often social pariahs because of odor and hygiene problems. In contrast, when these patients receive effective surgical and medical treatment, they can lead productive, healthy lives with manageable morbidity.
The morbidity associated with untreated BE led physicians to develop empiric operative approaches for this anomaly such as urinary reconstructive or diversion procedures. Initial efforts were directed at partial reconstruction of the abdominal wall to allow the application of a urinary receptacle to collect urine. Others performed urinary diversion through the creation of a ureterosigmoid fistula. Early results were poor.27 These early efforts were undertaken without an understanding of urinary tract and bladder physiology, or how these operations would affect urine storage and emptying, kidney function, electrolyte homeostasis, the propensity for urinary tract infection, or urinary calculus formation.
Current Operative Approaches
Urinary Diversion
Urinary diversion is not commonly used in the USA or most parts of Europe; this approach has been abandoned in favor of an anatomically based approach. However, continent urinary diversion techniques can produce a more consistent degree of urinary continence with less intervention than that achieved with anatomic reconstruction.37 Some urodynamic studies demonstrate low urine flow rates and poor contractility and continence in patients following primary bladder repair.38,39
Internal or incontinent urinary diversion avoids the potential complications associated with functional reconstruction such as urinary retention and subsequent kidney damage, and potential later dependence on clean intermittent catheterization (CIC) to empty the bladder. Advocates of early urinary diversion also cite a decreased risk of epididymitis and obstruction of the vas deferens by the creation of a receptacle with a suprapubic window at the level of the prostatic urethra.40 Diversion can also be combined with cosmetic and functional reconstructive procedures for the external genitalia. Because of the difficulties encountered with functional bladder reconstruction, advocates of early urinary diversion argue that their approach achieves the primary goals with fewer operations and higher success rates than are achieved with bladder closure and urethral reconstruction.
Given the successes of urinary diversion, why abandon it? Long-term complications associated with ureterosigmoidostomy (USO) are significant and include hyperchloremic metabolic acidosis, chronic pyelonephritis, bladder calculi, and a 250- to 300-fold increased risk of adenocarcinoma developing at the anastomosis.41–43 As a result of these complications, USO was subsequently replaced by incontinent urinary diversions such as colonic and ileal conduits. A significant disadvantage to these conduits is the incontinent abdominal stoma that is associated with them.
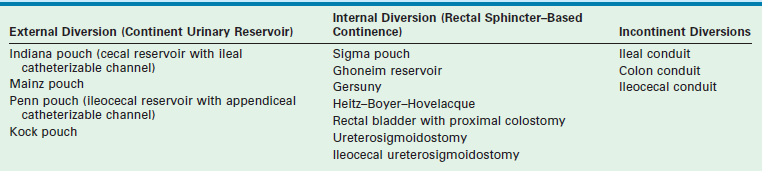
The Mainz II pouch and the Sigma pouch represent significant improvements to the USO.44–46 These rectal reservoirs permit urinary continence without reliance on CIC. In one study, renal preservation rates in children treated primarily with a urinary rectal reservoir (Mainz II pouch) approach 92% with continence rates up to 97%.37 The Heitz–Boyer–Hovelaque procedure involves isolation of a rectal segment for ureteral implantation followed by posterior sagittal pull-through of the sigmoid colon through the anal sphincter. A small series using this approach reported continence rates of 95% with an acceptable complication rate.47 Complications of this form of diversion include fecal-urinary incontinence in patients with impaired anorectal sphincter control. Metabolic electrolyte imbalances can be treated with frequent emptying of the rectal reservoir that reduces the contact time between urine and the absorptive rectal mucosa along with oral bicarbonate replacement. The significant risk of malignancy also remains a concern. Various modifications of the rectal reservoir to prevent admixture of feces and urine may decrease the incidence of adenocarcinoma if the risk is due to conversion of urinary nitrates into carcinogenic nitrites by fecal bacteria.48 Long-term results are not yet available. Techniques for constructing urinary diversions are listed in Table 58-3.
