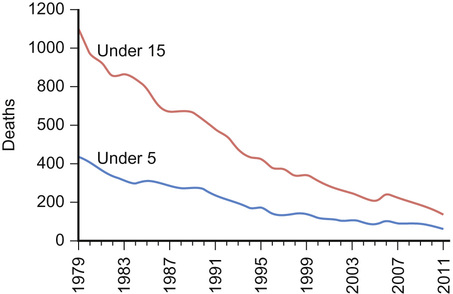
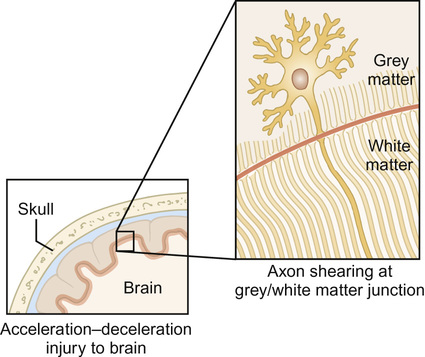
Mark Anderson, Eleanor Dawson Traumatic injury is the leading cause of death in children and young people aged 1–19 years. For every child who dies as the result of an accident, a significantly greater number are hospitalized, a proportion of whom will acquire permanent disability or disfigurement. In England and Wales, the mortality rate due to accidents has fallen markedly over the last 20 years (Fig. 7.1). This has resulted in more children aged 1–14 years now dying from malignant disease than injury. However, in 2011, 143 children died from an unintentional injury and 68 of these were under five years of age. The rate of admission to hospital of children and young people aged 0–17 years in England due to unintentional and deliberate injuries remains steady at about 120 per 10,000 population. Worldwide, injuries are a leading cause of death and disability in children and young people, with much higher mortality rates in low- and middle-income countries (Table 7.1), with road traffic injuries and drowning featuring very commonly. Accidents are particularly common in children and young people: Anatomical and physiological differences between young children and adolescents influence the pattern of injuries seen and have implications for the assessment and management of injured children and young people: Road traffic collisions (RTCs) account for the highest number of accidental deaths in children. Child pedestrians are the most vulnerable individuals in RTCs, followed by cyclists and then vehicle passengers. Most accidents occur in built-up areas rather than higher speed dual carriageways and motorways. Over 2000 children were killed or seriously injured as a result of road accidents in the UK in 2012. Burns and scalds, drownings, falls and poisonings complete the top five causes of childhood accidental deaths. Accident prevention is a major public health issue. The variety of causes and multitude of factors involved in accident causation render a blanket approach to their prevention ineffective. Small targeted strategies and campaigns, which can be scaled up once efficacy has been proven, are likely to be successful. There are three main strategies to accident prevention: Box 7.1 lists some specific examples of successful accident prevention strategies. Head injury is the commonest cause of death in injured children. Severity of the injury is therefore the principal determinant of outcome in multisystem trauma. In young children, falls are the commonest cause of severe injury, whereas in the older age groups, road traffic collisions, particularly from cycle accidents, are more common. Non-accidental (inflicted) head injury must be considered in infants. Damage to the central nervous system (CNS) as a result of head injury can be divided into primary and secondary causes (Table 7.2). Table 7.2 Examples of causes of primary and secondary injury This is sustained as a direct consequence of the impact, causing disruption of the intracranial contents, including neuronal injury, such as diffuse axonal injury and vascular trauma. Diffuse axonal injury (DAI) is one of the most serious forms of primary neuronal injury and is associated with high mortality and neurodisability. It results in widespread injury in the brain, not in just one specific area, and occurs as a result of traumatic shearing forces due to rapid acceleration, deceleration and/or rotation of the brain (Fig. 7.2). As the brain moves rapidly backwards and forwards within the skull, the axons are disrupted, particularly at the grey–white matter junction. The clinical manifestations of this will depend on the site and severity of axonal damage, but loss of consciousness is a predominant feature. DAI is typically not demonstrated by computerized tomography (CT) but requires magnetic resonance imaging (MRI). The force of impact may cause injury to intracranial blood vessels, leading to bleeding within the skull. Traumatic extra-axial bleeds (those occurring outwith the brain) are usually extradural and subdural haematomas. In extradural haematomas, blood accumulates between the dura mater and the skull. This type of bleed is usually due to arterial breach, particularly of the middle meningeal artery, and as such, develops rapidly. Subdural haematomas involve bleeding between the dura mater and the arachnoid mater and, in contrast to extradural haematomas, are usually venous in origin, so develop at a slower pace. Bridging veins in the dural regions are the most common source of bleeding. Both types of haematomas can cause raised intracranial pressure as the bleed enlarges, causing mass effect and compression of the brain tissue. Subdural haematomas can also be seen in non-accidental head injury. An incidental finding of these or a finding inconsistent with the history given, should raise suspicion and consideration of non-accidental injury. Traumatic subarachnoid haemorrhages can also occur and usually develop in close proximity to cerebral contusions or skull fractures. Secondary injury is further damage to the brain that can occur minutes to days after the original injury. It is often either preventable or treatable, and failure to minimize its effects results in a poorer overall outcome. Patients with significant traumatic brain injury need extremely close monitoring, especially in the initial period after injury, with the main aim of early management being the