Chapter 26
Anesthesia for Cesarean Delivery
Lawrence C. Tsen MD
Chapter Outline
History
Cesarean delivery is defined as the birth of an infant through incisions in the abdomen (laparotomy) and uterus (hysterotomy). Although the technique is commonly associated with the birth of the Roman Emperor Julius Caesar, medical historians question this possibility, given his birth in an era in which such operations were invariably fatal (100 BC) and the acknowledged presence of Caesar’s mother in his later life.1 Although the term cesarean section is commonly used, the Latin words caedere and sectio both imply “to cut,” and modern linguists argue that use of both words is redundant. Consequently, cesarean delivery is the preferred term.
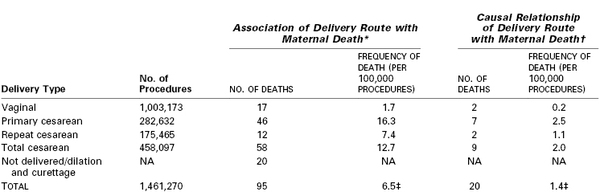
Morbidity and mortality, most often associated with hemorrhage and infection, limited the use of cesarean delivery until the 20th century, when advances in aseptic, surgical, and anesthetic techniques improved the safety for both mother and baby. Today, cesarean delivery is the most common major surgical procedure performed in the United States, accounting for more than 30% of all births and 1 million procedures each year.2 Globally, the incidence of cesarean delivery has progressively increased; however, the rate varies dramatically by country, ranging from 0.4% to 45.9% (Figure 26-1).3 Maternal, obstetric, fetal, medicolegal, and social factors are largely responsible for this variability, resulting in significant differences in cesarean delivery rates even among individual obstetricians and institutions (Box 26-1).4
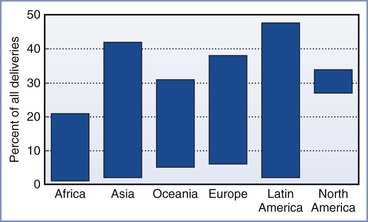
FIGURE 26-1 The range of cesarean delivery rates by world region as collected in surveys or vital registration system reports. (Data modified from Gibbons L, Belizan JM, Lauer JA, et al. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol 2012; 206:331.e1-19.)
Indications
The common indications for cesarean delivery include dystocia, malpresentation, nonreassuring fetal status, and previous cesarean delivery (Box 26-2). An elective cesarean delivery can be performed for obstetric or medical indications or at the request of a pregnant patient, and it is typically planned and performed prior to the onset of labor.5 A cesarean delivery performed during labor for a planned vaginal delivery can also occur for a wide range of maternal and fetal indications but may need to be conducted in an urgent or emergent manner. A prior cesarean delivery does not necessitate cesarean delivery in a subsequent pregnancy. A trial of labor after cesarean (TOLAC), which if successful is called a vaginal birth after cesarean (VBAC), is an alternative option; the use of TOLAC, once growing in popularity, has declined in recent years for a variety of reasons (Figure 26-2) (see Chapter 19).
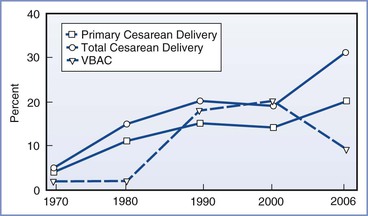
FIGURE 26-2 Rates of primary cesarean delivery, total cesarean delivery, and vaginal birth after cesarean delivery (VBAC) in the United States, 1970 to 2006. (Data for 1970-1988 from the National Hospital Discharge Survey; data for 1989-2006 from the National Vital Statistics System, Centers for Disease Control and Prevention. Available at http://www.cdc.gov.)
Operative Technique
The technical aspects of performing a cesarean delivery are comparable worldwide, with minor variations. A midline vertical abdominal incision allows rapid access and greater surgical exposure; however, the horizontal suprapubic (Pfannenstiel) incision offers better cosmesis and wound strength. Similarly, a low transverse uterine incision, in comparison with a vertical incision, allows for a lower incidence of uterine dehiscence or rupture in subsequent pregnancies, as well as a reduction in the risks of infection, blood loss, and bowel and omental adhesions. Vertical uterine incisions are most often used in the following situations: (1) when the lower uterine segment is underdeveloped (before 34 weeks’ gestation), (2) in delivery of a preterm infant in a woman who has not labored, and (3) in selected patients with multiple gestation and/or malpresentation. In some cases, a vertical uterine incision is performed high on the anterior uterine wall (i.e., classic incision), especially in the patient with a low-lying anterior placenta previa or when a cesarean hysterectomy is planned.
Uterine exteriorization following delivery facilitates visualization and repair of the uterine incision, particularly when the incision has been extended laterally. Although the effect of exteriorization on blood loss and febrile morbidity remains controversial,6 higher rates of intraoperative nausea, emesis, and venous air embolism as well as postoperative pain have been observed.7,8
Morbidity and Mortality
Complications of cesarean delivery include hemorrhage, infection, thromboembolism, ureteral and bladder injury, abdominal pain, uterine rupture in subsequent pregnancies, and death (Box 26-3).9 Nonelective cesarean delivery is associated with a greater risk for maternal morbidity than elective cesarean delivery; a 2008 study of all deliveries in Finland indicated that the rates of severe maternal morbidity were 5.2, 12.1, and 27.2 per 1000 vaginal, elective cesarean, and nonelective cesarean deliveries, respectively.10
Maternal mortality has decreased during the past 75 years (see Chapter 40). Since 1937, when the maternal mortality rate for nulliparous women undergoing cesarean delivery in the United States was 6%, the risk for death associated with the procedure has decreased by a factor of nearly 1000 owing to the availability of blood transfusions, antibiotics, safer anesthetic techniques, and critical care units.11 Maternal morbidity and mortality vary widely from country to country. In most developed nations, the rate of maternal death associated with all cesarean deliveries remains higher than that associated with vaginal deliveries.3,12 The risk for maternal death for a planned, elective primary cesarean delivery may not differ from that associated with a planned vaginal delivery, but performance of cesarean delivery places the mother at higher risk for morbidity (and perhaps mortality) in subsequent pregnancies and cesarean deliveries.13
Clark et al.12 identified the causes of maternal death in a retrospective study of 1.5 million deliveries that occurred between 2000 and 2006 within a health care network composed of primary, secondary, and tertiary care hospitals in 20 states (Table 26-1). Only 15% of maternal deaths were related to preexisting medical conditions; most deaths occurred in women classified as being at low risk at the beginning of pregnancy. The investigators concluded that 17 deaths (18%) could have been prevented by provision of more appropriate medical care. (Causality was determined by evaluating whether the maternal death could have been avoided with the use of an alternative route of delivery, with the assumption that all other details remained the same prior to delivery.) The preventable deaths were associated with postpartum hemorrhage (8), preeclampsia (5), medication error (3), and infection (1). Cesarean delivery was determined to be directly responsible for maternal death in four cases, including hemorrhage from surgical vascular injury in three cases and sepsis from surgical injury to the bowel in the fourth. Deaths associated with, but not directly caused by, cesarean delivery were associated with perimortem procedures or caused by thromboembolic phenomena; of the nine patients who died of thromboembolic phenomena, none had received peripartum mechanical or pharmacologic thromboprophylaxis. The investigators concluded that cesarean delivery per se was only rarely the causative factor in maternal death; in the majority of cases, death was related to the indication for the cesarean delivery rather than the operative procedure. Nonetheless, these investigators also concluded that the risk for death caused by cesarean delivery is approximately 10 times higher than that for vaginal birth and likely could be reduced with the implementation of universal perioperative thromboprophylaxis (see later discussion).
Neonatal morbidity, in particular respiratory system morbidity (thus potentially resulting in the anesthesia provider’s involvement in neonatal resuscitation), is greater with elective cesarean delivery than with vaginal delivery.14 Patterns and rates of neonatal mortality are similar to those of maternal mortality; the higher neonatal mortality rates observed after cesarean delivery most likely reflect the conditions that prompt nonelective cesarean delivery.15
Prevention of Cesarean Delivery
Neuraxial labor analgesia was earlier thought to increase the cesarean delivery rate compared with nonmedicated labor or other analgesic techniques; however, randomized controlled trials and sentinel event studies indicate that neuraxial analgesia is not associated with a higher cesarean delivery rate than systemic opioid analgesia (see Chapter 23).16,17 Moreover, the combined spinal-epidural (CSE) technique for labor analgesia, despite its association with fetal bradycardia, does not result in an increase in the total cesarean delivery rate.18,19 Some cesarean deliveries may be avoided through the provision of (1) adequate labor analgesia, including analgesia for trial of labor after cesarean delivery and instrumental vaginal delivery; (2) analgesia for external cephalic version (see Chapter 35); and (3) intrauterine resuscitation, including pharmacologic uterine relaxation in cases of uterine tachysystole.
Maternal Labor Analgesia
The National Institutes of Health consensus statement on cesarean delivery on maternal request emphatically concluded that “maternal request for cesarean delivery should not be motivated by unavailability of effective [labor] pain management.”5 It is of concern that a survey of 1300 hospitals indicated that as recently as 2001, 6% to 12% of hospitals in the United States did not provide any form of labor analgesia.20 Although the availability of labor analgesia, especially in the form of neuraxial techniques, has increased during the past three decades,20 there are still institutions, predominantly smaller ones, where cesarean deliveries are likely performed because of nonexistent or inadequate labor analgesia.
Adequate maternal analgesia and perineal relaxation are also important for instrumental (forceps, vacuum) vaginal deliveries. Neuraxial techniques can optimize anesthetic conditions for these obstetric procedures (see Chapter 23).
External Cephalic Version
Singleton breech presentations occur in 3% to 4% of term pregnancies. The Royal College of Obstetricians and Gynaecologists21 and the American College of Obstetricians and Gynecologists (ACOG)22 caution against a vaginal breech delivery, given the increased risk for emergency cesarean delivery and neonatal injury. External cephalic version (ECV), a procedure by which manual external pressure is applied to the maternal abdomen to change the fetal presentation from breech to cephalic, remains a viable option. ECV is usually performed between 36 and 39 weeks’ gestation.22
Neuraxial analgesia or anesthesia has been observed to increase the success of an ECV of a fetus with a breech presentation (see Chapter 35). Two recent, independent meta-analyses both concluded that the use of neuraxial blockade resulted in a significant improvement in the ECV success rate.23,24 Both randomized and nonrandomized studies have indicated that the use of neuraxial blockade improves the overall success rate by 13% to 50%. Moreover, in these studies, the use of neuraxial blockade did not appear to compromise maternal and fetal safety, and specifically it did not increase the incidence of fetal bradycardia, placental abruption, or fetal death.
Intrauterine Resuscitation
Evidence of intrapartum fetal compromise (nonreassuring fetal status) should prompt the obstetric team (including obstetric and anesthesia providers and nurses) to attempt intrauterine fetal resuscitation (Box 26-4).
In cases of uterine tachysystole, the administration of nitroglycerin (50 to 100 µg intravenously) may provide rapid onset (40 to 50 seconds) uterine relaxation.25 Higher doses of intravenous nitroglycerin (200 to 500 µg) have been described for uterine relaxation in other settings (e.g., internal podalic version, ECV, uterine prolapse)26; to date, a nitroglycerin dose-response study evaluating uterine tone as well as side effects (e.g., hypotension) has not been performed. Nitroglycerin may also be administered via other routes (e.g., sublingual, topical), but the bioavailability associated with the use of these routes is different and highly variable. For example, three sprays of sublingual nitroglycerin (400 µg/spray) have been used for uterine tocolysis27; however, the bioavailability of nitroglycerin by this route is approximately 38%. Nitroglycerin relaxes the uterus through the production of nitric oxide in uterine smooth muscle.28 Although the use of nitroglycerin has not been uniformly demonstrated to be superior to placebo for the promotion of uterine relaxation,29 a number of reports have indicated its value in cases requiring acute tocolysis.30 Nitroglycerin does not provide total relaxation of the cervix because the majority (85%) of cervical fibers are fibrous in origin.31
Preparation for Anesthesia
The anesthetic management of cesarean delivery may depend in part on the obstetric indications for operative delivery. The anesthesia provider should consider the patient’s medical, surgical, and obstetric history, the presence or absence of labor, the urgency of the delivery, and the resources available in preparing for a cesarean delivery.
Preanesthetic Evaluation
All women admitted for labor and delivery are potential candidates for the emergency administration of anesthesia, and an anesthesia provider ideally should evaluate every woman shortly after admission. Optimally, for high-risk patients, preanesthesia consultation should occur in the late second or early third trimester, even if a vaginal delivery is planned. This practice offers the opportunity to provide patients with information, solicit further consultations, optimize medical conditions, and discuss plans and preparations for the upcoming delivery.32,33 Early communication among the members of the multidisciplinary team is encouraged.34 In some cases, the urgent nature of the situation allows limited time for evaluation before induction of anesthesia and commencement of surgery; nonetheless, essential information must be obtained and risks and benefits of alternative anesthetic management decisions should be considered.