Anatomic Reconstruction
The first efforts at anatomic reconstruction for BE were unsuccessful, but set the stage for the current anatomic approach. In 1881, Trendelenberg described an exstrophy closure emphasizing the importance of pubic re-approximation in front of the reconstructed bladder in order to achieve continence and prevent dehiscence.49 However, because of discouraging results, anatomic reconstruction was largely replaced by urinary diversion in the early part of the 20th century. During this time there were scattered published reports of successful outcomes.50–53 However, several large series of patients who underwent single-stage anatomic reconstruction in the 1960s and 1970s reported continence rates of only 10–30%.54–59 Renal damage was as high as 90% in these series, generally because of bladder outlet obstruction.54
As a result of these complications and the low rate of urinary continence with single-stage approaches, reconstructive efforts were subsequently modified toward staged bladder reconstruction, an approach pioneered in the 1970s, and further refined to what is now known as the modern staged repair of exstrophy (MSRE).60–62 Recent advances in single-stage reconstruction for BE have been advocated and complete primary repair for exstrophy (CPRE) has gained favor.63
Preoperative Care
After delivery, to reduce trauma to the bladder plate, the umbilical cord should be ligated with silk suture rather than a plastic or metal clamp. A hydrated gel dressing or plastic wrap can be used to protect the exposed bladder from superficial trauma. Dressings should be changed daily, and the bladder should be irrigated with normal saline with each diaper change. A humidified air incubator may also minimize bladder injury.64
Operative Considerations
Ideally, the primary BE closure is performed in the newborn period. If the bladder template is amenable, early closure has several advantages. Early closure initiates the road toward anatomic normalcy as well as decreasing bladder exposure which can lead to histological changes such as acute and chronic inflammation, squamous metaplasia, cystitis glandularis and cystitis cystica, and muscular fibrosis which may adversely impact bladder capacity and compliance.65 Electron microscopy studies have shown that the newborn exstrophy bladder is ‘immature’ when compared to control newborns,66 and has fewer small nerve fibers,67 less smooth muscle, and a threefold increase in type III collagen content.68 While it is unclear whether these changes are part of the primary pathology or secondary to the lack of bladder cycling in utero, it is conceivable that early closure could ‘mature’ the bladder by restoring bladder cycling. Similarly, another study verified the importance of immediate postnatal exstrophy closure as infants closed before 7 days of age required fewer bladder augmentations to achieve eventual continence.69
Assessment of the adequacy of the bladder template is subjective. Even a small bladder template, if distensible and contractile, can enlarge to a useful size once closed. However, if the bladder template appears too small and stiff on initial assessment, some surgeons choose to defer early operation and re-evaluate the bladder at 4–6 months of age under anesthesia.70 If the bladder continues to appear inadequate for closure, a nonrefluxing colon conduit can be created in combination with an abdominal wall closure and epispadias repair. At a later age this can be converted to a continent diversion or anastomosed to the rectosigmoid.
During general anesthesia, nitrous oxide should be avoided during primary closure as it can cause bowel distension, which decreases exposure during the operation and may increase the risk of wound dehiscence. Some advocate postoperative nasogastric tube drainage to decrease abdominal distension although we do not routinely use it.71 We prefer an epidural catheter to reduce the inhaled anesthetic requirement during the operation. Tunneling the epidural may reduce the risk of infection if it is left in for prolonged periods after repair.72
For patients older than 3 days, or newborns with a wide pubic diastasis, we perform anterior iliac osteotomies. Osteotomies are recommended in most patients unless the pelvis is very pliable. Osteotomies assist closure and enhance anterior pelvic floor support, which may improve future urinary continence.60,73
Factors that appear to be important in the perioperative period include:
Complete Primary Repair for Exstrophy
Clinical experience in babies with posterior urethral valves suggests that early restoration of nonobstructive emptying and filling of the bladder allows the bladder to regain some of its normal physiologic and developmental potential.76 This implies that the bladder progresses through developmental milestones in the first few months of life. Precedence for this form of organ development is found in the brain with the acquisition of language and visual perception, and this is also true for skeletal and neuromuscular development. Finally, early bladder reconstruction creates a more normal appearing baby, which may foster improved bonding between the parents and infant.
In the CPRE (or Mitchell) technique,63 the bladder, bladder neck, and urethra are relocated posteriorly within the pelvis. This shift positions the proximal urethra within the pelvic diaphragm in an anatomically more normal position to maximize the effect of the pelvic muscles and support structures needed for urinary continence. Posterior location of the bladder neck and urethra also facilitates reapproximation of the pubic symphysis which, in turn, helps prevent anterior migration of the urethra and bladder neck, and provides a more anatomically normal pelvic diaphragm.
CPRE Technique: Boys.
After sterile preparation and draping, the lines of dissection are marked (Fig. 58-2). When marking these lines, it is important to exclude dysplastic tissue at the edges of the exstrophic bladder and bladder neck. This is particularly important at the bladder neck where remaining dysplastic tissue may impair later bladder neck function. Catheters (3–5 French) are placed into both ureters and sutured with 5-0 chromic suture. Bladder polyps should be removed prior to beginning the dissection as these can act as space-occupying lesions after the bladder is reconstructed. Initial dissection begins superiorly and proceeds inferiorly to separate the bladder from the adjacent skin and fascia since it is usually easiest to identify tissue planes in these areas. The umbilical vessels are ligated as the umbilicus will be moved superiorly to a more anatomically normal location, and will be later used as the location to exteriorize the suprapubic (SP) catheter.