prevention and treatment of complications which may give rise to secondary injury. Despite the seriousness of paediatric head trauma, the vast majority of head injuries in children are mild. Determining which children require neuroimaging is difficult. Various criteria, related to both the history and examination, are used to try to predict the likelihood of intracranial pathology. The current recommendations from the National Institute for Health and Care Excellence (NICE) are found in Box 7.2. These criteria display excellent sensitivity but poor specificity and result in a significant number of normal scans. The aim of resuscitation of the child with severe head injury is to maximize cerebral perfusion while minimizing the effect of raised intracranial pressure. This is described in Chapter 6, Paediatric emergencies and critical care. Although children sustaining a severe traumatic brain injury are likely to have a very long period of recovery, with intensive rehabilitation therapy they can make good progress and recover some function. Cognitive, behavioural and psychiatric problems are the most common long-term sequelae. Cognitive problems result in difficulty with memory, learning and language, while behavioural and psychiatric complications include personality changes, lack of inhibition and depression. These outcomes vary according to the severity of the injury, the age of the child and the pre-morbid condition. Spinal cord injury is rare in the paediatric age group, occurring most commonly as the result of road traffic collisions. The most common cervical fracture involves the first two vertebrae. In addition, spinal cord injury without radiologic abnormality (SCIWORA) is almost exclusively a paediatric problem. This occurs as a result of the elasticity of the cervical spine allowing significant cord injury in absence of X-ray changes. The most common causes of thoracic injury in children are road accidents and falls. Chest injuries are mostly caused by blunt trauma with only a very few due to penetrating injury, and usually occur in conjunction with trauma to other body parts. The chest wall of children is much more compliant than adults, leading to transfer of impact energy to underlying organs and structures with minimal, if any, external sign of injury or fracture. The presence of rib fractures or mediastinal injury indicates very significant and high energy impact. Common underlying injuries include lung contusions, which develop as energy is transferred rapidly to the lungs causing haemorrhage and oedema in the lung tissue, and pneumothoraces. Great vessel trauma is very rare. Children are more vulnerable to major abdominal injuries as a result of pliable rib cages, which provide little protection to solid organs, which are proportionally larger than in adults. In addition, their abdominal wall is thin and provides less impact absorption. Most abdominal injuries are caused by blunt trauma, often due to road traffic collisions, seat belt restraint and handlebar injury. The pancreas is particularly at risk from handlebar injury. Intra-abdominal organs bleed readily, resulting in hypovolaemia and circulatory collapse. Acceleration and deceleration forces cause injury to organs, which are moved rapidly and may come into contact with the spine. Abdominal injury can be life-threatening and difficult to diagnose quickly in the absence of external signs. Injury to organs such as the spleen and liver manifest themselves rapidly, while bowel or pancreatic injuries may not become clinically evident for several days. A proactive approach to identifying abdominal injury is needed, especially in high mechanism injuries. Although focused abdominal sonography for trauma (FAST) is a useful tool, it can miss major solid organ injury and it must be combined with clinical judgement. Burns are injuries to tissues usually caused by heat, but also by friction, electricity, radiation (from the sun, for example) or chemicals. Scalds are caused by contact with hot liquid or steam. They are among the most common of childhood accidents. The vast majority of childhood burns and scalds occur within the home. Children in low- and middle-income countries are most at risk from fatal burn injuries. Cooking on an open fire is a major risk factor and children with underlying medical conditions, such as epilepsy, are at particular risk when near fires. In high-income countries such as the UK, children in lower socio-economic groups are at increased risk. The severity of burns and scalds is determined by two main factors – the length of contact and the temperature: Burns are classified according to the depth and severity of the tissue damage and extent of body surface area. Previously, burns were described as first, second or third degree, but this has been replaced with the classification shown in Table 7.3. Table 7.3 Burn classification Burn injuries produce both local and systemic reactions. In small burns, the body’s response is localized to the site of the burn. In larger burns affecting over 30% of the total body surface area, and also in deeper dermal burns, a systemic inflammatory response is seen with inflammatory mediators such as cytokines, prostaglandins, histamine and complement being released into the circulation. Capillary leak increases, leading to oedema in the soft tissues and intravascular fluid depletion. Hypovolaemia then results in hypoperfusion. Myocardial contractility can be reduced by the presence of tumour necrosis factor alpha. Intra-abdominal vasoconstriction occurs, potentially compromising blood flow to organs such as the spleen, kidneys and bowel. Fluid, including electrolytes, is also lost through evaporation from the burn itself and all these changes combine to produce systemic hypotension and end organ hypoperfusion. Catabolism is marked after major burns and early nutritional input is necessary to aid recovery. Infection risk is increased significantly due to direct entry of micro-organisms through the damaged area and because the local immune response is compromised. As intravascular fluid depletion is a major complication of burns, adequate fluid resuscitation is important. Shock in burn is the result of a combination of factors, including hypovolaemia, microcirculatory injury and the release of local and systemic inflammatory mediators. The foundation of early burn management is the treatment and prevention of shock with intravenous fluid resuscitation. The heterogeneous nature of children with burns, in terms of their varying size and burn area, has led to the exploration of a number of formulae to guide fluid resuscitation. The most widely accepted version is the Parkland formula: 50% of this volume is administered over the first 8 hours with the remainder administered over the subsequent 16 hours. This mimics the physiological situation as plasma losses are greatest in the first 6–8 hours after a burn with ongoing slower capillary leakage thereafter. As a corollary, the 24-hour period therefore begins from the time of the burn, not the time of initiation of fluid resuscitation. The recommended fluid is crystalloid and, in general, Hartmann’s solution is used as this has the closest electrolyte composition to plasma. Maintenance fluid requirements should be administered in addition to these volumes. The Parkland formula, and others like it, provide only a guide to fluid requirements and clinical response is the final arbiter of adequacy of fluid resuscitation. In particular, maintenance of urine output of 1.0 mL/kg/hour is generally accepted as evidence of euvolaemia in patients with burns. Adequate analgesia is an essential element of the acute and ongoing management of burns with intravenous opiates often required for most significant burn injuries. It is generally accepted that burns involving more than 5–7% of the body surface area and certain other burns should be cared for in a specialist burns unit (where possible) (Box 7.3), as these burns are more likely to require surgical input (e.g. skin grafting) and/or specialist monitoring of longer term complications (e.g. contractures). The management of respiratory complications of burns sustained as a result of house fires is relatively common. Inhalation injury is the commonest cause of death in burns patients from smoke inhalation, and in combination with cutaneous burns has a mortality of 30–90%. Upper airway injury resulting in obstruction in the first 12 hours after exposure is caused by direct thermal injury as well as chemical irritation. Lung parenchymal injury associated with inhalation, by contrast, is not a result of direct thermal injury – only inhaled steam, which has a heat-carrying capacity significantly greater than dry air, is capable of overcoming the heat dissipation mechanisms of the upper airways. Damage to the distal airways is caused by the incomplete products of combustion, in particular aldehydes, nitrogen and sulphur oxides, and carbon monoxide. Whilst inhalation injury mostly results in proximal airway damage and oedema, it also inactivates surfactant leading to reduced pulmonary compliance and in severe cases to adult respiratory distress syndrome (ARDS).
Accidents and poisoning
Accidents
Trauma
Head injury
Primary
Secondary
Extradural haemorrhage
Cerebral oedema
Subdural haemorrhage
Infection
Subarachnoid haemorrhage
Hypoxia
Cerebral contusion/laceration
Hypotension
Axonal stretching/shearing
Seizures
Primary injury
Secondary injury
Management
Mild head injury
Severe brain injury
Outcome
Spinal cord injury
Thoracic injury
Abdominal injury
Burns and scalds
Risk factors
Pathophysiology
Type of burn
Description
Superficial – simple erythema
Painful, reversible redness of the skin, such as in milder cases of sunburn. Only affects the epidermis so there is no blistering of the skin. Takes several days to heal and may result in peeling over the following days.
Superficial – partial thickness
Involves only the upper layers of the skin (epidermis and into the dermis) and usually heals within two weeks with minimal or no scarring. It appears as erythema with blistering and is painful.
Deep – partial thickness
Extends into the deeper layers of the dermis. The burn will be more yellow or white in colour and there may be blistering. These burns may require surgery such as skin grafting to aid healing. Without surgery, they will usually be associated with delayed healing and risk of significant scarring.
Full thickness
Involves all layers of skin and extends through the entire dermis. As the nerve endings have been fully damaged, these burns are painless and white or brown in colour. Healing takes many months and there is a high risk of complications such as contractures if the burn occurs across a joint. Surgery is usually indicated.
Inhalation injury
Carbon monoxide poisoning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Accidents and poisoning
Chapter 7
Learning objectives
By the end of this chapter the reader should: