Asthma is the commonest chronic illness of childhood, occurring in up to 15% of children. The symptoms of cough, wheeze and dyspnoea are due to narrowing of the bronchi and bronchioles, mucosal inflammation and thick mucus. In a susceptible individual this process is initiated by environmental factors such as dust mite allergens, air pollution, cigarette smoke, cold air, viral infections, stress and exercise.
Presentation
Children with asthma usually present in infancy or early childhood. The diagnosis is clinical, based on recurrent cough or wheeze that responds to bronchodilator treatment. A history of atopy (eczema or hay fever) or a family history of asthma supports the diagnosis. In infancy it is often unclear whether recurrent wheeze is the first manifestation of asthma or merely airway obstruction due to viral respiratory tract infections. As the airways are narrow, mucosal oedema contributes more to obstruction than bronchoconstriction, and there may be poor response to bronchodilators.
In older children recurrent episodes of wheeze and cough, especially if triggered by exercise, viral infections or allergens, suggest a diagnosis of asthma. A good response to bronchodilators, either in symptom reduction or improvement in peak expiratory flow rate (PEFR), confirms the diagnosis. In asthma the chest radiograph may show hyperinflation (due to air trapping) and areas of collapse (due to mucous plugging). Skin prick testing is not usually helpful. Blood can be sent for specific IgE to common inhaled allergens and may identify allergens to be avoided.
Management of Chronic Asthma
The goal of good asthma management is to relieve the symptoms and allow normal activity, school attendance and growth. A stepwise approach is used—increasing the amount of treatment until control is obtained, then stepping back to the minimum required to maintain good control.
Inhaler Devices
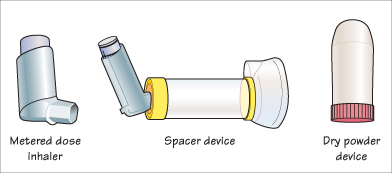
Treatment is effective only if the drug is delivered in sufficient quantity to the small airways of the lungs. This is best achieved using an aerosolized drug delivery system, via a metered dose inhaler (MDI). A high degree of coordination is required to activate the MDI during inhalation, and this method is really only suitable for teenagers.
For children under 5 years, the MDI can be used in conjunction with a spacer device (e.g. Aerochamber). In infants these should be fitted with a mask to place over the child’s mouth and nose.
Medical Management of Asthma in Children*
| <5 years | 5–12 years |
| Step 1. Mild intermittent asthma | |
| Inhaled short-acting β2 agonist prn | Inhaled short-acting β2 agonist prn |
| Step 2. Regular preventive therapy | |
| Add inhaled steroids | Add inhaled steroids |
| Step 3. Add-on therapy (<6 months proceed to step 4) | |
| Add leukotriene receptor antagonist | 1. Add inhaled long-acting β2 agonist (LABA) |
| 2. Consider leukotriene receptor antagonist or oral theophylline | |
| Step 4. Persistent poor control | |
| Refer to respiratory paediatrician | Increase dose of inhaled steroids |
| Step 5. Persistent poor control | |
| Not used | Add oral low-dose daily steroids |
| Refer to respiratory paediatrician | |
In children aged 5–12 the choice of device includes MDI spacer or Dry Powder Inhaler, depending on preference for convenience and effectiveness. Nebulisers can be used for delivering high doses quickly, although there is evidence that MDIs via a spacer are as effective. Nebulizers can be used in infants and for emergency treatment of acute exacerbations although there is evidence that MDIs via a spacer are as effective.
Treatment of Severe Exacerbation
Acute exacerbations should be treated promptly at home by using more reliever medication. If symptoms continue or worsen then aggressive treatment with high flow oxygen, regular β2-agonists or ipratropium bromide via a nebulizer or spacer device (e.g. 10 puffs) and systemic corticosteroids is indicated. All children should have oxygen saturations measured and be admitted for close observation. If the oxygen saturation in air is <92% following treatment then the child should be admitted to hospital. In life-threatening asthma an infusion of steroids, salbutamol or aminophylline is used.
KEY POINTS
- Asthma is the commonest chronic childhood illness, occurring in 10–15% of all children.
- Bronchoconstriction, viscid mucous and mucosal oedema cause airway narrowing with wheeze, cough and dyspnoea.
- Treatment is increased and decreased step by step to gain symptom control and maintain a normal lifestyle.
- It is crucial to use an inhaler device suitable for the child’s age.



