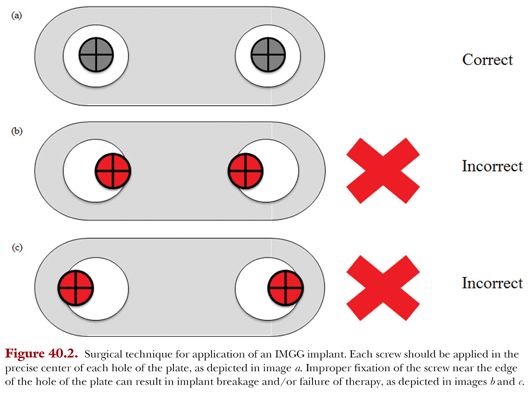
A bone age determination, made by analyzing the patient’s hand radiograph, should be made in order to identify whether or not the patient has reached skeletal maturity.12 This determination can now be made efficiently with the use of a shorthand method developed by researchers at the Hospital for Special Surgery that uses a single written criterion for each age rather than a single radiograph and multiple criteria (Fig. 40.1).13 For more detailed information on growth assessment in pediatric patients, see Chapter 38.
For patients with genu valgum who still have immature growth plates, IMGG is the preferred temporary corrective strategy because it permits subsequent growth upon implant removal. This technique is effective for patients who have at least 6 to 12 more months of growth remaining.4
HOW MUCH CORRECTION TO EXPECT PER MONTH
When deciding to initiate IMGG therapy, it is important to consider the implant’s rate of correction in order to avoid over- or undercorrection and appropriately monitor the patient’s treatment trajectory. Ballal et al.12 recently examined the rate at which the 8-plate corrected a cohort of 25 skeletally immature patients with either pathologic genu valgus or genu varus. The authors reported a mean correction rate of 0.7 degrees per month in the distal femur, 0.5 degrees per month in the tibia, and 1.2 degrees per month if the femur and tibia were treated simultaneously. They also found that children younger than the age of 10 years corrected at a faster rate, on average, than the children older than the age of 10 years (1.4 degrees per month vs. 0.6 degrees). Additionally, Boero et al.14 reported a mean correction rate of 0.93 degrees per month in the distal femurs of 58 patients treated with the 8-plate for either pathologic genu valgus or varus.
In a cohort of 25 patients with 47 valgus deformities treated with a tension band plate on the distal femoral physis, Guzman et al.15 reported a mean correction rate of the anatomic lateral distal femoral angle (aLDFA) of 0.96 degrees every 3 months, or 3.8 degrees per year. Consistent with the age-stratified results by Ballal et al.,12 Guzman et al.15 found that girls younger than 11 years of age and boys younger than 13 years of age corrected at a faster rate than older children (4.5 degrees per year vs. 3.4 degrees). Table 40.2 summarizes the most recent reported rates of correction in patients treated with IMGG for lower limb angular deformities.

As a temporary measure, IMGG inherently requires routine serial follow-ups to prevent overcorrection of the deformity and ensure that hardware removal occurs at the appropriate time. It is critical for the treating physician to educate the patient regarding the significance of follow-ups to monitor the treated knee, as overcorrection may demand compensatory IMGG in the contralateral side should the patient fail to follow up. Saran and Rathjen16 recommend a follow-up approximately every 4 months. Additionally, Blount and Clarke3 recommend not leaving the epiphyseal staples on the growth plate for more than 2 years in a growing child.
The surgical technique for fixation of different tension band plates typically follows the same general protocol and thus will be generalized for most commonly used implants. Before tension band plates can be applied, preoperative planning and radiologic analysis must occur to ensure appropriate application of the hardware. Standing anteroposterior (AP) and lateral radiographs that include the hip and the ankles should be analyzed to locate the patient’s center of rotation of angulation (CORA), which will indicate the precise site and magnitude of the deformity to be corrected. Blunt dissection will reveal the periosteal surface, which should be carefully exposed to prevent injury to this layer. Periosteal stripping should be avoided, as it may lead to growth arrest or asymmetrical growth.
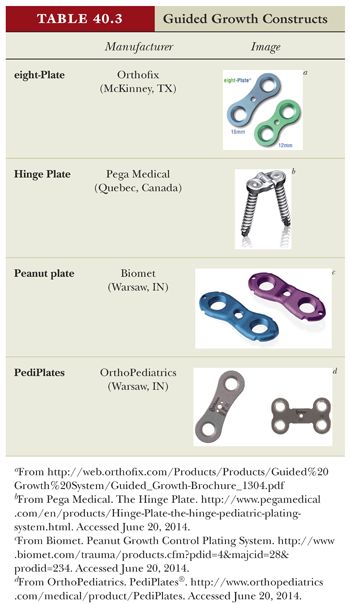
The following technical steps have been adapted from the technique manual published by Pega Medical for fixation of the Hinge Plate. Although this surgical protocol is relatively standard, innovation in tension band plates has resulted in a variety of plate designs, with more technical details specific to each plate type. A list of these guided growth constructs can be found in Table 40.3.
Under fluoroscopic imaging, a K-wire is introduced near the patient’s growth plate to ensure proper implant alignment over the physis. If a template is being used, the template is centered over the physis on the lateral surface of the bone using the K-wire as a guide. If a template is not being used, then the tension band plate will be directly applied over the K-wire. Next, a second K-wire is introduced through one of the two main screw holes of the template (or tension band plate) at an angle away from the growth plate with the aid of a wire guide. After verification of the K-wire’s position under fluoroscopy, a screw hole is drilled into the bone using a cannulated drill bit that matches the predetermined screw length. If a template is being used, then the template is removed at this point and the tension band plate is directed over the guiding K-wire to ensure proper placement. The guiding K-wire is removed, and a cannulated screw is introduced into the bone surface so that it is perfectly center within the plate’s first hole. Once the first screw is applied, proceed with the same method for drilling and screwing the second screw. It is important for the plate to be flush against the bone surface to prevent periosteal damage.
If performing a medial distal femur epiphysiodesis, it is critical to minimize damage to the medial patellofemoral ligament (MPFL), which inserts just distal to the femoral growth plate on the surface of the medial epicondyle.17 A recent experiment found that partial or complete transection of the MPFL occurred in 6 of 8 cadaveric knees after temporary mechanical hemiepiphysiodesis using a plate and two screws.18 Therefore, we recommend placing the plate in the posterior one-third of the femur and avoiding transection of the MPFL when applying a growth modulating implant to this area. Current literature has illuminated cases of postoperative pain and decreased range of motion following temporary mechanical hemiepiphysiodesis,8 and damage to the MPFL may be a significant contributing factor to these outcomes.
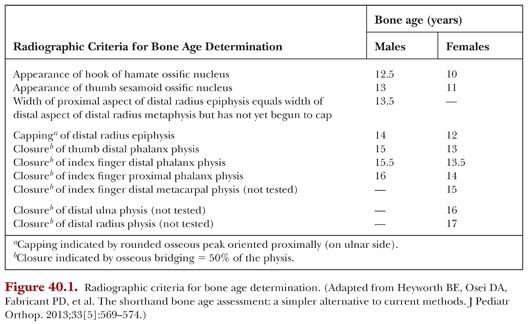
It is also critical to ensure that each of the screws is screwed directly into the center of the plate’s two holes. Incorrect placement of the screws near the edge of the plate’s holes can result in faulty plate fixation and ultimately implant failure. Figure 40.2 illustrates proper and improper screw position within the plate.