Tanner JL, Stein MT, Olson LM, Frintner MP, Radecki L: Reflections on well-child care practice: a national study of pediatric clinicians. Pediatrics 2009 Sep;124(3):849–857 [Epub 2009 Aug 10] [PMID: 19706587].
PEDIATRIC HISTORY
A unique feature of pediatrics is that the history represents an amalgam of parents’ objective reporting of facts (eg, fever for 4 days), parents’ subjective interpretation of their child’s symptoms (eg, infant crying interpreted by parents as abdominal pain), and for older children their own history of events. Parents and patients may provide a specific and detailed history, or a vague history that necessitates more focused probing. Parents may or may not be able to distinguish whether symptoms are caused by organic illness or a psychological concern. Understanding the family and its hopes for and concerns about the child can help in the process of distinguishing organic, emotional, and/or behavioral conditions, thus minimizing unnecessary testing and intervention.
Although the parents’ concerns need to be understood, it is essential also to obtain as much of the history as possible directly from the patient. Direct histories not only provide firsthand information but also give the child a degree of control over a potentially threatening situation and may reveal important information about the family.
Obtaining a comprehensive pediatric history is time consuming. Many offices provide questionnaires for parents to complete before the clinician sees the child. Data from questionnaires can make an outpatient visit more productive, allowing the physician to address problems in detail while more quickly reviewing areas that are not of concern. Questionnaires may be more productive than face-to-face interviews in revealing sensitive parts of the history. Developmental and mental health screening saves provider time and the results when reviewed with the parent or family member can yield critical information. However, failure to review and assimilate this information prior to the interview may cause a parent or patient to feel that the time and effort have been wasted.
Elements of the history that will be useful over time should be readily accessible in the medical record. In absence of an electronic medical record, such information can be accumulated on a summary sheet, as illustrated in Figure 9–1. Demographic data; a problem list; information about chronic medications, allergies, and previous hospitalizations; and the names of other physicians providing care for the patient are commonly included. Documentation of immunizations, including all data required by the National Childhood Vaccine Injury Act, should be kept on a second page.
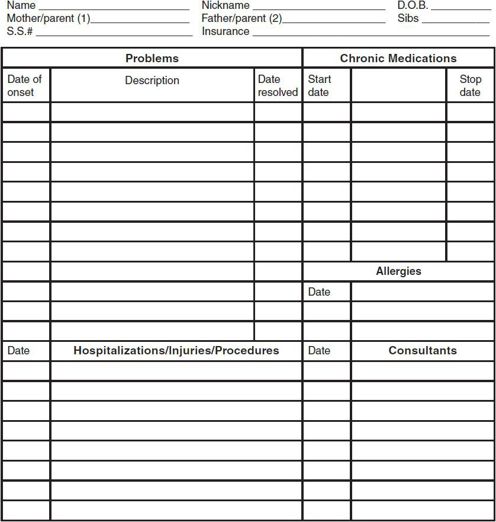
 Figure 9–1. Use of a summary sheet such as this at the front of the chart or the electronic medical record facilitates reorienting the caregiver and his or her partners to the patient. Some practices keep track of health supervision visits on this sheet to tell the physician whether the child is likely to have received the appropriate preventive services. A second page documenting immunizations should record data required by the National Childhood Vaccine Injury Act. When an allergy with potential for anaphylaxis is identified, the patient should wear a medical alert bracelet and obtain an epinephrine kit, if appropriate.
Figure 9–1. Use of a summary sheet such as this at the front of the chart or the electronic medical record facilitates reorienting the caregiver and his or her partners to the patient. Some practices keep track of health supervision visits on this sheet to tell the physician whether the child is likely to have received the appropriate preventive services. A second page documenting immunizations should record data required by the National Childhood Vaccine Injury Act. When an allergy with potential for anaphylaxis is identified, the patient should wear a medical alert bracelet and obtain an epinephrine kit, if appropriate.
