Fig. 13.1
a A clinical photograph of a newborn with left testiculat torsion. Note the swelling and discoloration of the scrotum. b, An intraoperative photograph of a newborn with left testicular torsion. Note the extravaginal type of torsion
◦ This type occurs exclusively in newborns.
◦ Extravaginal torsion constitutes approximately 5 % of all torsions and of these cases of testicular torsion, 70 % occur prenatally and 30 % occur postnatally.
◦ Neonates with extravaginal torsion present with scrotal swelling, discoloration, and a firm, painless mass in the scrotum (Fig. 13.1b).
◦ It is commonly unilateral but can present bilaterally (Fig. 13.2a).
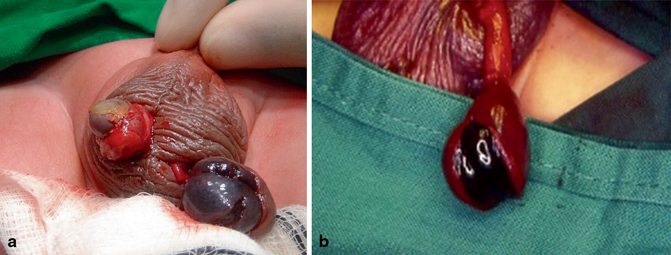
Fig. 13.2
Intraoperative photograph of a newborn with bilateral testicular torsion (a) and an intraoperative photograph of a newborn with testicular torsion (b). Note the already necrotic testis
◦ Such testes are usually necrotic from birth and must be removed surgically (Fig. 13.2b).
◦ It is also believed that torsion occurring during fetal development can lead to the vanishing testis, and is one of the causes of an infant being born with monorchism.
◦ The fact that 30 % of these cases occur postnatally calls for early surgical exploration.
Intravaginal torsion:
◦ Torsion occurring within the tunica vaginalis.
◦ The peak incidence of intravaginal torsion occurs at age 13–14 years.
◦ The left testis is more frequently involved.
◦ Bilateral cases account for 2 % of all torsions.
Clinical features :
Testicular torsion usually presents with an acute onset of diffuse testicular pain and tenderness. There is a rapid onset of testicular pain.
The age of the patient may be helpful as torsion of the appendix testis is more common in prepubertal boys (Table 13.1).
Table 13.1
Differential diagnosis and management of the acute scrotum
Type
Onset of symptoms
Age at diagnosis
Site of tenderness
Urinalysis
Cremasteric reflex
Treatment
Testicular torsion
Acute
Early puberty
Diffuse
Negative
Negative
Surgical exploration
Appendiceal torsion
Subacute
Prepubertal
Localized to upper pole
Negative
Positive
Bed rest and scrotal elevation
Epididymitis
Insidious
Adolescence
Epididymal
Positive or negative
Positive
Antibiotics
Nausea is common and usually afebrile but may have a low-grade fever.
The scrotum is generally neither swollen nor discolored, and the affected testis may have a horizontal lie.
Prehn’s sign: The physical lifting of the testicles relieves the pain of epididymitis but not pain caused by testicular torsion. This was once believed to be helpful in determining whether the presenting testicular pain is caused by acute epididymitis or from testicular torsion but it is not reliable.
The cremasteric reflex is generally absent in cases of testicular torsion.
Many of the symptoms of testicular torsion are similar to epididymitis though epididymitis is usually characterized by discoloration and swelling of the testis, often with fever, and the cremasteric reflex is not affected.
Diagnosis :
The diagnosis of testicular torsion is often made clinically.
Emergency diagnosis and treatment are usually necessary within 4–6 hours from the onset of symptoms in order to prevent necrosis.
The most widely used imaging modality for evaluation of testicular torsion is ultrasonography with Doppler scanning for blood flow (Fig. 13.3).
Fig. 13.3
An algorithm of the diagnosis and management of acute scrotum
In general, a Doppler ultrasound should be obtained only in low-suspicion cases to rule out torsion while in those cases with a convincing history and physical examination immediate surgical detorsion is the treatment of choice.
A Doppler ultrasound scan is nearly 100 % accurate at diagnosing torsion. There is absence of blood flow in the twisted testicle, which distinguishes the condition from epididymitis.
Radionuclide scanning (technetium-99 m pertechnetate) of the scrotum:
This is the most accurate imaging technique to diagnose testicular torsion.
It is however not widely available, and even in centers with functioning nuclear medicine facilities, they may not have these available at all hours.
Radioisotope scanning has been reported to be highly accurate for the diagnosis of testicular torsion.
The ischemic area is seen as a photopenic zone in testicular ischemia.
In cases of inflammation and infection, increased uptake is seen.
Treatment
The two most important determinants of early salvage rate of the testis are:
The time between onset of symptoms and detorsion
The degree of twisting of the cord thus, time is of the essence
Time should not be wasted attempting to arrange for imaging studies, laboratory testing, or other diagnostic procedures as this results in lost testicular tissue.
Salvage rate depends on the time between onset of symptoms and detorsion:
Between 90 and 100 %, if detorsion is done within 6 h of onset of symptoms.
Between 20 and 40 % after 12 h.
From 0 to 10 % if > 24 h.
Testicular torsion classically develops as a medial rotation; however, in up to one-third of cases, a lateral rotation has been described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


