Abnormal Pubertal Development
Dennis M. Styne and Leonna Cuttler
SEXUAL PRECOCITY AND EARLY PUBERTY
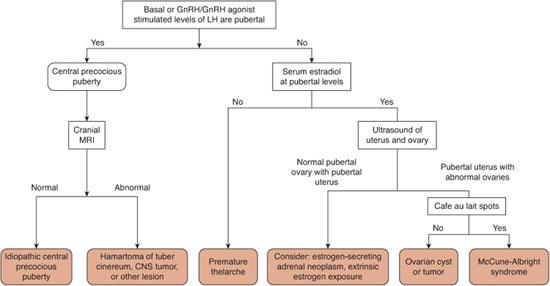
Sexual precocity is the general term for early puberty. Isosexual precocity refers to a girl who feminizes or a boy who virilizes early. Central precocious puberty or true precocious puberty is a term reserved for children with gonadotropin-releasing hormone (GnRH)-dependent early puberty that follows the normal pubertal pattern and the normal control mechanisms through GnRH. The only difference from normal puberty is the earlier age at onset. Central precocious puberty can be idiopathic or caused by organic conditions such as a brain tumor or a hamartoma of the tuber cinereum. GnRH-independent isosexual precocity is caused by excessive estrogen secretion in girls or androgen secretion in boys from sources other than the GnRH-gonadotropin axis (such as the gonads, the adrenal glands, ectopic human chorionic gonadotropin (hCG) secretion, and exogenous sources of sex steroids). Gonadotropins are suppressed by negative feedback in all forms of GnRH-independent isosexual precocity because sex steroid secretion is autonomous. Contrasexual (or heterosexual) precocity refers to girls who virilize and boys who feminize.
Onset of puberty among Caucasian girls as early as 7 years of age or among African American girls as early as 6 years of age can be considered normal if there are no neurologic symptoms or signs of increased intracranial pressure, if there is not a rapid advancement in pubertal development or bone age, and if menses is after at least age 9 years. If there is a family history of a pattern of early pubertal development, the child is even more likely to have a variant of normal puberty rather than a pathologic condition causing sexual precocity. Among boys the earliest limit of normal puberty is 9 years of age. Onset earlier than these limits is considered sexual precocity.1 The classification schema and causes of precocious puberty are outlined in Table 541-1.
All children with sexual precocity show the effects of increased sex steroids such as secondary sexual characteristics, excessive growth for chronologic age, and rapid bone age advancement. Although some children progress rapidly through precocious puberty, some follow a waxing and waning course. The more severely affected children have tall stature and a bone age that advances faster than height velocity. If untreated, these patients achieve a severely decreased adult height because of premature epiphyseal closure. Historically, girls not treated for sexual precocity reached a mean adult height of 151 to 152 cm compared with a mean adult height in the United States of 164 cm. Boys not treated for sexual precocity reached an adult height of 161 cm compared with an average adult height in the United States of 178 cm.
Some children start puberty somewhat early compared with current standards but not strikingly so and may be manifesting a family tendency toward early puberty. The milder cases (ie, without marked advancement of bone age, without marked elevation of the serum level of IGF-I, and among girls, without marked elevation of the serum level of estrogen) may not need treatment and still achieve an acceptable adult height as may those with unsustained precocious puberty that may wax and wane over a period of time. In both situations, there should be careful follow-up, as slowly progressive puberty can convert to rapidly progressive true precocious puberty. The psychological stress of early sexual development and menarche among girls can influence a parental decision toward therapy. While boys may exhibit hyperactivity or aggression and masturbation due to early puberty, girls do not necessarily change their behavior.
Table 541-1. Causes and Classification of Sexual Precocity
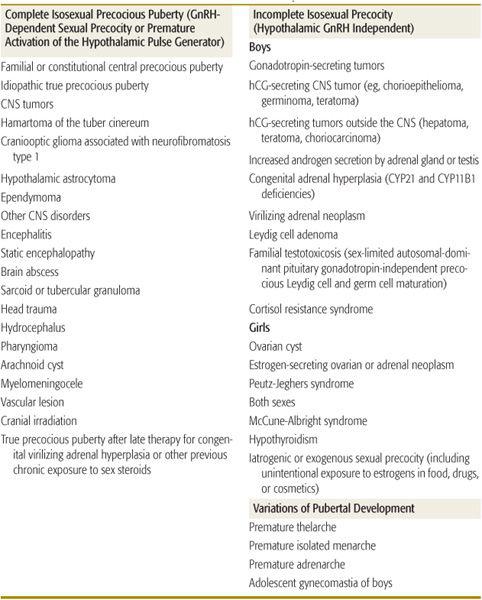
CNS, central nervous sytem; GnRH, gonadotropin-releasing hormone; hCG, human chorionic gonadotropin.
Copyright © 2002 by The McGraw-Hill Companies, Inc. All rights reserved.
 TRUE CENTRAL PRECOCIOUS PUBERTY (GNRH DEPENDENT)
TRUE CENTRAL PRECOCIOUS PUBERTY (GNRH DEPENDENT)
True central precocious puberty results from an increase in GnRH secretion at a younger age than normal. Most cases are idiopathic, but because organic causes include brain tumors, further evaluation is usually indicated. Precocious puberty occurs more frequently among girls than among boys, but central nervous system tumor as a cause of precocious puberty is more common among boys than among girls.
Signs of central precocious puberty in boys include the development of secondary sexual characteristics, and an increase in testicular diameter to greater than 2.5 cm in longest measurement or a volume greater than 4 mL. Girls with precocious puberty have an increased growth rate even before development of the breasts, but the breast development is more easily detected. Breast development is noticed among girls with all types of isosexual precocity, but true menarche occurs only in GnRH-dependent precocious puberty. Fertility can be achieved early in children with central precocious puberty. There is a report of a 6-year-old girl delivering a child by Caesarian section due to the combination of precocious puberty and sexual abuse, emphasizing the importance of ensuring the safety of girls with early puberty.
Central Nervous System Causes of Precocious Puberty
The most common central nervous system (CNS) abnormality causing central precocious puberty is hamartoma of the tuber cinereum.2 These nonmalignant congenital masses of heterotopic tissue, composed of GnRH-synthesizing neurons, are derived from the embryonic hypothalamus and escape regulation by the central nervous system, so they cause pulsatile secretion of gonadotropins with stimulation of the gonads during childhood. They do not grow so that they are not associated with a mass effect, but they can be associated with gelastic or laughing seizures, petit mal seizures, or grand mal seizures. Hamartoma of the tuber cinereum has a characteristic appearance on magnetic resonance (MR) images of a sessile or pedunculated mass attached to the posterior hypothalamus between the tuber cinereum and the mamillary bodies projecting into the suprasellar cistern.3 Biopsy is not needed for diagnosis due to the classic radiographic findings. Surgical management is not usually indicated, as the lesion is responsive to GnRH agonists as discussed below. However, if seizures are not responsive to treatment, surgery may be necessary.
Craniopharyngioma, astrocytoma, ependymoma, and optic or hypothalamic glioma and ependymoma all interfere with the normal juvenile pause and can cause central precocious puberty, as can optic glioma or neurofibroma in the hypothalamic area associated with neurofibromatosis type 1 (von Recklinghausen disease). These tumors can cause other symptoms, such as headache, abnormalities of vision, optic atrophy, and diabetes insipidus.
Central nervous system radiation therapy may also cause central precocious puberty even if the treated tumor does not cause precocious puberty. When radiation causes central precocious puberty, the resultant growth acceleration can mask radiation-induced growth hormone (GH) deficiency (see Chapter 521). When both occur, treatment with combined GH and GnRH agonist is necessary to achieve more normal adult height.
High intracranial pressure caused by hydrocephalus or a subarachnoid cyst can cause precocious puberty, which is reversed solely by means of release of the elevated intracranial pressure. Fetal or childhood central nervous system infections of any type, such as tuberculosis and brain abscess, can cause precocious puberty, as can cerebral vascular accidents and central nervous system trauma. Developmental delay of various causes, including static cerebral encephalopathy, can cause precocious adrenarche (see below) or complete central precocious puberty. Congenital defects of the central nervous system such as septooptic dysplasia may cause central precocious puberty.
Those who have no hamartoma or other definable cause of central precocious puberty have idiopathic precocious puberty.
Androgen Exposure
Exposure to high serum concentrations of androgens, as seen with virilizing congenital adrenal hyperplasia, causes early maturation of the hypothalamus with central precocious puberty even after the primary cause of increased androgens is treated, and the androgen levels have reverted to normal levels. Often children diagnosed with congenital adrenal hyperplasia require treatment with a GnRH agonist, in addition to the standard treatment of glucocorticoid and mineralocorticoid, to prevent early puberty. Likewise, children with androgen-secreting tumors that are removed after years of virilization can subsequently have central true precocious puberty.
Children Adopted from Developing Countries
Girls adopted into Western families after an infancy in the Third World may develop central precocious puberty.4 This is postulated to be linked to early malnutrition followed by normal or excessive nutrition with both effects tending to advance the age of puberty.
 GNRH-INDEPENDENT SEXUAL PRECOCITY (INCOMPLETE ISOSEXUAL PRECOCITY)
GNRH-INDEPENDENT SEXUAL PRECOCITY (INCOMPLETE ISOSEXUAL PRECOCITY)
Sexual precocity occurring in the absence of an increase in GnRH is caused by either autonomous secretion of sex steroids in both sexes or, among boys, to production of hCG, which stimulates testicular testosterone secretion. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are suppressed to nondetectable concentrations in the face of elevated (often extremely elevated) sex steroid concentrations. Agonists of GnRH have no effect on these conditions, although as noted above, exposure to sex steroids may stimulate early hypothalamic maturation that persists following treatment for the virilizing condition.
Causes of GnRH-Independent Sexual Precocity among Boys
Germ cell tumors secrete hCG, which in high concentrations stimulates the Leydig cells to produce testosterone. Human chorionic gonadotropin does not stimulate the seminiferous tubules, so these boys have only slight enlargement of the testes (to a degree far less than occurs in central precocious or normal puberty). The penis enlarges; the serum hCG concentration is elevated, but levels of FSH and LH are not. (It is essential to use assays that can differentiate hCG from LH, usually a beta-hCG assay.) The lesion responsible can be teratoma, chorioepithelioma, dysgerminoma, or a mixed germ cell tumor, which can be located in the hypothalamus, the mediastinum, the lungs, the gonads, or the retroperitoneal cavity. Hepatoblastoma also can be causative. The tumors may secrete -feto protein as well as hCG. Boys with 47,XXY Klinefelter syndrome have an increased incidence of hCG-secreting mediastinal germ cell neoplasms.5
Virilizing congenital adrenal hyperplasia can be caused by 21-hydroxylase deficiency, which can be associated with the salt-loss of mineralocorticoid deficiency, or can be caused by 11β-hydroxylase deficiency, which can be accompanied by hypertension because of excess mineralocorticoid secretion. In boys, these conditions cause virilization without testicular enlargement, because the androgen originates from the adrenal glands. Because gonadotro-pins are suppressed, the testes can be small for age or small for the degree of virilization. The classical form manifests during infancy as salt loss and normal genital appearance. Without salt loss, the condition can manifest as GnRH-independent isosexual precocity in boys later in infancy (see Chapter 533). Virilizing adenoma and carcinoma of the adrenal gland secrete large amounts of dehydroepiandrosterone (DHEA) (and dehydroepiandrosterone sulfate [DHEAS]), which is peripherally converted to more potent androgens. When the adrenal gland is the cause of the virilization, the testes remain prepubertal in size. Leydig cell tumors are rare among boys but manifest as asymmetrically enlarged testis or testes.
Familial gonadotropin-independent sexual precocity with premature Leydig and germ cell maturation (or “testotoxicosis”) is a rare, sex-limited dominant condition that manifests clinically only among boys.1 It is due to an activating mutation in the luteinizing hormone receptor, rendering it constitutionally activated, so that it constantly stimulates testosterone production. Affected boys have enlargement of the penis and virilization but only minimal enlargement of the testes because there is predominant stimulation of Leydig cells and relatively less enlargement of the seminiferous tubules. The boy grows rapidly, but adult height is markedly decreased; affected girls are normal. Fertility is normal at adulthood. These patients have elevated testosterone levels with low gonadotropin concentrations. Spironolactone, an antimineralocorticoid and antiandrogen agent used to limit androgen effect, has been combined with testolactone, an inhibitor of aromatase that limits bone age advancement, as treatment for these boys. An alternative is cyproterone acetate, a powerful antiandrogen that blocks the androgen receptor, can be used alone. Ketoconazole, an inhibitor of steroidogenesis, has also been employed effectively in males with testotoxicosis. Later in life, central precocious puberty often develops, and these patients become responsive to GnRH, although they were not responsive in childhood. This phenomenon appears similar to the hypothalamic-pituitary-gonadal maturation that occurs among patients with premature puberty after therapy for other virilizing disorders and is responsive to a GnRH agonist.
Familial cortisol resistance syndrome leads to a compensatory increase in corticotropin (ACTH) secretion which increases glucocorticoid secretion; because there is resistance to glucocorticoids, there is no manifestation of excess glucocorticoid effect in spite of elevated circulating glucocorticoids.7 However, because there is an increase in ACTH, adrenal androgen secretion rises causing premature adrenarche and virilization as well as hypertension and hypokalemia due to increased mineralocorticoid secretion. Occasionally, testosterone topically applied by the father may be transferred to his young son resulting in virilization of the child.
Causes of GnRH-Independent Sexual Precocity among Girls
Gonadotropin-independent isosexual precocity among girls can be caused by ovarian cysts or neoplasms, exposure to exogenous estrogens, or abnormalities of the adrenal glands. Prepubertal girls normally have small ovarian cysts, but some cysts enlarge and secrete sufficient estrogen to cause breast development and even withdrawal bleeding.8 The estrogen levels are usually only at pubertal values, but occasionally very high levels, characteristic of tumors, are encountered. Most cysts do not recur, but repetitive cyst formation can occur. Affected girls secreted more FSH than normal prepubertal girls which may explain the pathogenesis of this condition.
Several neoplasms can cause gonadotropin-independent isosexual precocity among girls. Granulosa cell tumors of the ovary are rare, being discovered by bimanual examination in 80% of cases.9 Antimüllerian hormone and inhibin are useful tumor markers for postoperative follow-up evaluation of these tumors. Gonadoblastomas can arise in streak gonads and secrete estrogen or even testosterone. These tumors are benign but can harbor malignant ovarian tumors. Estrogen-secreting adrenal neoplasms are infrequent compared with those that secrete androgens. Tumors that secrete human chorionic gonadotropin (hCG) cause no physical pubertal changes in girls due to endocrine effects alone. Girls and boys can be exposed to estrogens through ingestion of their mothers’ oral contraceptives or contact with estrogen-containing ointment; lavender oil and tea tree oil contain estrogen and exert these effects. Feminization also has been attributed to estrogen contamination of milk, meat, or even vitamins prepared on machinery previously used to package estrogen.
Causes of GnRH-Independent Sexual Precocity among Boys and Girls
McCune-Albright syndrome is a disorder including irregular café-au-lait spots (“Coast of California pattern”), polyostotic fibrous dysplasia (cysts in the long bones and thickening of the skull), and autonomous endocrine function, usually manifesting as GnRH-independent sexual precocity. Patients may have autonomous hyperactivity of the somatotropes (acromegaly or gigantism), thyroid cells (thyrotoxicosis), parathyroid glands, or adrenal glands (Cushing syndrome). The widespread endocrine activity is caused by activating mutations of the stimulatory G-protein subunit of the adenyl cyclase system attached to the membrane receptor of the affected cells. Because these are somatic cell mutations that are not in the germline, the disease affects some organs while skipping others, leading to the variable manifestations.
This syndrome is most common among girls but can affect boys. The skin and skeletal manifestations develop after birth. The sexual precocity of the McCune-Albright syndrome is initially autonomous, but exposure to the endogenous estrogens or androgens eventually can mature the hypothalamic-pituitary-gonadal axis and cause GnRH-dependent precocious puberty. Therapy in girls typically includes the use of an antiestrogen, and treatment options in boys include an antiandrogen in combination with an aromatase inhibitor.10,11 Agonists of GnRH have been effective later in childhood in managing secondary central precocious puberty, which occurs after maturation of the hypothalamic-pituitary-gonadal axis.
Severe, uncontrolled hypothyroidism can be associated with incomplete sexual precocity of both boys and girls. The extremely high levels of TSH caused by hypothyroidism can stimulate gonadotropin receptors (hormonal overlap syndrome). Plasma level of prolactin is elevated, and galactorrhea can occur, especially among girls. Growth is impaired as for any child with hypothyroidism, so there is no pubertal growth spurt. Girls may have breast development, menstrual flow, and estrogen effects on the vaginal mucosa. In boys, the size of the testes may increase because of enlargement of the seminiferous tubules. The pituitary gland may enlarge and erode the sella turcica in a manner incorrectly suggesting a tumor because of increased TSH secretion and thyrotroph hyperplasia. Once hypothyroidism is controlled, sexual precocity reverts and the sella turcica becomes smaller.
Peutz-Jeghers syndrome is an autosomal dominant condition characterized by nasal polyps, hyperpigmentation of the lips, and macules of the buccal mucosa; affected boys can have gynecomastia and precocious puberty with Sertoli cell tumors, and girls can develop ovarian cysts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