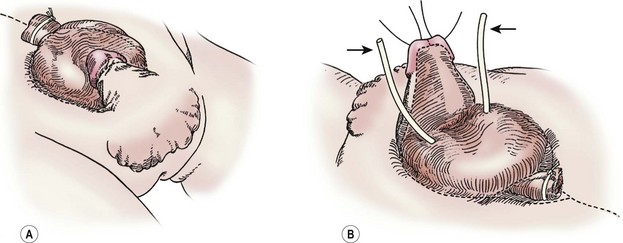
FIGURE 58-2 In a male undergoing complete primary repair for bladder exstrophy, the outlines of the planes of dissection are seen in these drawings. (A) Ventral view. (B) Dorsal view. The ureteral stents are marked with arrows.
Penile/Urethral Dissection.
Traction sutures are placed into each hemiglans of the penis to aid in dissection. These sutures will rotate to a parallel vertical orientation because the corporal bodies will naturally rotate medially after they are separated from the urethral wedge (urethral plate plus underlying corpora spongiosa). We begin the penile dissection along the ventral aspect of the penis with a circumscribing incision (Fig. 58-3A). This step precedes dissection of the urethral wedge from the corporal bodies because it is easier to identify the plane of dissection ventrally above Buck’s fascia. Buck’s fascia is deficient or absent around the corpora spongiosum. As the dissection progresses medially to separate the urethra from the corpora cavernosa, it is important to realize that the plane shifts subtly from above Buck’s fascia to just above the tunica albuginea. Failure to adjust the plane of dissection will carry the dissection into the corpora spongiosa which will result in excessive, difficult-to-control bleeding during the deep ventral dissection of the urethral wedge from the corporal bodies.
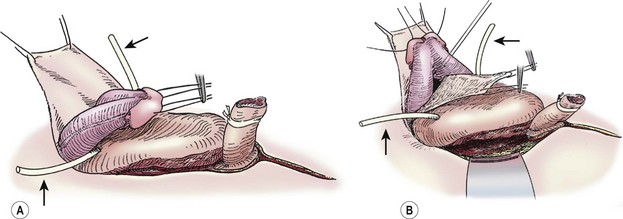
FIGURE 58-3 These two diagrams show early portions of the ventral subcoronal and corporeal dissection. (A) Initiation of the subcoronal dissection is seen. This is typically the easiest plane to initiate dissection. (B) Corporeal dissection proximally and dorsally is shown. Initiation of corporeal separation is easiest to establish proximally. Note the ureteral catheters (arrows), which have been introduced into the ureteral orifices.
Careful lateral dissection of the penile shaft skin and dartos fascia from the corporal bodies will avoid damaging the laterally located neurovascular bundles on the corpora of the epispadic penis. The lateral dissection on the penis should be superficial to Buck’s fascia because of the lateral location of the neurovascular bundles in the epispadic penis.
Complete Penile Disassembly and Deep Dissection.
Once a plane is established between the penis and the urethral wedge, the penis may be disassembled into three components: the right and left corporal bodies with their respective hemiglans, and the urethral wedge.77 This is performed in order to provide exposure to the intersymphyseal band and to allow adequate proximal dissection. We have found the easiest plane of dissection to completely isolate the corporal bodies is proximal and ventral. The plane of dissection should be carried out at the level of the tunica albuginea on the corpora (Fig. 58-3B). After a plane is established between the urethral wedge and the corporal bodies, this dissection is carried distally to separate the three components from each other (Fig. 58-4A). Complete separation of the corporal bodies increases exposure to the pelvic diaphragm for deeper dissection. The corporal bodies can be completely separated from each other since they are nourished via a separate blood supply. It is important to keep the underlying corpora spongiosa with the urethra as the vasculature to the urethra is based on this corporal tissue (which should appear wedge-shaped after its dissection from the adjacent corpora cavernosa). The urethral/corpora spongiosa component will later be tubularized and placed ventral to the corporal bodies. Para-exstrophy skin flaps should not be made with this technique because creating these flaps may injure the blood supply to the distal urethra. As the bladder and urethra are located posteriorly in the pelvis as a unit (with a common blood supply), division of the urethral wedge is counter-intuitive to the intent of the repair.
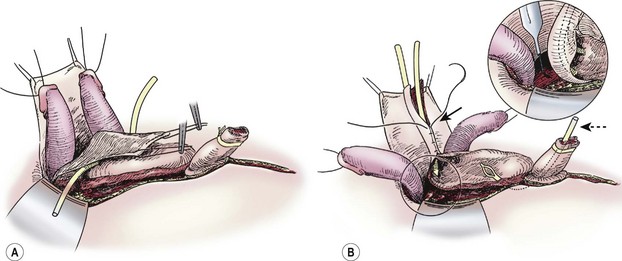
FIGURE 58-4 (A) Separation of corporeal bodies and urethra. (B) Deep pelvic dissection. Note the division of the intersymphyseal band (inset) is critical to allowing placement of the bladder in the pelvis. Also note the tubularization of the neourethra over the urethral catheter (solid arrow) and the suprapubic tube in the still-open bladder (dotted arrow).
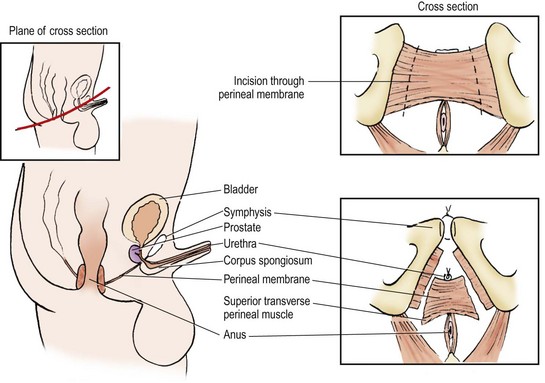
After separating the components distally, the urethral dissection is carried proximally to the bladder neck. Exposure to the pelvic diaphragm is optimized by complete proximal separation of the urethra and corporal bodies (Fig. 58-4B). This creates the exposure to perform the deep incision of the intersymphyseal band (the condensation of anterior pelvic fascia and ligaments) which is necessary to move the bladder and urethra posteriorly (Fig. 58-5). When dissecting the urethral wedge from the corporal bodies medially, the dissection plane is along the tunica albuginea of the corpora cavernosa. This medial dissection should be carried down through the intersymphyseal band.
With a deep incision of the intersymphyseal band posterior and lateral to each side of the urethral wedge, the bladder and bladder neck can be moved to a posterior position in the pelvis. This dissection should be carried until the pelvic floor musculature becomes visible and the future bladder neck and proximal urethra lie deep in the pelvis with little anterior tension. Failure to adequately dissect the bladder and urethral wedge from these surrounding structures will prevent posterior movement of the bladder in the pelvis and will create anterior tension along the urethral plate, all of which can lead to failure of the closure (Fig. 58-5).
Primary Closure.
Once the above steps are completed, the bladder closure and urethral tubularization can be initiated. This portion of the repair is straightforward and anatomic (Fig. 58-6A). To provide urinary drainage, an SP tube is used. The bladder is closed in three layers with monofilament absorbable suture. The urethra is tubularized using a two-layer running closure with monofilament and braided absorbable suture. Because of the previous deep dissection, we can now position the tubularized urethra ventral to the corpora without tension. If the urethra cannot be positioned ventrally without creating tension and restricting the urine flow, it may be necessary to more aggressively incise the intersymphyseal band and pelvic diaphragm.
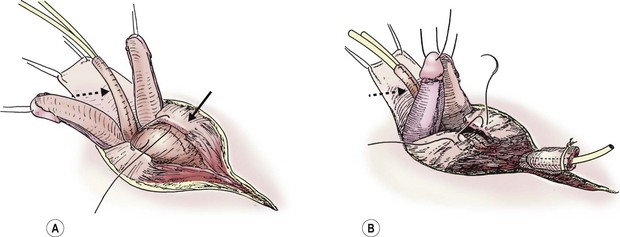
FIGURE 58-6 Once the intersymphyseal band is adequately incised and the bladder and urethral wedge are dissected from the surrounding tissues, bladder repair and urethral tubularization can be performed. (A) The bladder is being closed in three layers using monofilament absorbable suture (solid arrow). The urethra has been tubularized using a two-layer running closure with monofilament and braided absorbable suture (dotted arrow). (B) This schematic depicts closure of the pubic symphysis with two number 1 polydioxanone interrupted sutures placed in a figure-of-eight fashion. The knots are placed anteriorly to prevent suture erosion into the neck of the bladder. The urethra (dotted arrow) has been placed ventral to the corpora.
The pubic symphysis is reapproximated using two large polydiaxanone (PDS) interrupted sutures (Fig. 58-6B). Knots are left anteriorly to prevent erosion into the bladder neck. The rectus fascia is reapproximated using an interrupted or running 2-0 PDS. We also place interrupted 6-0 PDS sutures along the distal dorsal aspect of the corporal bodies to reapproximate them. Penile skin coverage is achieved with either a primary dorsal closure or reversed Byars flaps if needed. The skin covering the abdominal wall is reapproximated using a two-layer closure with absorbable monofilament suture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree