Fig. 3.1
Positioning and port placement for robotic left renal procedures
Pelvic and Bladder Surgeries
Positioning children for bladder procedures should begin by placing a Foley catheter into the bladder. The patients during bladder procedure are placed at the end of the operating table in a lithotomy position with stirrup supports and a slight Trendelenburg angle. The patient should be provided with sufficient foam padding at all pressure points to prevent injury. The robot will dock from the foot of the table, between the patient’s legs. Of importance, the camera swinging during the foot-docked robot position may come near the patient’s face, and thus adequate foam padding protecting the face and airway is critical (see Fig. 3.2).
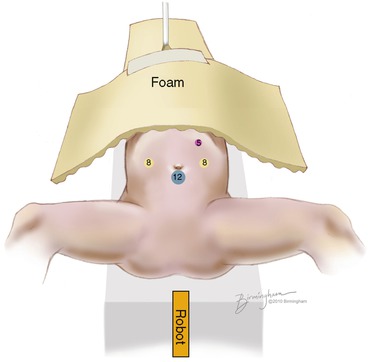
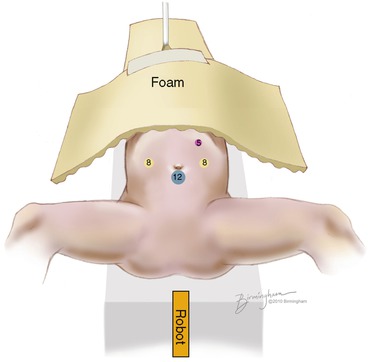
Fig. 3.2
Port placement and positioning for pelvic procedures
Port Placements
Port placement for all robotic surgeries requires an initial insufflation of the peritoneal cavity and the subsequent placement of working and assistant ports. The preferred approach for initial insufflation in pediatric cases is the open Hasson technique. Initial insufflation is set to 10–15 mmHg of carbon dioxide. Nitrous oxide is not preferred given the potential for intestinal distention and loss of visualization. A trocar is inserted for the 12 mm/8.5 mm camera port via the preferred technique [14].
Two 8 mm instrumentation ports are generally used during operation. Ports are placed after pneumoperitoneum is achieved and under direct vision with a 0° flat or 30° upward-facing lens. The ports are placed midline 6–10 cm superior and inferior to the umbilicus for renal surgeries or laterally 6–10 cm away from midline at or above the level of the umbilicus. If the patient’s umbilicus to pubic symphysis distance is below 10 cm for pelvic procedures, the camera port should be moved to a supraumbilical position. Adequate spacing (6–10 cm) between ports and the camera is critical to prevent collision. Newer models of the DVSS robot (S and Si) tolerate closer spacing between ports. An additional 5 mm assistant port is often useful for needle delivery and can be placed as described in the included diagrams.
After port placement surgery, the pneumoperitoneum pressure should be reduced to 12 mmHg (10 mmHg for infants), and the pressurized carbon dioxide should be connected to the assistant port to prevent fogging. After instrument change, the pressure of the pneumoperitoneum reliably drops. Reinsufflation should proceed to maintain 12 mmHg during operation.
Visualization and Instrumentation
High-definition visualization is a hallmark of modern robotic-assisted laparoscopy. Three sizes of endoscopes are available on the DVSS: 5 mm (discontinued production), 8.5, and 12 mm. The 5 mm scope allows for a 2D monocular view, whereas the 8.5 and 12 mm endoscopes allow for 3D views with binocular vision. Warming the endoscopes prior to insertion into the pneumoperitoneum as well as attaching the carbon dioxide tubing to the assistant port will help limit fogging of the visualization.
Instrumentation on the da Vinci machine allows for a wrist-like 7 degrees of freedom, which is particularly helpful for complex laparoscopic maneuvers such as suturing. In addition, due to motion control algorithms, movements of the instrumentation are tremor-free. Both 5 and 8 mm instruments are available, yet 8 mm is often preferred by the author due to ease of use and geometrical limitations of angulation of the 5 mm instruments. Currently, the 5 mm instruments require an additional 2 cm of intracorporeal working distance over the 8 mm instruments. The increased distance is a limiting factor in the pediatric population and has discouraged the use of 5 mm instrumentation. The 8 mm instruments include a large needle driver, Maryland bipolar forceps, curved and straight scissors, scalpels, bi- and monopolar cautery instruments, ultrasonic energy instruments, and laser cutters. Appropriate miniaturization of the instrumentation is anticipated in future releases and may facilitate operating in tight anatomical spaces.
Training and Team Building
Adequate robotic training and meaningful mentorship is important for the development of skilled robotic surgeons. Currently, no standardized robotic training curriculum in pediatric urology for practicing pediatric urologists is universally accepted. Nevertheless, specialized fellowships, cadaveric laboratory experience, and one-on-one training with an experienced robotic surgeon provide opportunities for training. At our institution, we have designed a 5-day immersive training mini-fellowship for pediatric urologists worldwide [14]. The curriculum includes hands-on supervised training in the laboratory, simulation, dry skills, and didactic lectures. For basic robotic skills, virtual training simulation such as the Robotic Surgical Simulator (RoSS) developed by Simulated Surgical Systems LLC has proved popular among practicing robotic surgeons as a training tool [15]. Also, simulators packaged with the SI dual console DVSS have been useful in training regimens. For more specialized training, the use of a mentor and formalized training has been shown in conventional laparoscopy to impact the learning curve as well as maintenance of the skills in future practice [16].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