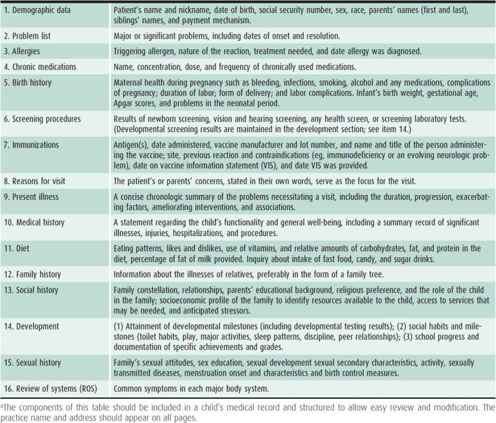
The components of a comprehensive pediatric history are listed in Table 9–1. The information should, ideally, be obtained at the first office visit. The first seven items may be included on a summary sheet at the front of the medical record. Items 8 and 9, and a focused review of systems, are dealt with at each acute or chronic care visit. The entire list should be reviewed and augmented with relevant updates at each health supervision visit.
PEDIATRIC PHYSICAL EXAMINATION
During the pediatric physical examination, time must be taken to allow the patient to become familiar with the examiner. Interactions and instructions help the child understand what is occurring and what is expected. A gentle, friendly manner and a quiet voice help establish a setting that yields a nonthreatening physical examination. The examiner should take into consideration the need for a quiet child, the extent of trust established, and the possibility of an emotional response (crying!) when deciding the order in which the child’s organ systems are examined. Painful or unpleasant procedures (eg, otoscopic examination) should be deferred until the end of the examination. Whether or not the physician can establish rapport with the child, the process should proceed efficiently and systematically.
Table 9–1. Components of the pediatric historical database.a
Because young children may fear the examination and become fussy, simple inspection is important. For example, during an acute-care visit for fever, the examiner should observe the child’s skin color and work of breathing prior to beginning the examination. During a health supervision visit, observation will provide the examiner with an opportunity to assess parent-child interactions.
Clothing should be removed slowly and gently to avoid threatening the child. A parent or the child is usually the best person to do this. Modesty should always be respected, and gown or drapes should be provided. Examinations of adolescents should be chaperoned whenever a pelvic examination or a stressful or painful procedure is performed.
Examination tables are convenient, but a parent’s lap is a comfortable location for a young child. For most purposes, an adequate examination can be conducted on a “table” formed by the parent’s and examiner’s legs as they sit facing each other.
Although a thorough physical examination is important at every age, certain components of the examination may change based on the age of the patient. An astute clinician can detect signs of important clinical conditions in an asymptomatic child. In infancy, for example, physical examination can reveal the presence of craniosynostosis, congenital heart disease, or developmental dysplasia of the hip. Similarly, examination of a toddler may reveal pallor (possible iron-deficiency anemia) or strabismus. The routine examination of an older child or adolescent may reveal scoliosis or acanthosis nigricans (a finding associated with insulin resistance).
HEALTH SUPERVISION VISITS
One of several timetables for recommended health supervision visits is illustrated in Figure 9–2. (Note: A PDF printable format of this figure is available from the American Academy of Pediatrics [AAP].) The federal Maternal and Child Health Bureau has developed comprehensive health supervision guidelines through their Bright Futures program. In areas where evidence-based information is lacking, expert opinion has been used as the basis for these plans. Recently revised Bright Futures Guidelines emphasizes working collaboratively with families, recognizing the need for attention toward children with special healthcare needs, gaining cultural competence, and addressing complementary and alternative care, as well as integrating mental health care into the primary care setting. Practitioners should remember that guidelines are not meant to be rigid; services should be individualized according to the child’s needs.
 Figure 9–2. Recommendations for preventive health care. (Hagen JF, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 3rd ed. American Academy of Pediatrics; 2008.)
Figure 9–2. Recommendations for preventive health care. (Hagen JF, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 3rd ed. American Academy of Pediatrics; 2008.)
During health supervision visits, the practitioner should review child development and acute and chronic problems, conduct a complete physical examination, order appropriate screening tests, and anticipate future developments. New historical information should be elicited through an interval history. For example, “Since your last visit have there been any changes in your child and family’s life that I should be aware of?” Development should be assessed by parental report, clinician observation, and a formal screening tool at each visit. Developmental surveillance with systematic use of parent-directed questionnaires or screening tools such as the Ages and Stages Questionnaire (ASQ) or the Parents’ Evaluation of Developmental Status (PEDS) is a growing trend. Growth parameters should be carefully recorded, and weight, length or height, head circumference (up to age 3), and body mass index (BMI) (for > 2 years) should be plotted and evaluated using established growth charts (see Chapter 3). Vision and hearing should be assessed subjectively at each visit, with objective assessments at intervals beginning after the child is old enough to cooperate with the screening test, usually at 3–4 years of age. Various laboratory screening tests may also be part of the visit.
Because fewer than 4% of asymptomatic children have physical findings on routine health maintenance visits, a major portion of the health supervision visit is devoted to anticipatory guidance. This portion of the visit enables the healthcare provider to address behavioral, developmental, injury prevention, and nutritional issues; school problems; and other age-appropriate issues that will arise before the next well-child visit.
American Academy of Pediatrics Committee on Practice and Ambulatory Medicine: Recommendations for preventive pediatric health care. Pediatrics 2007;120:1376 [PMID: 2479904].
Bright Futures Guidelines, 3rd ed. http://brightfutures.aap.org/3rd_
Edition_Guidelines_and_Pocket_Guide.html. Accessed August 24, 2009.
Dinkevich E, Ozuah PO: Well-child care: effectiveness of current recommendations. Clin Pediatr 2002;41:211 [PMID: 12041716].
Radecki L, Sand-Loud N, O’Connor KG, Sharp S, Olson LM: Trends in the use of standardized tools for developmental screening in early childhood: 2002–2009. Pediatrics 2011 Jul;128(1):14–19 doi: 10.1542/peds.2010-2180 [Epub 2011 Jun 27] [PMID: 21708798].
DEVELOPMENTAL & BEHAVIORAL ASSESSMENT
Addressing developmental and behavioral problems is one of the central features of pediatric primary care. The term developmental delay refers to the circumstance in which a child has not demonstrated a developmental skill (such as walking independently) by an age at which the vast majority of normally developing children have accomplished this task. Developmental delays are, in fact, quite common: approximately 18% of children younger than 18 years either have developmental delays or have conditions that place them at risk of developmental delays.
Pediatric practitioners are in a unique position to assess the development of their patients. This developmental assessment should ideally take the form of developmental surveillance, in which a skilled individual monitors development in multiple domains (gross motor, fine motor, language, and personal/social) over time as part of providing routine care. Developmental surveillance includes several key elements: listening to parent concerns; obtaining a developmental history; making careful observations during office visits; periodically screening all infants and children for delays using validated screening tools; recognizing conditions and circumstances that place children at increased risk of delays; and referring children who fail screening tests for further evaluation and intervention.
The prompt recognition of children with developmental delays is important for several reasons. Children with delays can be referred for a wide range of developmental therapies, such as those provided by physical, speech/language, and/or educational therapists. Children with delays, regardless of the cause, make better developmental progress if they receive appropriate developmental therapies than if they do not. Many infants and toddlers younger than 3 years with delays are eligible to receive a range of therapies and other services, often provided in the home, at no cost to families. Children aged 3 years and older with delays are eligible for developmental services through the local school system.
Although the benefits of early detection of developmental delays are clear, it is often difficult to incorporate developmental surveillance into busy outpatient practice. Many pediatric practitioners do not use a formal screening tool but rely on their own clinical judgment. However, when screening tests are not used, delays are often not detected until school age, particularly when the delays are not severe. There are several practical barriers to performing routine surveillance using standardized screening tools: perceived lack of time to screen all children at every well-child visit, lack of familiarity with the various screening tools, not wanting to concern parents by identifying a possible delay, and not knowing where in the community to refer patients with suspected delays. There are some solutions to these barriers, such as using parent developmental questionnaires rather than provider-administered tests to save time, become familiar with one or two screening tests, and making use of Internet-based resources. For example, the National Dissemination Center for Children With Disabilities maintains a website with links to a wide variety of resources in each state (http://www.nichcy.org).
Several parent- and physician-administered developmental screening tools are available. The PEDS, ASQ, and the Child Development Inventories (CDI) are screening tests that rely on parent report. Other screening tools, such as the Denver II screening test (reproduced in Chapter 3, Figure 3–12), the Early Language Milestone Scale (see Chapter 3, Figure 3–11), and the Bayley Infant Neurodevelopmental Screener, involve the direct observation of a child’s skills by a care provider. All developmental screening tests have their strengths and weaknesses. The Denver II is familiar to many pediatric providers and is widely used. However, whereas the Denver II has relatively high sensitivity for detecting possible developmental delays, the specificity is poorer, and this may lead to the overreferral of normal children for further developmental testing.
In addition to general developmental screening, autism-specific screens (such as the Modified Checklist for Autism in Toddlers [MCHAT]) should be administered at the 18- and 24-month health supervision visits.
Regardless of the approach taken to developmental screening, there are a number of important considerations: (1) The range of normal childhood development is broad, and therefore a child with a single missing skill in a single developmental area is less likely to have a significant developmental problem than a child showing multiple delays in several developmental areas (eg, gross motor and language delays); (2) continuity of care is important, because development is best assessed over time; (3) it is beneficial to routinely use formal screening tests to assess development; (4) if developmental delays are detected in primary care, these patients need referral for further testing and likely will benefit from receiving developmentally focused therapies; and (5) parents appreciate when attention is paid to their child’s development and generally react positively to referrals for appropriate developmental therapies.
Several developmental charts with age-based expectations for normal development are presented in Chapter 3 (see Tables 3–1 through 3–3), as well as a discussion of the recommended medical and neurodevelopmental evaluation of a child with a suspected developmental disorder.
In addition to developmental issues, pediatric providers are an important source of information and counseling for parents regarding a broad range of behavioral issues. The nature of the behavioral problems, of course, varies with the child’s age. Some common issues raised by parents, discussed in detail in Chapter 3, include colic, feeding disorders, sleep problems, temper tantrums, breath-holding spells, and noncompliance. Behavioral issues in adolescents are discussed in Chapter 4.
American Academy of Pediatrics Council on Children With Disabilities: Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics 2006; 118:1808 [PMID: 168118591].
Godoy L, Carter AS: Identifying and addressing mental health risks and problems in primary care pediatric settings: a model to promote developmental and cultural competence. Am J Orthopsychiatry 2013 Jan;83(1):73–88 doi: 10.1111/ajop.12005 [PMID: 23330625].
GROWTH PARAMETERS
Monitoring appropriate growth is pivotal in ambulatory pediatric practice.
Height, weight, and head circumference are carefully measured at each well-child examination and plotted on age- and sex-specific charts. The Centers for Disease Control and Prevention (CDC) recently recommended use of the World Health Organization (WHO) growth standards to monitor growth for infants and children ages 0–2 in the United States, in lieu of its own growth charts. The WHO standards are based on a sample of 8500 babies (from Brazil, Ghana, India, Norway, Oman, and the United States) who were predominantly breast-fed for at least 4 months, still nursing at 1 year and living in nonsmoking households. The methods used to create the CDC growth charts and the WHO growth charts are similar for children aged 2 years and older.
To ensure accurate weight measurements for longitudinal comparisons, infants should be undressed completely and young children should be wearing underpants only. Recumbent length is plotted on the chart until approximately 2 years of age. When the child is old enough to be measured upright, height should be plotted on the charts for ages 2–20 years. Routine measurements of head circumference may cease if circumferential head growth has been steady for the first 2 years of life. However, if a central nervous system (CNS) problem exists or develops, or if the child has growth deficiency, this measurement continues to be useful. Tracking the growth velocity for each of these parameters allows early recognition of deviations from normal.
It is useful to note that in the first year of life, it is common for height and weight measurements to cross over a percentile line. After approximately 18 months, most healthy children tend to follow the curve within one growth channel.
Determination of whether or not a child’s weight falls within a healthy range also relies on growth charts. For children younger than 2 years, the weight-for-length chart is used. For children 2 to 18 years, a BMI chart is used, which is a measure that correlates well with adiposity- and obesity-related comorbidities. The BMI is calculated as the weight (in kilograms) divided by the squared height (in meters). The BMI is useful for determining obesity (BMI ≥ 95th percentile for age) and at risk for overweight (BMI between 85th and 95th percentiles), as well as underweight status (BMI ≤ 5th percentile for age). It must be emphasized that “eyeballing” overweight/underweight is frequently inaccurate and should not substitute for careful evaluation of the data on growth charts.
CDC and WHO growth charts: http://www.cdc.gov/growthcharts/. Accessed March 17, 2013.
Grummer-Strawn LM et al: Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR Recomm Rep 2010;59(RR-9):1–15 [PMID: 20829749].
Krebs NF, Jacobson MS; American Academy of Pediatrics Committee on Nutrition. Pediatrics. 2003 Aug;112(2):424–30 [PMID:12897303].
BLOOD PRESSURE
Blood pressure screening at well-child visits starts at age 3 years. There are some conditions that warrant blood pressure monitoring at an earlier age:
• History of prematurity, very low birthweight, or other neonatal complication requiring intensive care
• Congenital heart disease (repaired or nonrepaired)
• Recurrent urinary tract infections, hematuria, or proteinuria
• Known renal disease or urologic malformations
• Family history of congenital renal disease
• Solid organ transplant
• Malignancy or bone marrow transplant
• Treatment with drugs known to raise blood pressure (steroids, oral contraceptives)
• Other systemic illnesses associated with hypertension (neurofibromatosis, tuberous sclerosis, etc)
• Evidence of elevated intracranial pressure
Accurate determination of blood pressure requires proper equipment (stethoscope, manometer and inflation cuff, or an automated system) and a cooperative, seated subject in a quiet room. Although automated blood pressure instruments are widely available and easy to use, blood pressure readings from these devices are typically 5 mm Hg higher for diastolic and 10 mm Hg higher for systolic blood pressure compared with auscultatory techniques. Therefore, the diagnosis of hypertension should not be made on the basis of automated readings alone. Additionally, blood pressure varies somewhat by the height and weight of the individual. Consequently, hypertension is diagnosed as a systolic or diastolic blood pressure greater than the 95th percentile based on the age and height (or weight) percentile of the patient.
The width of the inflatable portion of the cuff should be 40%–50% of the circumference of the limb. Obese children need a larger cuff size to avoid a falsely elevated blood pressure reading. Cuffs that are too narrow will overestimate and those that are too wide will underestimate the true blood pressure. Hypertension should not be diagnosed based on readings at one visit, but rather three separate occasions of documented hypertension are required. Repeated measurements at different visits over time should be tracked using flow charts in an electronic medical record or equivalent in a paper chart. Children with repeated blood pressure readings from the 90th to the 95th percentile may be classified as having prehypertension. Those with greater than between the 95th and 99th percentile plus 5 mm of Hg are classified as Stage 1 hypertension, and those greater than the 99th percentile plus 5 mm of Hg are termed Stage 2 hypertension. National High Blood Pressure Education Program recommends that all children with blood pressure of greater than or equal to 95% should have a complete blood count (CBC), serum nitrogen, creatinine, electrolytes, fasting lipid panel, glucose, urinalysis, urine culture, renal ultrasound, echocardiogram, and retinal examination. Nonpharmacologic interventions include diet, exercise, and weight management. Indications for pharmacologic therapy may include the following:
• Symptomatic hypertension
• Secondary hypertension
• Hypertensive target-organ damage
• Diabetes (types 1 and 2)
• Persistent hypertension despite nonpharmacologic measures
Based on a recent systematic review for US Preventive Services Task Force, it is unclear whether screening for hypertension in children and teens reduces adverse outcomes in adults.
National High Blood Pressure Education Program Working Group in High Blood Pressure in Children and Adolescents: The fourth report on diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Revised 2005. http://www.nhlbi.nih.gov/guidelines/hypertension/child_tbl.pdf. Accessed November 13, 2013.
Park MK et al: Comparison of auscultatory and oscillometric blood pressures. Arch Pediatr Adolesc Med 2001;155:50 [PMID: 11177062].
Thompson M et al: Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics 2013 Mar;131(3):490–525 doi: 10.1542/peds.2012-3523 [Epub 2013 Feb 25] [PMID: 23439904]
Wiesen J et al: Evaluation of pediatric patients with mild to moderate hypertension: Yield of diagnostic testing. Pediatrics 2008;122:e988–e993 [PMID: 18977966].
VISION & HEARING SCREENING
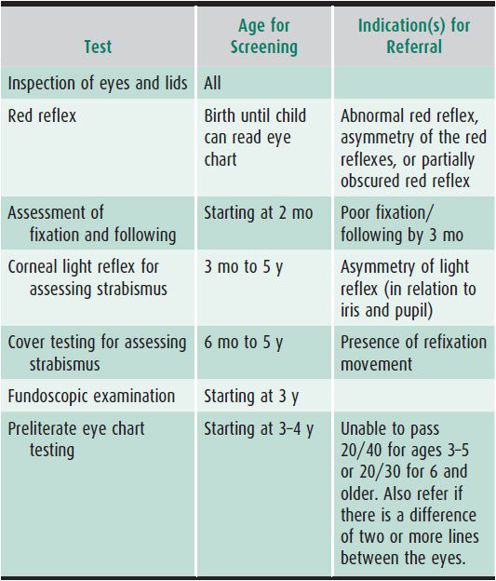
Examination of the eyes and an assessment of vision should be performed at every health supervision visit. Eye problems are relatively common in children: refractive errors (including myopia, hyperopia, and astigmatism), amblyopia (loss of visual acuity from cortical suppression of the vision of the eye), and/or strabismus (misalignment of the eyes) occur in 5%–10% of preschoolers. Assessment of vision should include visual inspection of the eyes and eyelids, alignment of eyes, and visual acuity.
From birth to 3 years of age, the movement and alignment of the eyes should be assessed and the pupils and red reflexes examined. The red reflex, performed on each pupil individually and then on both eyes simultaneously, is used to detect eye opacities (eg, cataracts or corneal clouding) and retinal abnormalities (eg, retinal detachment or retinoblastoma). By 3 months of age, an infant should be able to track or visually follow a moving object, with both eyes.
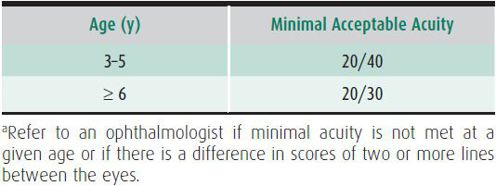
Starting at age 3, formal testing of visual acuity should be done. This can be performed in the office with a variety of tests, including the tumbling E chart or picture tests such as Allen cards. In these tests, each eye is tested separately, with the nontested eye completely covered. Credit is given for any line on which the child gets more than 50% correct. Children 4 years of age and older who are unable to cooperate should be retested, ideally within 1 month, and those who cannot cooperate with repeated attempts should be referred to an ophthalmologist. Because visual acuity improves with age, results of the test are interpreted using the cutoff values in Table 9–2. However, any two-line discrepancy between the two eyes, even within the passing range (eg, 20/20 in one eye, 20/30 in the other in a child aged ≥ 6 years) should be referred to an ophthalmologist.
Table 9–2 Age-appropriate visual acuity.a
Throughout childhood, clinicians should screen for undetected strabismus (ocular misalignment). The corneal light reflex test can be used starting at 3 months and the cover test can be used beginning at 6 months to assess for strabismus. The random dot E test may also be used for detecting strabismus. The corneal light reflex test, the cover test, and visual acuity test are described further in Chapter 16.
Recommendations for vision screening and indications for referral are listed in Table 9–3. Referral to an ophthalmologist is also recommended for preterm infants for evaluation of retinopathy of prematurity (ROP), as well as children with a family history of amblyopia, strabismus, retinoblastoma, or retinal degeneration. Children with Down syndrome should be referred to an ophthalmologist at 6 months of age given their increased risk for refractive error, strabismus, and cataracts.
Table 9–3. Recommended vision screening in the primary care office.
Hearing loss, if undetected, can lead to substantial impairments in speech, language, and cognitive development. Because significant bilateral hearing loss is one of the more common major anomalies found at birth, and early detection and intervention of hearing loss leads to better outcomes for children, universal hearing screening is provided to newborns in most parts of the United States. Hearing in infants is assessed using either evoked otoacoustic emissions or auditory brain stem-evoked responses. Because universal newborn hearing screening is sometimes associated with false-positive test results, confirmatory audiology testing is required for abnormal tests.
Informal behavioral testing of hearing, such as observing an infant’s response to a shaken rattle, may be unreliable. In fact, parental concerns about hearing are of greater predictive value than the results of informal tests, and such concerns should be taken seriously. Prior to age 4, infants should be referred to an audiologist for testing if a concern arises. Conventional screening audiometry, in which a child raises her hand when a sound is heard, can be performed starting at age 4. Each ear should be tested at 500, 1000, 2000, and 400 Hz and referred at threshold levels of greater than 20 dB at any of these frequencies. Any evidence of hearing loss should be substantiated by repeated testing, and if still abnormal, a referral for a formal hearing evaluation should be made.
The AAP periodicity schedule recommends routine hearing screening at 4, 5, 6, 8, and 10 years of age. Children with any risk factors for hearing loss should be closely followed and receive more frequent screening. A number of inherited or acquired conditions increase the risk of hearing loss. Sometimes hearing loss can be mistaken for inattention, and so hearing screening should be part of workup for attention problems. Additional details regarding hearing assessment are provided in Chapter 18.
American Academy of Pediatrics et al: Eye examination in infants, children, and young adults by pediatricians. Pediatrics 2003;111:902 [PMID: 12671132].
American Academy of Pediatrics et al: Red reflex examination in neonates, infants, and children. Pediatrics 2008;122:1401 [PMID: 19047263].
Harlor AD Bower C; American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section of Otolaryngology: Hearing assessment in infants and children: recommendations beyond neonatal screening. Pediatrics 2009;124(4):1252–1263 [PMID: 19786460].
Katbamna B, Crumpton T, Patel DR: Hearing impairment in children. Pediatr Clin North Am 2008;55:1175 [PMID: 18929059].
Tingley DH: Vision screening essentials: screening today for eye disorders in the pediatric patient. Pediatr Rev 2007;28:54 [PMID: 17272521].
SCREENING
Newborn Screening
Newborn screening involves population-wide testing for metabolic and genetic diseases. It has become an essential component in a public health program that screens over 4 million newborns every year. Blood samples are collected by heelstick from newborns before hospital discharge, and results are usually available within 1 week. Some states routinely repeat blood testing between 7 and 14 days of life, while others recommend it if the child is discharged in less than 24 hours. The state-to-state variation seen in newborn screen panels has begun to diminish as a result of national recommendations. In 2010, the Secretary Advisory Committee on Heritable Disorders in Newborns and Children recommended screening for 30 core conditions with another 26 detectable through differential diagnosis. Most states have adopted these guidelines.
