Bacterial Pathogenesis
Janet R. Gilsdorf and Carl F. Marrs
Bacteria possess a number of characteristics that facilitate the lifestyle of the organism representing a variety of functional activities, including transmission from host to host, attachment to host cells and tissues, invasion of host tissues, facilitation of growth in specific host environments, or avoidance of host defenses by immune evasion and intracellular growth. Occasionally, these factors may be related, either directly or indirectly, to damage and disease in humans and are then called virulence factors.
HOST–BACTERIAL RELATIONSHIPS
Bacterial infections are the result of complex interactions between the bacteria causing the infection and the human host in which the infection occurs. These host–bacterial interactions, known as the damage framework,1 occur in a continuous dynamic and are summarized as follows:
1. Exposure of the host to the bacteria is required for the initiation of bacterial disease and occurs in a variety of ways, such as skin exposure through direct cutaneous contact, respiratory tract exposure through inspiration, or intestinal exposure through ingestion.
2. Acquisition of the bacteria occurs in the face of a direct interaction with the host, often through specific adherence mechanisms by which the organisms bind to specific receptors on human skin or mucosal surfaces.
3. Persistence of bacteria in or on the human host is a factor of time (as short as minutes or as long as a lifetime), during which the bacteria remain attached to the host cells or tissues and host–bacterial interactive processes, such as adherence, engulfment, intoxication, or immunity, may occur. The persistence of bacteria in or on the host, with bacterial replication, is infection.2 A state of mutualism between host and bacteria with no host damage is called commensalism. Colonization represents the continuum of persistence ranging from absence of damage (commensalism) to stimulation of the host immune response leading to immune damage.
4. Damage is the effect of the bacteria on the host and is the means by which disease occurs. The damage may result directly from bacterial factors, such as toxins, or from host immune factors stimulated by the presence of the bacteria.
5. Disease is the clinical manifestation (ie, symptoms) of damage to the host related to the bacterial infection.
6. Immunity is the host response to the presence of the bacteria and may involve either the innate or the adaptive immune system. Although immunity may protect the host from future infection or may contribute to clearance of the bacteria, it may also contribute to damage to the host cells or tissues.
7. Clearance of the bacteria from the human host may occur during multiple states in the host–bacterial interaction and may result from a variety of processes, such as bacterial detachment with loss of adherence to host cells, shedding of bacteria with desquamation of host cells, or immune-mediated bacterial lysis or phagocytosis.
Different bacteria interact with human hosts in many different ways within the spectrum of host–bacteria interaction states. Commensalism, which involves exposure to, acquisition of, and asymptomatic persistence of microbes, as well as infection, which involves a specific bacterial interaction with the host, may or may not ultimately result in damage and disease. The outcome depends on many bacterial and host factors and on multifactorial regulation of the host–microbe interactions, as summarized in Table 222-1.
Table 222-1. Bacterial and Host Factors Contributing to Host–Microbial Interactions
Bacterial factors that contribute to infectious diseases |
Attachment factors |
Invasive factors |
Metabolic pathways and growth factors |
Antigenic variation (immune evasion) |
Toxic molecules |
Stimulation of immune response with resulting |
host damage |
Antibacterial resistance |
Host factors that contribute to infectious diseases with bacteria |
Disruption of mechanical barriers to infection |
Alteration of physiologic barriers to infection |
Inadequacy of innate immunity |
Inadequacy of adaptive immunity |
PATHOGENICITY AND VIRULENCE
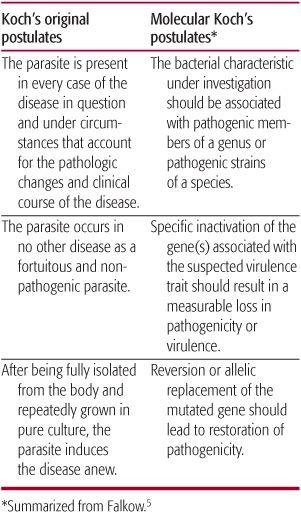
On the advent of the germ theory of disease, physicians and scientists began to associate specific diseases with specific bacteria. The accumulation of medical knowledge revealed, however, that many microbes live in and on humans and that most human infections are caused by only a few of the organisms. The pathogenicity (ie, the ability to cause an infection) of a bacterium and, thus, its virulence (ie, a comparative measure of pathogenicity) is not a finite quantity and can only be defined in the context of the host.3 Thus, the probability of disease caused by a specific bacterium is a function of both the pathogenic capability of the bacteria and the integrity of the host defenses, with exposure as a cofactor. The previous guideline for establishing microbial causation of infections (Koch’s postulates) did not account for this variation in host. Moreover, over the years, these postulates have been modified to reflect the prevailing concepts of bacterial pathogenesis, natural history, and infections, and the availability of whole genome sequences, resulting in the establishment of Molecular Koch’s Postulates (see Table 222-2).5
HOST SUSCEPTIBILITY/RESISTANCE TO INFECTIONS
The pathogenesis of bacterial infections must take into consideration the defenses available to the host because these defenses, which vary in their integrity from patient to patient, must be breached for infection to occur. The healthy human body possesses many physical barriers to the establishment of bacterial infections, including skin, mucous membranes, and mechanical clearance mechanisms, as outlined in eTable 222.1  . Either inherent or acquired abnormalities in the host’s physical or physiologic barriers, innate immunity, or adaptive immunity (see Chapter 186) may be associated with the increased ability of bacteria to cause infection. Each of these is also discussed in further detail in additional text on DVD.
. Either inherent or acquired abnormalities in the host’s physical or physiologic barriers, innate immunity, or adaptive immunity (see Chapter 186) may be associated with the increased ability of bacteria to cause infection. Each of these is also discussed in further detail in additional text on DVD.
BACTERIAL INFECTIVITY
Many bacterial characteristics and the factors responsible for those activities contribute to the ability of bacteria to infect humans and cause disease. Bacterial growth is imperative for bacterial infectivity and requires the availability of optimal nutrients, temperature, hydration, osmolality, and pH, as well as a conducive environment that is free of antibacterial forces. In addition, the probability that a bacterial agent will cause infection and disease depends on the bacterial infectious dose, on tissue tropism, and a number of specific bacterial pathogenic factors.
Specific bacteria appear to have an affinity to inhabit/infect specific body sites, a characteristic called tissue tropism. For example, Staphylococcus aureus and Streptococcus pyo-genes frequently cause skin and soft tissue infections as well as osteomyelitis in children but rarely cause meningitis or urinary tract infections. Similarly, Haemophilus influenzae type b cause meningitis and septic arthritis in nonimmune children but rarely cause urinary tract or bone infections, and Escherichia coli frequently cause urinary tract infections but rarely cause septic arthritis or osteomyelitis.
GENETICS OF BACTERIAL VIRULENCE FACTORS
 ORGANIZATION OF BACTERIAL GENOMES
ORGANIZATION OF BACTERIAL GENOMES
Genes essential for bacterial growth under all environmental conditions are normally located on the bacterial chromosome. In addition, genes encoding important bacterial functions, including pathogenic factors, may also be found on other genetic elements, such as plasmids, phages, and transposons.
Plasmids are extrachromosomal elements that replicate separately from the bacterial chromosomes. Besides the plasmid genes needed for replication and maintenance of the plasmid within bacteria, genes found on plasmids often benefit the bacteria as they encounter growth limiting environmental conditions. Bacterial virulence genes may be transferred between bacteria by plasmids, a process called conjugation. Examples include antibiotic resistance genes, heavy metal resistance genes, genes that allow bacteria to metabolize uncommon substrates, bacteriocins (toxins made to kill neighboring bacteria lacking the plasmid), and virulence genes, such as heat labile and heat stable enterotoxins of Escherichia coli, exfoliative toxin of Staphylococcus aureus and edema factor, and lethal factor and protective antigen of Bacillus anthracis.
Table 222-2. Original and Revised Koch’s Postulates
Bacteriophage are bacterial viruses that parasitize their host bacteria, infect the bacteria and use various bacterial functions to make multiple copies of themselves, and lyse the bacteria in a process called lytic growth.10 However, some bacteriophages are also capable of an alternative cycle in which they shut down their lytic functions and either insert themselves into the host chromosome (eg, phage λ) or exist as low copy number plasmids (eg, phage P1). In these lysogenic (or prophage) states, the bacteriophage becomes a relatively stable part of the bacterial genome. Virulence genes may thus be transferred between bacterial hosts by bacteriophage, a process called transduction. In some cases, prophage may express genes that are beneficial to the host bacterium, including virulence genes such as diphtheria toxin genes of Clostridium diphtheriae, cholera toxin genes of Vibrio cholerae, and shigalike toxins of Escherichia coli.
Insertion sequences (IS elements), small regions of DNA (500 bp to ∼2,500 bp), insert themselves at many different sites in bacterial chromosomes, plasmids, or phage. The presence of IS elements in the bacterial genome affect bacterial virulence potential because of their role in homologous recombination, increasing the probability of the uptake of exogenous virulence genes by the bacteria.
Transposons (Tn) are larger elements that are created on the insertion of two IS elements near each other. The region between them, which may carry virulence genes among other things, can then be transposed—spread from bacterial cell to a neighboring bacterial cell or to another site on a single bacterial cell—by the joint action of the flanking elements. Many antibiotic resistance genes are carried on transposons. Another function of transposons in bacterial pathogenesis is their ability to disrupt existing genes when they are inserted into a new genomic region.
Pathogenicity islands (PAI) are large (often >30 kb), unstable blocks of chromosomal virulence genes that are capable of being transmitted from strain to strain among bacteria.11 They are identified by the difference in their G+C content compared to DNA of host bacteria, and are often flanked by direct repeats and located next to tRNA genes and/or insertion sequence (IS) elements. A single PAI often carries multiple virulence genes and has been shown to be present in pathogenic strains and absent or sporadically distributed in less pathogenic strains of a single species. Examples include PAIs found in urinary tract isolates of Escherichia coli compared to rectal isolates of E coli, an island found in Vibrio cholerae that contains the TCP pilus gene cluster and other virulence genes that is lacking in related Vibrio species, and the cag pathogenicity island of Helicobacter pylori associated with strains causing ulcers and stomach cancer but is missing in many less pathogenic strains.
Chromosomal genes that encode virulence genes are sometimes transferred between closely related bacterial strains by a process called horizontal gene transfer. Such transfer may occur via bacteriophage or via plasmids, although these are relatively low frequency events. Another method of transferring genes between bacterial species includes “natural transformation,” in which bacteria directly take up naked DNA from their environment, and if the DNA is similar enough to that of the recipient strain, recombine it into their chromosomes. Examples of important human pathogens that undergo natural transformation, and transformation of virulence genes, include Haemophilus influenzae, Helicobacter pylori, Neisseria gonorrhoeae, and Streptococcus pneumoniae.
MECHANISMS OF BACTERIAL PATHOGENESIS
Bacteria have evolved in parallel with humans and have developed numerous strategies to live in concert with their human hosts and, in some cases, to damage their human hosts, either for their own benefit or as an accident of their microbial lifestyle.
 ATTACHMENT
ATTACHMENT
For bacteria to remain intimately associated with human tissues, adhesive molecules (adhesins) on bacterial surfaces bind specific receptors on host cells.14 Receptor-mediated adherence plays two important roles in bacterial pathogenesis: (1) it allows the bacteria to resist the flushing and cleaning mechanisms that protect many epithelial surfaces, and (2) it determines the site of infection by facilitating specific surface-to-surface interactions between the bacteria and the host epithelium. Differential adherence to tissues is so critical to the different stages of bacterial interaction with the host that most bacteria have multiple adhesins with different functional capabilities.
