Anaerobic Bacterial Infections
Ayesha Mirza and Mobeen H. Rathore
Anaerobes form the predominant bacterial components of the normal human skin and mucous membranes. They are responsible either alone or in combination with aerobes for a wide variety of infections ranging from superficial skin infections to intra-abdominal and intracranial infections.
 EPIDEMIOLOGY AND PATHOGENESIS
EPIDEMIOLOGY AND PATHOGENESIS
Anaerobic organisms are widely distributed in nature. They are present in the soil as well as the skin, mucous membranes, and gastrointestinal tracts of animals and humans. Only a few of these organisms have been identified as responsible for disease in humans (eTable 249.1  ).
).
Infection with these organisms usually results secondary to disruption in the normal skin or mucous membrane barriers of the host, resulting in entry of the bacteria into deeper tissues and leading to, at times, potentially severe infections from an individual’s own endogenous flora. Although some are strict anaerobes, others may be facultative anaerobes, able to survive in conditions with or without oxygen. The presence of devitalized tissues, low oxygen tension, and low pH serve to greatly contribute to the pathogenesis of anaerobic infections. Other conditions that may play a role include host defense mechanisms, virulence factors (bacterial adherence factors), production of toxins (eg, Clostridium species), and the presence of other bacteria in polymicrobial infections.
Due to their fastidious nature, as well as inconsistent use of adequate methods for isolation and identification, anaerobic bacteria are not easily isolated, which makes their exact frequency difficult to ascertain.1 Although anaerobes have been reported to account for 8% to 11% of episodes of bacteremia in adults, anaerobic organisms have rarely been isolated from blood cultures in pediatric patients.2,3 This may partly be explained by higher prevalence of chronic or debilitating conditions in adults, like malignant neoplasms, secondary immunodeficiencies, diabetes, obstetric and gynecologic surgery, and the presence of decubitus ulcers.
 CLINICAL MANIFESTATIONS
CLINICAL MANIFESTATIONS
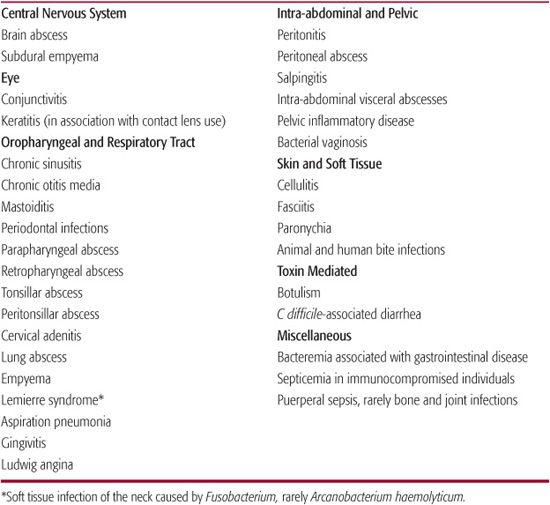
Commonly encountered diseases caused by anaerobic bacteria in children are listed in Table 249-1. The principal sites of infection are deep soft tissue infections around the mouth and oropharynx, peritonitis and peritoneal abscesses following appendicitis, or bowel rupture, and brain and lung abscesses. In females, beyond menarche, anaerobic bacteria may cause different pelvic infections, such as salpingitis, tuboovarian abscesses, pelvic inflammatory disease, as well as bacterial vaginosis. Recently, various eye infections have been associated with contact lens use, such as conjunctivitis and keratitis. Overuse of antibiotics leading to pseudomembranous colitis, which may be quite refractory to treatment, has also emerged as a significant problem, more so in adults than in children.
Clinically differentiating anaerobic from aerobic infections is often difficult. Although anaerobic infections may be more putrid, there is generally no gas formation unless C perfringens are present. Bacteremia, although rare, has been associated with a high mortality rate (15%–35%) and is invariably secondary to a primary focal infection.2 Disease in neonates and immunocompromised children is often more severe and needs to be recognized and treated early.
Central Nervous System Infections
Although not commonly isolated, anaerobes can cause a variety of central nervous system infections including those that are relatively common (ie, brain abscess, subdural empyema) to the rare epidural abscess and meningitis. Chronic infections of the adjacent structures (ie, ears, mastoids, sinuses, and teeth) commonly predispose to these infections, either as a result of direct extention or less commonly due to bacteremia. Meningitis may also follow the infection of a cerebrospinal fluid shunt with skin flora such as Propionibacterium acnes. Anaerobes of enteric origin (ie, Bacteroides fragilis) may be isolated when these shunts perforate the gut. Following intracranial surgery or trauma, infections with Clostridium perfringens tend to be seen more commonly than infections with the other anaerobes. Respiratory and dental infections leading to brain abscess as a secondary complication are generally caused by Prevotella, Porphyromonas, Bacteroides, Fusobacterium, and Peptostreptococcus, as well as microaerophilic and other streptococci.1
Treatment generally consists of aspiration along with appropriate antimicrobial therapy that includes metronidazole, penicillins, and carbapenems. Chloramphenicol may also be considered in this situation when there is no other alternative.
Ocular Infections
Recent studies illustrate the importance of anaerobic bacteria in ocular infections such as conjunctivitis, keratitis, and dacrocystitis. Although anaerobes are part of the normal flora of the conjunctival sac, this does not exclude their ability to become pathogenic given the correct milieu (eg, injuries, foreign bodies, and underlying diseases). Apart from this direct contamination is a frequent mode of transmission. In studies that employed adequate methods for isolation, anaerobes were recovered from about a third of patients with conjunctivitis, half of the time in pure culture.4
Table 249-1. Anaerobic Bacterial Infections in Children
Conjunctivitis associated with anaerobic bacteria is not distinguishable from inflammation caused by other bacteria, although patients who use contact lenses may be at higher risk of developing infections caused by these organisms. Although the vast majority of cases of acute conjunctivitis, are caused by viruses as well as aerobic bacteria, such as Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae, anaerobic gram-positive cocci (eg, Peptosteptococcus) have also been recovered in significant numbers from these patients. Other bacteria that have been recovered include Propionobacterium, B fragilis, pigmented Prevotella, Porphyromonas, Fusobacteria, and Bifidobacteria. Often these are found in conjunction with other aerobic bacteria. In addition to this, Chlamydia trachomatis and Neisseria gonorrheae have been isolated from sexually active adolescents. Corneal ulcerations on the other hand have been associated with S pneumoniae, Pseudomonas species, and Peptostreptococcus.
Keratitis, a relatively serious infection that may result in corneal scarring, opacification, and blindness, although mostly associated with a variety of aerobic gram-positive and gram-negative bacteria, has been reported in conjunction with Clostridium perfringens, in which case it can result in a fulminant endophthalmitis. This has been associated with perforating ocular injuries. Clostridium tetani has also been associated with ocular trauma. Corneal susceptibility to infection is secondary to its continuous exposure, as well as avascularity. Anaerobic bacteria should also be considered in cases of chronic dacrocystitis.
The treatment for anaerobic ocular infections depends on the severity as well as the site of infection. Simple cases of conjunctivitis may be treated with topical antibiotics. Bacitracin is very effective against pigmented Prevotella and Porphyromonas as well as Peptosptreptococcus species but is usually not effective against B fragilis and Fusobacterium. Similarly, erythromycin is active against pigmented Prevotella and Porphyromonas, miroaerophilic and anaerobic streptococci, Clostridium species, as well as gram-positive non-spore-forming anaerobic bacilli but has poor activity against gram-negative anaerobic bacilli. Chloramphenicol has very good activity against most anaerobes, however, caution should be used even when used topically because absorption from the conjunctivae can occur and may rarely cause aplastic anemia even when administered locally. Sulfonamides, quinolones, polymyxin B, and aminoglycoside preparations may also not be very effective against most anaerobes. The newer third- and fourth-generation quinolones, such as levofloxacin and moxifloxacin, have shown better activity than ciprofloxacin and ofloxacin, including superior activity against the gram-positive organisms that are most commonly involved in keratitis and endophthalmitis.5
Complications such as the presence of a corneal ulcer as well as more severe infections involving the lacrimal glands and cases of endophthalmitis will need to be treated aggressively with broad-spectrum antimicrobials that include anaerobic coverage. In addition, early surgical intervention should be initiated where indicated. Every effort should be made to send appropriate aerobic and anaerobic cultures. This applies particularly to neonates with blockage of the nasolacrimal duct where infection is often a concern.
Head and Neck Infections
Anaerobes may be isolated in cases of acute as well as chronic infections involving the ears, sinuses, mastoids, and other head and neck structures.6 Members of the oropharyngeal flora (ie, Prevotella, Porphyromonas, Bacteroides, Fusobacterium, and Peptostreptococcus) are the predominant anaerobic flora involved in these infections. In addition to these, Streptococcus salivarius and microaerophilic streptococci may be involved in the pathogenesis of dental infections.
Anaerobes have been isolated from approximately 5% to 15% of cases of acute otitis media as well as 50% of cases of chronic suppurative otitis media, including those with the presence of a cholesteotoma. These can accelerate the absorption of bone which is enhanced by organic acids produced by anaerobic bacteria.1,7-9
Recovery of anaerobes in up to 75% of tonsils of children with recurrent group A beta hemolytic streptococcus (GABHS) as well as 40% of those with non-GABHS has been one of the possible explanations offered for the failure of penicillin to treat these infections. Selection of beta-lactamase producing strains of aerobic as well as anaerobic bacteria may render penicillin ineffective in these situations.1,10-12
Other infections, such as thyroiditis, have been associated with anaerobic bacteria, such as anaerobic gram-negative bacteria as well as Peptostreptococcus species.
Lemierre Syndrome
Human infection with Fusobacterium necrophorum usually involves F necrophorum subsp funduliforme as opposed to infection with F necrophorum subsp necrophorum, which is a common pathogen in animals. Lemierre syndrome, or postanginal sepsis, is the most common life-threatening manifestation. Tonsillitis is followed by septic thrombophlebitis of the internal jugular vein and is then followed by septicemia with septic emboli in lungs and other sites.13
Recent evidence suggests that F necrophorum can be limited to the throat and cause persistent or recurrent tonsillitis. F necrophorum is unique among non-spore-forming anaerobes, mainly for its virulence and association with Lemierre syndrome as a monomicrobial infection and also because it seems probable that it may be an exogenously acquired infection. The source of infection is unclear; suggestions include acquisition from animals or human-to-human transmission. Approximately 10% of published cases are associated with infectious mononucleosis, which may facilitate invasion. Recent work suggests that genetic mutations leading to hypercoagulability may predispose to internal jugular vein thrombophlebitis when infected with fusobacterium.13 Lemierre syndrome was a relatively common entity in the preantibiotic era but seemed to virtually disappear with widespread use of antibiotics for upper respiratory tract infection. In the last several years, however, there has been a rise in incidence, possibly related to a decrease in antibiotic usage for sore throat. Coinfection with Fusobacterium necrophorum and Arcanobacterium haemolyticum in a case of Lemierre syndrome has been reported.14
Pleuropulmonary Infections
Severe periodontal or gingival disease as well as aspiration of oropharyngeal secretions or gastric contents are the major risk factors associated with the development of pleuropulmonary disease which can range from uncomplicated pneumonia to severe necrotizing pneumonia with the formation of empyema or lung abscess. Like most anaerobic infections, these are generally polymicrobial in nature. The predominant anaerobes to be isolated in these situations include Prevotella, Porphyromonas, Fusobacterium, and Peptostreptococcus. These may be mixed with aerobic organisms such as alpha hemolytic as well as microaerophilic streptococci and in nosocomial-acquired pneumonia gram-negative organisms such as Pseudomonas spp, Enterobacteriaceae. S aureus may be isolated as well.15
Intra-abdominal Infections
Perforation of abdominal viscera, either traumatically or during surgery, may lead to peritonitis as well as the formation of intra-abdominal abscesses. The specific microorganisms involved here are the normal flora of the gastrointestinal tract where the anaerobic bacteria outnumber aerobes in a ratio of 1:1000 to 1:10,000. These infections often tend to be biphasic, with the initial infection being caused by Enteriobacteriaceae followed by a later phase with the development of abscesses from which B fragilis or Peptostreptococcus may be isolated. Because Bacteroides species tend to make up 25% of the anaerobes in the gut, infections with these organisms are seen most commonly. Members of the Clostridium species are another common group of anaerobic organisms to be isolated in these situations. Combination therapy is generally initiated, often incorporating an aminoglycoside along with a penicillin-beta-lactamase (ie, ticarcillin-clavulanate) or third- or fourth-generation cephalosporin and, depending on the severity of the illness, a carbapenem.1
Osteomyelitis and Septic Arthritis
These infections also tend to be polymicrobial with osteomyelitis after trauma and fracture most commonly involving the long bones, whereas osteomyelitis involving the spine may be seen following decubitus ulcers. Cranial and facial bones may be involved as well, particularly following trauma.1
Anaerobic streptococci and Bacteroides are the most common organisms at all sites, including bites and cranial infections. Pigmented Prevotella as well as Porphyromonas are other common organisms isolated in these infections. Clostridia may be isolated in compound fractures involving the lower extremities and pelvis.
Septic arthritis involving anaerobes may be seen following hematogenous or direct spread of infection, trauma, as well as in association with prosthetic joints.
Infections of the Female Genital Tract Including Pelvic Inflammatory Disease
Genital tract infections mimic other infections caused by anaerobes in the sense that they are usually polymicrobial. This includes bacterial vaginosis, endometritis, salpingitis, tuboovarian abscesses, as well as intrauterine-device-associated infections. The predominant anaerobic bacteria include Prevotella species, Peptostreptococcus, Porphyromonas, and Clostridium species.
In addition to these infections, more than one million women in the United States are treated for pelvic inflammatory disease (PID) annually. Although C trachomatis and N gonorrheae are the organisms most frequently associated with PID, up to 70% of cases are neither gonococcal nor chlamydia related. Anaerobic gram-negative rods are frequently involved in these infections, although isolation is often difficult for reasons mentioned elsewhere in this chapter. Treatment includes the use of doxycycline or a macrolide in combination with cefoxitin, cefotetan, clindamycin, or metronidazole. Recently, randomized clinical trials using moxifloxacin, ofloxacin, clindamycin-ciprofloxacin, and azithromycin among women with mild to moderate PID found clinical cure rates of 90% to 97%. Although single-drug therapy holds promise for milder cases, further studies are needed to show the efficacy of these regimens in treating anaerobes associated with these regimens as well as preventing adverse reproductive sequelae, the ultimate goal for effective and early treatment of PID.16
Neonatal Infections
In addition to infections in older children, anaerobes colonize the newborn during vaginal delivery and have been recovered from several types of newborn infections, including cellulitis, aspiration pneumonia, bacteremia, conjunctivitis, omphalitis, and infant botulism. The wide range of endogenous infections caused by anaerobes in neonates as well as older children is not surprising being that they form the predominant component of the normal human skin and mucosa.
 DIAGNOSIS
DIAGNOSIS
Given the overall low incidence of anaerobic infections in children, the routine use of anaerobic blood cultures in childhood illness has been debated. However, with the reemergence of anaerobic bacteremia, the evidence favors obtaining anaerobic blood cultures.2,17,18 Diagnosis made on clinical grounds can prove difficult because the clinical features of anaerobic bacteremia are not very different from those associated with other types of bacteremias in children. Diagnosis may also be delayed due to the more fastidious growth requirements and time needed for identification of these bacteria. Knowledge of host risk factors as well as organ system involved may aid in the diagnosis. Presence of a foul odor in the clinical specimen or site from which the specimen was obtained may also provide a useful clue to the diagnosis. Antimicrobial susceptibility studies for anaerobic bacteria are often not available from hospital laboratories; however, they should be requested in exceptional and life-threatening cases.
 TREATMENT
TREATMENT
Because of the mortality associated with anaerobic infections, it is important to establish timely appropriate therapy. Infections involving anaerobes are often polymicrobial making antibiotic combinations useful. Patients should be started on broad-spectrum antibiotics effective against aerobic as well as anaerobic organisms. Site of the infection, antimicrobial resistance patterns when available, pharmacokinetics of the different drugs used, as well as potential side effects should all be taken into consideration when deciding on an antimicrobial agent. Penicillin G remains the drug of choice against most non-beta-lactamase-producing organisms, including anaerobic streptococci, Clostridium species other than C difficile, and nonsporulating anaerobic bacilli. This makes it appropriate for treatment of most oropharyngeal infections. Metronidazole and clindamycin have excellent activity against anaerobes, including those producing β-lactamase (eg, Bacteroides). Clindamycin is superior to penicillin for serious lung infections. Antibiotic combinations with β-lactamase inhibitors (amoxicillin/clavulanic acid, ticarcillin/clavulanic acid, ampicillin/sulbactam, piperacillin/tazobactam) have become increasingly popular due to their broad-spectrum aerobic and anaerobic activity as well as the ability to overcome β-lactamase production. Second-generation cephalosporins cefotetan and cefoxitin also have good anaerobic activity, although cefoxitin is relatively inactive against most species of clostridium except C perfringens.
The carbapenems (imipenem, ertapenem, meropenem) all have excellent anaerobic activity. Chloramphenicol also has excellent in vitro activity against most anaerobes; however, its use has been limited by the availability of safer antibiotics. The macrolides have moderate to good in vitro activity against anaerobic bacteria other than B fragilis and Fusobacterium. Although the newer quinolones (moxifloxacin, levofloxacin) have better anaerobic activity especially against the B fragilis group, their use in children is limited due to the possible adverse effects on cartilage. Vancomycin has good activity against all gram-positive anaerobes including C difficile.1
In addition to antimicrobial therapy, drainage of any abscesses and debridement of necrotic tissue are important. Certain types of adjunct therapy, such as hyperbaric oxygen, although controversial may also be considered in certain circumstances.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