Infants with a positive screening result should receive close follow-up, with additional confirmatory studies performed at a center with experience in doing these tests. Screening tests are usually accurate, but the sensitivity and specificity of a particular screening test must be carefully considered. If symptoms of a disease are present despite a negative result on a screening test, the infant should be tested further. Newborn screening has benefited thousands of infants and their families, preventing and diminishing the morbidity of many diseases. At the same time, the emotional cost of false-positive screening is a continuing challenge. Parents report high levels of stress during the evaluation process. Recommendations for useful resources, given the variability of information on the Internet, and prompt clinical services can help reduce this distress.
Calonge N et al, Advisory Committee on Heritable Disorders in Newborns and Children: Committee report: method for evaluating conditions nominated for population-based screening of newborns and children. Genet Med 2010 Mar;12(3):153–159 [PMID: 20154628].
Deluca JM, Kearney MH, Norton SA, Arnold GL: Parents’ experiences of expanded newborn screening evaluations. Pediatrics 2011 Jul;128(1):53–61 [Epub 2011 Jun 27] [PMID: 21708804].
Fernoff PM: Newborn screening for genetic disorders. Pediatr Clin North Am 2009 Jun;56(3):505–513.
National Newborn Screening by State: http://genes-r-us.uthscsa.edu/sites/genes-r-us/files/nbsdisorders.pdf. Accessed March 16, 2013.
Lead Screening
The developing infant and child are at risk of lead poisoning or toxicity because of their propensity to place objects in the mouth and their efficient absorption of this metal. Children with lead toxicity are typically asymptomatic. High blood levels (> 70 mcg/dL) can cause severe health problems such as seizures and coma. Numerous neuropsychological deficits have been associated with increased lead levels. Blood lead levels less than 10 mcg/dL have been correlated with lower intelligence quotients. The primary source of lead exposure in this country remains lead-based paint, even though most of its uses have been banned since 1977. Lead levels have declined nationally from a mean of 16 mcg/dL in 1976 to 2 mcg/dL in 2001. However, considerable variation in lead levels exists in different regions of the United States, and a majority of children at risk of lead toxicity are not currently screened. Despite the wide variation in the prevalence of lead toxicity, the CDC recommends universal lead screening for children at ages 1 and 2 and targeted screening for older children living in communities with a high percentage of old housing (> 27% of houses built before 1950) or a high percentage of children with elevated blood lead levels (> 12% of children with levels > 10 mcg/dL). Previously, all Medicaid-enrolled children were screened, but now the recommendation is to screen those at risk because of local variations in lead exposure.
Communities with inadequate data regarding local blood lead levels should also undergo universal screening. Caregivers of children between 6 months and 6 years of age may be interviewed by questionnaire about environmental risk factors for lead exposure (Table 9–4), although the data to support the use of this screening are inconclusive. If risk factors are present, a blood lead level should be obtained. A venous blood sample is preferred over a capillary specimen. An elevated capillary (fingerstick) blood sample should always be confirmed by a venous sample. CDC now states that reference level of 5 mcg/dL should be used to identify children with blood lead levels that are much higher than most levels in children. This new recommendation is based on the US children ages 1–5 years who are in the highest 2.5% of children when tested for lead in their blood.
The cognitive development of children with confirmed high blood levels should be evaluated and attempts made to identify the environmental source. Iron deficiency should be treated if present. Chelation of lead is indicated for levels of 45 mcg/dL and higher and is urgently required for levels above 70 mcg/dL. All families should receive education to decrease the risk of lead exposure. With any elevated lead level (> 5 mcg/dL), rescreening should be performed at recommended intervals.
American Academy of Pediatrics 2006:678. American Academy of Pediatrics Committee on Environmental Health. Lead exposure in children: prevention, detection, and management. Pediatrics 2005;116(4):1036–1046 [PMID: 16199720].
Centers for Disease Control and Prevention Lead: http://www.cdc.gov/nceh/lead/ACCLPP/blood_lead_levels.htm.
Lead fact sheet (English and Spanish): http://www.cdc.gov/nceh/
lead/ACCLPP/Lead_Levels_in_Children_Fact_Sheet.pdf.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