Adhesins that are close to the surface of the bacteria have the potential of being hidden beneath large molecules such as lipopolysaccharides or bacterial capsules, making them unable to interact with the appropriate receptors on the host cells. In part to get around this problem, many adhesins are located at the end of long filamentous extracellular appendages composed of up to 10,000 polymerized protein subunits. These structures, called fimbriae or pili, not only extend well past bacterial capsules, but they also increase the effective diameter of the bacterial cell and increase the chance that the adhesin at the tip of the pilus will be able to interact with a host receptor. In addition to helping bacteria attach to host tissues, some pili help the bacteria expressing them to form biofilms.
 COLONIZATION
COLONIZATION
During both colonization and infections, bacteria are almost universally present in biofilms, a complex aggregation of organisms, DNA, bacterial products, and host cell debris enmeshed in an adhesive matrix. Life in a biofilm affords several advantages to bacteria, such as avoidance of some host defenses, avoidance of molecules toxic to bacteria (eg, some antibiotics), and avoidance of physiologic conditions in the host environment that may be hostile to the microbes.15
Biofilms are dynamic structures with a circulation system for distribution of nutrients and a specific sequence maturational events determined by bacterial signals. Biofilms spawn biofilm-free (planktonic) bacteria, resulting in dispersion of bacteria with variable pathogenic potential. Bacterial cells in different regions of a biofilm exhibit different patterns of gene expression and, thus, possess variable characteristics, such as antigenic features, nutritional requirements, growth parameters, and susceptibility to antibiotics. The role of biofilms in infections is under study, but clearly biofilms allow bacteria to persist in foreign material implanted into humans, such as bladder and vascular catheters, and certain infections, such as chronic bronchitis in patients with cystic fibrosis, are the result of bacteria in biofilms.
 BACTERIAL INVASION
BACTERIAL INVASION
Many bacteria exhibit characteristics that facilitate their spread within humans. Such spreading factors are generally bacterial enzymes that affect the physical properties of tissue matrices and intercellular spaces. For example, hyaluronidase produced by streptococci, staphylococci, and clostridia, which depolymerize the hyaluronic acid of human connective tissue; and streptokinase and staphylokinase produced by streptococci and staphylococci, respectively, which convert inactive plasminogen to plasmin, thus digesting fibrin and allowing rapid diffusion of the bacteria through infected tissues. In addition, bacteria have evolved mechanisms to survive inside phagocytic cells by interfering with the formation or function of the phagolysosome.
Examples include Listeria monocytogenes, Shigella flexneri, and Rickettsia, whose hemolysin lyses open the phagosome, releasing the bacteria into the host cytosol, where they are able to replicate. Each organism then causes asymmetric actin polymerization to form an “actin rocket” that shoots the bacteria into a neighboring cell, allowing the bacteria to spread cell to cell without encountering potential antibacterial factors outside host cells.16 Mannose-capped lipoarabinomannan (Man LAM) released from M. tuberculosis inside phagosomes inhibits phagosome-lyso-some fusion, allowing the bacteria to persist in macrophages.
 CELL AND TISSUE DAMAGE
CELL AND TISSUE DAMAGE
Bacterial toxins are bacterial substances (generally proteins) that produce a toxic effect on eukaryotic cells.18Exotoxins are specific molecules released from growing bacteria and have direct toxic effects on eukaryotic cells. Enterotoxins are exotoxins produced by bacteria in the intestinal tract that cause diarrhea or appear to overstimulate T cells. Endotoxins are sections of bacterial cell walls or membranes that, when present in large volumes, have a toxic effect on the host intestinal cells.
Many toxins act directly at the surface of the host cells, such as cytolysins, which are capable of lysing mammalian cells. Most toxins must enter host cells to carry out their effects and, thus, possess a “delivery” domain and an “action” domain. The range of activities of bacterial toxins is vast and includes cholera toxin of Vibrio cholerae, shiga toxin of Shigella dysenteriae and certain strains of Escherichia coli, and the neurotoxin of Clostridium botulinum. Some toxins act without actually entering cells, such as superantigens of Streptococcus pyogenes and Staphylococcus aureus, which activate T cells expressing particular Vβ chains in the T-cell receptor and bind to these chains with high affinity.19 At the same time, they bind to the major histocompatibility complex class II molecules (MHC-II) of antigen-presenting cells, resulting in T-cell proliferation independent of the normal binding specificity of the T-cell class. Host immunity may also, paradoxically, injure host cells, and the host inflammatory response to a bacterial infection may be responsible for the manifestations of the infectious disease through deposition of immune complexes, delayed-type hypersensitivity responses, or host inflammation caused through stimulation of inflammatory cytokines.
 EVASION OF HOST DEFENSES
EVASION OF HOST DEFENSES
Bacteria have developed a number of specific mechanisms to evade human host defenses and, thus, successfully maintain their interactions with humans. Such mechanisms include evasion of phagocytosis through the action of bacterial surface molecules such as capsules of pyogenic bacteria and lipopolysaccharides of gram-negative bacteria, as well as through molecular mimicry, in which host tolerates hostlike bacterial molecules; antigenic variation, in which the host fails to recognize altered bacterial antigens; and phase variation, in which certain bacterial factors are variably, and reversibly, expressed. For bacteria to survive extracellularly within the circulatory system of the human body, they must be resistant to the killing action of serum (as mediated by complement with or without antibody), to phagocytosis by professional phagocytes, and to cellular immune activities. To evade these host protective systems, many bacteria have polysaccharide material, called bacterial capsules, surrounding them. The capsule inhibits phagocytosis, probably due to the prevention of opsonization through resistance to the direct effects of complement, as well as through the repellant electrostatic forces associated with the highly negatively charged surface polysaccharide. Many bacteria are able to avoid human host defenses because of the presence of surface molecules that are antigenically similar to those present on human cells, in a process known as molecular mimicry. The human immune system is tolerant of these bacterial factors and, because they are recognized as “self,” no immune response is generated in their presence. Examples include the decoration of surface molecules of Streptococcus agalactiae, Neisseria meningitidis, and Haemophilus influenzae with sialic acid. Bacteria also escape antigen-specific host immunity by antigenic variation, such that there can be up to a 25% variation in genetic content coding for surface antigens, allowing bacteria of the same species to escape antigen-specific host immunity.20 Examples include the different capsular types of Streptococcus pneumoniae and Haemophilus influenzae, some of which demonstrate increased pathogenicity compared to others. Another mechanism of evading host defenses is known as phase variation. Because the presence of virulence factors may be beneficial to bacteria in some environments but detrimental in others, bacteria have devised reversible and inherited strategies for alternating expression with nonexpression of phenotypic traits, which is called phase variation.21 For example, the presence of pili on the bacterial surfaces may result in increased phagocytosis of the bacteria by host neutrophils, and yet, the presence of pili facilitates bacterial adherence to mucosal epithelial cells, fostering colonization. In Proteus mirabilis infections, only piliated bacteria adhere well to uroepithelial cells and readily produce ascending urinary tract infection in an animal model. But when the route of inoculation is via the bloodstream, the piliated bacteria are ingested by phagocytes, and only nonpiliated bacteria are able to produce hematogenous pyelonephritis. Thus, the ability to “phase vary” between states in which bacteria express certain surface molecules, or fail to do so, may be an important virulence trait.13
 ANTIBIOTIC RESISTANCE
ANTIBIOTIC RESISTANCE
Bacterial resistance to antibiotics can be viewed as a virulence factor because such activity promotes bacterial growth under certain host conditions, such as presence of antibiotics to which bacteria are resistance.
The prevalence of wide host range, conjugal plasmids that carry multiple drug resistance genes, many of which are also components of transposons, has greatly increased the spread of drug resistance among important pathogenic bacteria and, under selective antibiotic pressure, increased their pathogenicity.22
In addition, bacterial resistance to antiseptics and disinfectants (especially those now being marketed in “antibacterial” soaps and other household products) may demonstrate cross-resistance with antibiotics used for medical purposes. The most commonly used agent, triclosan, has been found to inhibit an enzyme involved in fatty acid synthesis. Triclosan-resistant Pseudomonas aeruginosa possess efflux pumps that simultaneously remove other antibiotics from the bacterium.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