A focused preanesthetic history and physical examination includes (1) a review of maternal health and anesthetic history, relevant obstetric history, allergies, and baseline blood pressure and heart rate measurements; and (2) performance of an airway, heart, and lung examination consistent with the American Society of Anesthesiologists (ASA) guidelines (see Appendix B).34,35
Informed Consent
Recognized by the courts as early as the 18th century, the concept of informed medical consent was defined in 1957 as a requirement that the physician explain to the patient the “risks, benefits, and alternatives” of a procedure.36 The ethical issues in obtaining consent from the obstetric patient can be challenging because of the clinical situations encountered, such as (1) the pain and stress of labor; (2) birth plans (in which the patient dictates in advance those interventions that are “acceptable” and “not acceptable”); (3) rapidly changing maternal and fetal status, often requiring emergency care; and (4) fetal considerations, which may involve consideration of extrauterine viability and the definition of independent moral status (i.e., the existence of fetal rights equal to those of the mother). Discussion of this last issue may invoke theological, moral, ethical, and philosophical arguments (see Chapter 33).
Informed consent has the following three elements: threshold, information, and consent (Box 26-5).37
Threshold Elements
Threshold elements include the ability of the patient to meet the basic definition of competence, which refers to the patient’s legal authority to make a decision about her health care. Although some cognitive functions may be compromised by the effects of pain, exhaustion, and analgesic drugs,38 evidence suggests that most laboring women retain the capacity to hear and comprehend information during the consent process.36
Information Elements
The premise that a patient should be informed about the risks of a planned procedure in a language that she understands is the basis for the information elements of the consent process. In part, the difficulty with obtaining informed consent for anesthesia lies in determining the incidence of anesthesia-related morbidity and mortality. Jenkins and Baker39 surveyed the risks associated with anesthesia and compared them with risks inherent in daily living to provide contextual comparisons for patients. The investigators concluded that the perceptions regarding anesthesia risks held by anesthesia providers, surgeons, and the public are somewhat optimistic and that the consent process should include a more realistic and comprehensive disclosure.
A second difficulty is determining what risks require disclosure. White and Baldwin40 stated:
Anesthesia is by nature a practical specialty; every procedure [is] performed carrying a range of risks, which may be minor or major in consequence, common or rare in incidence, causal or incidental to the harm sustained (if any), convenient or inconvenient in timing, expected or unexpected, relative or absolute, operator-dependent or any combination of the above. In addition, there are significant difficulties in communicating risk, caused by patient perceptions, anaesthetist perceptions and the doctor-patient interaction, and complicated by the range of communication methods (numerical, verbal, or descriptive).
A survey conducted among obstetric anesthesia providers in the United Kingdom and Ireland found a consensus that the following neuraxial anesthetic risk factors should be disclosed: (1) the possibility of intraoperative discomfort and a failed/partial blockade, (2) the potential need to convert to general anesthesia, (3) the presence of weak legs, (4) hypotension, and (5) the occurrence of an unintentional dural puncture (with the use of an epidural technique).41 Backache and urinary retention were considered “optional” for discussion, and the risk for paraplegia was considered unworthy of mention unless the patient specifically asked about it.41
Among obstetric patients, the desire for risk disclosure varies. In a study from Australia, Bethune et al.42 reported a significant range (between 1 : 1 and 1 : 1 billion) in the level of risk for complications of epidural analgesia at which pregnant women wished to be informed. In a similar study from the United Kingdom in which the risks associated with general anesthesia were discussed, Jackson et al.43 found that 50% of pregnant women wished to know all risks that occurred at a frequency of greater than 1 : 1000. Overall, pregnant women appear to want more rather than less information regarding the risks of anesthetic interventions.44
Consent Elements
In obtaining consent, care must be taken to preserve patient autonomy by providing information in a noncoercive, nonmanipulative manner (i.e., avoiding a paternalistic or maternalistic approach). Barkham et al.37 observed that there are occasions when noncoercive forms of influence may be appropriate and that reasoned argument can be used to persuade patients of the merits of a particular course of action. For example, a woman with anatomy consistent with a difficult airway who is requesting general anesthesia for an elective cesarean delivery may reconsider her choice after rational persuasion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree