Asthma
Gurjit K. Khurana Hershey
Asthma is a chronic inflammatory disorder of the airways characterized by increased airways hyperresponsiveness and mucus production. Its symptoms of cough, wheeze, shortness of breath, and chest tightness are associated with variable airflow limitation that is at least partly reversible. Asthma is estimated by the World Health Organization to affect 150 million people worldwide,1 and its global pharmacotherapeutic costs exceed $5 billion per year. In children, where asthma remains the leading cause of emergency care and hospitalization, rates continue to rise. The National Asthma Education and Prevention Program recently issued its third Expert Panel Report outlining guidelines for the diagnosis and management of asthma. The importance of inflammation in the pathogenesis of asthma remains recognized and highlighted. The heterogeneity of asthma is also a key feature of the report. The Panel emphasizes the importance of individualizing treatment for patients because of the heterogeneous nature of the disease.
EPIDEMIOLOGY
Asthma is one of the leading chronic childhood diseases in the United States and a major cause of childhood disability.1 From 1980 to 1996, asthma prevalence among children 0 to 17 years of age more than doubled, from 3.6% in 1980 to 7.5% at the peak of the trend in 1995. Although the prevalence rate has leveled off since 1995, prevalence remains at high levels, and in 2005, 12.7% of children had been diagnosed with asthma at some point in their lifetime (9 million children), of whom 70% were reported to currently have asthma (6.5 million). Nearly two thirds of these children who currently have asthma reported at least 1 attack in the previous 12 months, highlighting the problem of poorly controlled asthma in the childhood age group. Despite increased overall health care utilization and that there are means to prevent attacks or exacerbations, the majority of children with asthma still suffer from attacks. Furthermore, the burden of avoidable emergency department visits and hospitalizations for asthma is high and has remained resistant to intervention efforts.
 RACIAL DISPARITIES
RACIAL DISPARITIES
Racial disparities in childhood asthma are extensive.2 Children of American Indian or Alaska Native descent have current asthma prevalence rates 25% higher, and black children 60% higher, than those in white children. African Americans are 4 times more likely to be hospitalized and 5 times more likely to die of asthma than non–African Americans. When race and ethnicity are considered, Puerto Rican children have the highest prevalence of all groups, 140% higher than non-Hispanic white children. In light of these differing prevalence rates, the lower rate for ambulatory care visits among black children compared with white children suggests that black children may be underutilizing ambulatory care. Rates in adverse outcomes such as emergency department visits, hospitalizations, and death are substantially higher for black children. The disparity in asthma mortality between black and white children has increased in recent years. The relative importance of urban residence, low socioeconomic status, and minority (particularly black and Hispanic) status as independent risk factors for increased asthma morbidity and mortality remains controversial.
 NATURAL HISTORY OF ASTHMA IN EARLY LIFE
NATURAL HISTORY OF ASTHMA IN EARLY LIFE
The Tucson cohort study,3 which followed children from birth or early childhood, described 2 asthmatic phenotypes in children: Transient wheezing is associated with symptoms in the first 3 to 5 years of life and with decreased lung function, maternal smoking during pregnancy, and exposure to other siblings or children at day care centers. Family history of asthma or allergic sensitization was not part of this phenotype. Episodic asthma symptoms were associated with apparent viral infections. Nonatopic wheezing independent of either sensitization or atopy but associated with wheezing and respiratory syncytial virus in the first years of life carried an increased likelihood of wheezing up to 13 years of age. Immunoglobulin E (IgE)-mediated wheezing is associated with evidence of allergic sensitization and portrays the classic asthma pheno-type. Early allergic sensitization is a significant risk factor for persistent asthma. Among school-age children, allergies/atopic sensitization starts to become an even more prominent cause of wheezing and displaces respiratory infections as a main trigger of attacks. Follow-up from the Tucson cohort at age 16 revealed that 60% of children with asthma in the prepubertal period continue to have intermittent wheezing after puberty. Asthma was found to remit in adolescence in 21% of cohort participants, but 11% had newly diagnosed asthma, so the global burden of the disease was largely unchanged. Allergic sensitization and obesity were associated with persistent asthma.
The important insights that have been gained in the natural history of asthma yield questions about the potential for early intervention and prevention or attenuation of childhood asthma by early identification of the high-risk population of children who have symptoms before 3 years of age and will develop persistent asthma. It is important to distinguish this group from the majority of children who wheeze before 3 years of age and do not experience any more symptoms after 6 years of age. Recently, the asthma predictive index was developed4 and subsequently validated2 to predict which children among those who had asthmalike symptoms early in life would go on to have persistent asthma. The asthma predictive index identifies the following risk factors for developing persistent asthma among children younger than 3 years of age who had 4 or more episodes of wheezing during the previous year: either one of the following major criteria: parental history of asthma, a physician diagnosis of atopic dermatitis, or evidence of sensitization to aeroallergens; or two of the following minor criteria: evidence of sensitization to foods, 4% or higher peripheral blood eosinophilia, or wheezing apart from colds. Ninety-five percent of wheezy young children with a negative index never developed asthma between their 6th and 13th years. Using this index to identify the young children at highest risk for persistent asthma, Guilbert and colleagues examined whether inhaled corticosteroids could modify the subsequent development of asthma in pre-school children at high risk for asthma.2 However, no significant differences were seen between the treatment and placebo groups in the proportion of episode-free days, the number of exacerbations, or lung function after corticosteroids were discontinued. Thus, in preschool children at high risk for asthma, 2 years of inhaled-corticosteroid therapy did not change the development of asthma symptoms or lung function during a third, treatment-free year. Thus, the natural history course of asthma was not altered by anti-inflammatory treatment with inhaled corticosteroids under the conditions examined in this study. The concept of prevention is very important, and the age, duration, and nature of the intervention obviously may affect the findings.
ENVIRONMENTAL RISK FACTORS
Evidence of the impact of the environment on asthma incidence and morbidity—especially allergens and irritants such as cigarette smoke and outdoor pollutants—has been mounting. The hygiene hypothesis was proposed in 1986 in an attempt to provide a framework to understand the epidemiological observations in the late 19th and early 20th centuries that allergic disorders were increasing in prevalence and were more prevalent in westernized than in developing countries. It proposed that reduced exposure to infections in early childhood, due to increased use of antibiotics, decreased rural exposures, diminishing family size, improved living standards, and improved personal hygiene, resulted in increased risk of developing allergic disease.5 The underlying mechanism for the hygiene hypothesis has focused traditionally on a skewing of the Th1/Th2 balance toward Th2 responses. Th1 and Th2 cells are functional subsets of CD4+ T cells defined phenotypically by the production of polarized sets of cytokines: Th1 cells produce interleukin (IL)-2, interferon-γ, and tumor necrosis factor-β, which are important in macrophage activation, phagocytic responses, and the development of cell-mediated immunity. Th2 cells produce IL-4, IL-5, IL-10, and IL-13 and are important in the inhibition of macrophage activation and the development of IgE responses and eosinophilia. The immunologic milieu during T-cell priming is important in driving CD4+ T-cell polarization. IL-12 is indispensable for the development of most Th1 responses, and IL-4 has a similar role for Th2 responses. A reduction in developed regions of environmental factors and microbial exposures that promote Th1 responses leads to skewing of the immune response toward a Th2 immunologic milieu that favors the development of Th2-mediated allergic disorders. However, this hypothesis has now evolved to incorporate the worldwide epidemiologic trends witnessing the simultaneous increase in the prevalence of both Th1- and Th2-mediated disorders. In order to accommodate these observations, the hygiene hypothesis has evolved along with novel insights into the development of innate immunity. It is now proposed that early-life microbial and environmental exposures modify the development of the host immune system and affect future adaptive immune responses by invoking counterregulatory mechanisms. Alterations in these critical early life exposures has resulted in biologically significant changes in these counterregulatory mechanisms, and this has translated to the observed trends in prevalence rates for allergic disorders, including asthma. There are many recognized environmental exposures that impact the development of asthma, and undoubtedly, there are many more that are not yet recognized.
 ALLERGENS
ALLERGENS
The association of asthma and allergy has been long recognized, first in cross-sectional studies and more recently in prospective studies. IgE-mediated hypersensitivity to environmental allergens is present in the majority of children and young adults with asthma, and exposure to allergens appears to be involved in the initial development of asthma as well as in the exacerbation of existing asthma. Sensitization and exposure to house dust mites and Alternaria mold are important factors in the development of asthma in children. Data from the Childhood Asthma Management Program (CAMP) revealed that house dust mite and cockroach exposure are strong risk factors for sensitization. Thus, allergen exposure is linked to sensitization, which is a risk factor for asthma. However, the role of allergens in the development of asthma is complex and is yet to be fully defined. Recent observations from longitudinal birth cohort studies have revealed that dog exposure in early life may actually protect against the development of asthma. Thus, environmental influences may have different effects on disease during specific windows of opportunity or times when the child is most vulnerable. There is a strong association between asthma, allergic rhinitis, and atopic dermatitis in childhood, and the sequence of these events has been termed the atopic march, where atopic dermatitis is the earliest manifestation, followed by allergic rhinitis and then the onset of asthma. Due to the high prevalence of allergy in children with asthma, allergy testing is recommended for patients who have persistent asthma. Based on data on children in the United States, it is estimated that at least 70% of all patients who have asthma have persistent asthma.
 ENVIRONMENTAL TOBACCO SMOKE (ETS)
ENVIRONMENTAL TOBACCO SMOKE (ETS)
Despite an overall decrease in tobacco use in the United States over the last decade, the prevalence of cigarette smoking remains high in urban populations. Fifty-nine percent of urban asthmatic children enrolled in the National Cooperative Inner-City Asthma Study and 48% of urban asthmatic children enrolled in the Inner-City Asthma Study live in a house with at least 1 cigarette smoker. In the National Cooperative Inner-City Asthma Study, a household member was smoking during 10% of the home visits, and 48% of urine samples collected from asthmatic children had cotinine/creatine ratios that were consistent with significant tobacco smoke exposure in the last 24 hours. Among children who have asthma, exposure to environmental tobacco smoke is associated with increased symptoms, decreased lung function, and greater use of health services.
 AIR POLLUTION
AIR POLLUTION
Epidemiologic and laboratory studies have provided evidence that inhalation of respirable particulate matter adversely affects lung function in patients with asthma. Diesel exhaust particles are respirable with over 90% in the fine or ultrafine size range. They are composed of elemental carbon cores with large surface areas capable of binding organic polycyclic aromatic hydrocarbons, transition metals, and airborne allergens, all of which have the potential to induce reactive oxygen species and inflammation. Diesel exhaust particles can interact directly with allergens and have been shown to augment allergen-induced responses.
 RESPIRATORY INFECTIONS
RESPIRATORY INFECTIONS
A number of respiratory viruses in infancy have been associated with the subsequent development of asthma. Prospective longitudinal studies of children admitted to hospital with documented respiratory syncytial virus have observed that approximately 40% of these infants will continue to wheeze or have asthma in later childhood. Symptomatic rhinovirus infections in early life also are emerging as risk factors for recurrent wheezing. As discussed previously, the majority of children who wheeze with viral infections do not go on to develop asthma; further understanding of the viral mechanisms that contribute to persistent recurrent wheezing is needed.
COMORBID CONDITIONS
 ALLERGIC RHINITIS AND SINUSITIS
ALLERGIC RHINITIS AND SINUSITIS
The upper and lower airways exist as a continuum and show similar histopathologic changes when inflamed, including epithelial damage, thickening of the basement membrane, and a predominantly eosinophilic cellular infiltrate. Epidemiologic studies support a strong association between allergic rhinitis and asthma. Segmental bronchial allergen challenge causes inflammatory changes in both nasal and bronchial mucosa. Epidemiologic studies confirm that sensitization among genetically susceptible populations to allergens, including house dust mite, pet dander, Alternaria mold, and cockroach, confers risk for childhood asthma.6 Anti-inflammatory treatment aimed at the upper airway results in decreased markers of lower airway inflammation.7 Furthermore, treatment of allergic rhinitis with antihistamines and intranasal steroids have been reported to decrease emergency department visits for asthma.3 Similar to rhinitis, sinusitis can contribute to asthma symptoms.
 ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS
ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS
Allergic bronchopulmonary aspergillosis (ABPA) should be suspected in patients who have asthma and have the presence or a history of pulmonary infiltrates. The criteria for the diagnosis of ABPA complicating asthma include (1) positive immediate skin test to Aspergillus, (2) total serum IgE greater than 417 IU (1,000 ng/mL), (3) elevated Aspergillus-specific serum IgE and/or IgG, and (4) central bronchiectasis.8 Additional supporting findings for a diagnosis of ABPA include a sputum culture positive for Aspergillus, serum-precipitating antibodies to Aspergillus, and an arthus late-phase response after intradermal injection of Aspergillus. The standard treatment for ABPA is oral steroids. Serum total IgE levels and follow-up chest radiographs are used to monitor response to therapy.8 Early, aggressive therapy may prevent progression to advanced-stage disease. Azole antifungal agents have also been tried as adjunctive treatment in patients who are stable and who have ABPA. Itraconazole administered orally for 16 weeks reduced sputum eosinophilia, serum IgE and IgG levels, and the number of exacerbations requiring oral corticosteroids.
 GASTROESOPHAGEAL REFLUX DISEASE (GERD)
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
Symptoms of GERD are common in both children and adults who have asthma. According to the National Guidelines Expert Panel Report 3, medical management of GERD should be instituted for patients who have asthma (especially nocturnal symptoms) and complain of frequent heartburn or pyrosis.6 In patients who have poorly controlled GERD, treatment with a proton pump inhibitor has been reported to reduce nocturnal symptoms, reduce asthma exacerbations, and improve quality of life related to asthma.
 OBESITY
OBESITY
The parallel rise in the prevalence of asthma and obesity suggests that they are related. Obesity has been associated with asthma persistence and severity in both children and adults.9 Compared with nonasthmatics, body mass index in asthmatics was 44% to 48% higher in 3 cross-sectional US health surveys. Further support for an association between asthma and obesity is provided by prospective studies, which show that risk for asthma is increased with increasing body mass index. A recent meta-analysis confirmed that obesity is a strong risk factor for incident asthma.10 Notably, as obese asthmatics lose weight, their asthma symptoms and lung function improve.
 ASPIRIN SENSITIVITY
ASPIRIN SENSITIVITY
The classic aspirin triad (also known as the Samter triad) of asthma, aspirin intolerance, and nasal polyposis most commonly develops in adulthood; however, up to 5% of children with asthma may have aspirin-induced symptoms. Avoidance of aspirin and nonsteroidal anti-inflammatory drugs should be considered in children with severe, persistent asthma or nasal polyps. Studies have shown relative overproduction of cysteinyl leukotrienes linked to an imbalance between proinflamma-tory and anti-inflammatory mediators derived from arachidonic acid.
PATHOPHYSIOLOGY
According to the Expert Panel Report 3, asthma is defined as
a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role: in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells. In susceptible individuals, this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli. Reversibility of airflow limitation may be incomplete in some patients with asthma.
Airway inflammation in asthma is found in patients with mild, moderate, and severe disease. The pathologic features of the asthmatic airways include denudation of the airway epithelium, mucus overproduction, goblet cell hyperplasia, basement membrane thickening with variable subepithelial fibrosis, bronchial smooth muscle hyperplasia, and cellular infiltration with eosinophils, lymphocytes, and neutrophils (especially in acute or fatal disease; Fig. 512-1). Airway narrowing and subsequent airflow limitation leads to clinical symptoms in acute exacerbations of asthma whereby bronchoconstriction occurs quickly to narrow the airways in response to exposure to a variety of triggers, including allergens, irritants, and viral infection. As the disease becomes more persistent and inflammation plays a bigger role, other factors further limit airflow. These include edema, inflammation, mucus overproduction, and airway smooth muscle hypertrophy and hyperplasia. In some persons who have asthma, airflow limitation may be only partially reversible due to permanent changes in the airway known as airway remodeling.
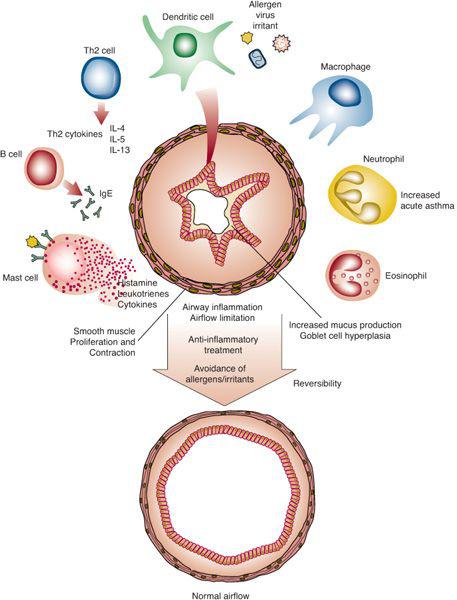
Inflammation has a central and consistent role in the pathophysiology of asthma regardless of the severity or subtype of asthma. It is due to many mediators and processes, including cytokines, chemokines, leukotrienes, oxidative stress, and neuropeptides. The airway inflammation involves an interaction of many cell types, including lymphocytes (specifically Th2 cells), mast cells, eosinophils, macrophages, dendritic cells, and neutrophils, and leads to airflow limitation that is reversible (Fig. 512-2).
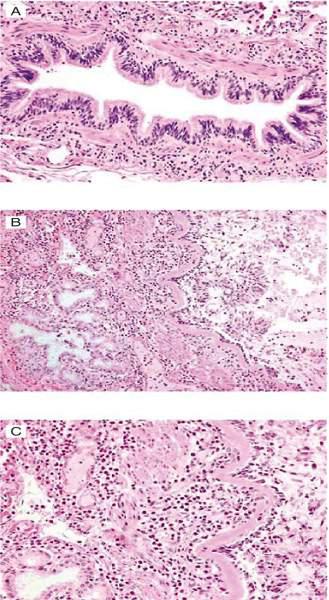
FIGURE 512-1. Pathology of an airway from a normal patient (A) compared with that of a patient who died of fatal asthma (B: 10× magnification; C: 20× magnification). The features include denudation of the airway epithelium, mucus overproduction, goblet cell hyperplasia, basement membrane thickening, bronchial smooth muscle hyperplasia, and cellular infiltration.
GENETICS
Although environmental influences are important in the development of asthma, there is a strong genetic predisposition.  A recent review11 of nearly 500 papers on asthma genetic studies identified 10 genes (IL4, IL13, CD14, ADRB2, HLA-DRB1, HLA-DQB1, TNF, FCER1B, IL4RA, ADAM33) that have been associated with an asthma or atopy pheno-type in more than ten populations.
A recent review11 of nearly 500 papers on asthma genetic studies identified 10 genes (IL4, IL13, CD14, ADRB2, HLA-DRB1, HLA-DQB1, TNF, FCER1B, IL4RA, ADAM33) that have been associated with an asthma or atopy pheno-type in more than ten populations. 
DIAGNOSIS
According to the National Expert Panel Report 3,6 a diagnosis of asthma should be considered if any of the following clinical indicators are present: wheezing (high-pitched whistling sounds, especially in children), but asthma can occur in the absence of wheezing; recurrent cough; recurrent chest tightness or difficulty breathing; worsening symptoms with exercise or at night; or worsening symptoms during viral infection, exposure to furry pets, changes in weather, exposure to pollen, or environmental tobacco smoke (all known triggers for asthma). Improvement of symptoms after treatment with a bronchodilator is suggestive of asthma, but a lack of improvement does not rule out asthma. Pulmonary function testing is recommended if any of the indicators is present.
Symptom history varies with age. An infant or young child often has a history of recurrent wheeze or persistent cough with colds, while older children often complain of chest tightness or persistent cough/wheeze. Triggers for childhood asthma often include viral infections (especially respiratory syncytial virus and rhinovirus), allergen exposure, irritants (environmental tobacco smoke, pollution), weather changes, stress or emotional factors, gastroesophageal reflux, aspirin sensitivity, hormonal factors such as menses, and exercise.
The upper respiratory tract, chest, and skin are the focus of the physical examination for childhood asthma. Physical findings that increase the probability of asthma include hyperexpansion of the thorax, use of accessory muscles of breathing, wheezing during normal breathing or elicited by forced exhalation (typical of airflow obstruction), rhinitis, swollen pale nasal turbinates and/or nasal polyps, and the presence of atopic dermatitis/eczema. The absence of these findings does not rule out asthma, because the disease is by definition variable, and signs of airflow obstruction are often absent between attacks.
 PULMONARY FUNCTION TESTS
PULMONARY FUNCTION TESTS
Pulmonary function tests are objective and noninvasive. A pulmonary function test should be attempted in children 5 years old or older with symptoms suggestive of asthma. Objective assessments of pulmonary function are recommended for the diagnosis of asthma because medical history and physical examination are not reliable means of excluding other diagnoses or of characterizing the status of lung impairment. These measurements help to determine whether there is airflow obstruction, its severity, and whether it is reversible over the short term. Demonstration of reversibility of airflow obstruction following inhalation of a bronchodilator is central to the definition of asthma. Examination of the volume time curve and the shape of the flow-volume loop provides an estimate of the adequacy of the patient effort in performing the test. Airflow obstruction is indicated by a reduction in the values for both the forced expiratory volume in 1 second, FEV1, and the FEV1 relative to FVC, forced vital capacity, or FEV1/FVC when compared to reference or predicted values. Predicted values for FEV1/FVC are based on National Health and Nutrition Examination Survey (NHANES) data, National Center for Health Statistics, Centers for Disease Control and Prevention (CDC). Significant reversibility is indicated by American Thoracic Society standards as an increase in FEV1 of at least 12% from the baseline measure after inhalation of a short-acting bronchodilator (eg, albuterol, 2–4 puffs of 90 mcg/puff). If obstruction is detected on the baseline pulmonary function test, a bronchodilator (albuterol) should be administered and the test repeated in 20 minutes. An improvement of 12% or greater in the FEV1 is consistent with a diagnosis of asthma; however, neither this finding nor any other single test or measure is adequate to diagnose asthma. In addition to the pulmonary function test results, the patient’s history and symptoms along with the exclusion of other possible diagnoses are needed to establish a diagnosis of asthma. 
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


