KEY POINTS
• Dystocia results from abnormalities during labor with the interplay between the power (uterine contractions and maternal expulsive forces), the passenger (fetal size, presentation, and position), and the passage (maternal bony pelvis and soft tissues).
• Recognition of risk factors and causes of dystocia are critical for proper treatment.
• Appropriate management of dystocia reduces maternal and fetal morbidity and prevents unnecessary cesarean deliveries (CD).
BACKGROUND
Definitions
• Dystocia: difficult labor and childbirth.
• Prolonged latent phase (Table 10-1; Fig. 10-1)
• Nulliparous patient: greater than 20 hours
• Multiparous patient: greater than 14 hours
• It is often difficult to determine the start of the latent phase because of increased uterine activity (“false labor”) that may occur days before the onset of spontaneous labor (1).
• The latent phase is generally considered complete when cervical dilation reaches 3 to 5 cm.
• Protraction disorders—slow progression of labor (Fig. 10-2) (2,3).
• Protracted active phase dilation:
 Nulliparous patient: rate of dilation less than 1.2 cm/h
Nulliparous patient: rate of dilation less than 1.2 cm/h
 Multiparous patient: rate of dilation less than 1.5 cm/h
Multiparous patient: rate of dilation less than 1.5 cm/h
• Protracted descent—descent of fetal presenting part during second stage of labor:
 Nulliparous patient: less than 1 cm/h
Nulliparous patient: less than 1 cm/h
 Multiparous patient: less than 2 cm/h
Multiparous patient: less than 2 cm/h
• Arrest disorders—no progression of labor (Fig. 10-3) (2–4).
• Secondary arrest of dilation
 No cervical dilation after 2 hours in active labor with adequate contractions
No cervical dilation after 2 hours in active labor with adequate contractions
• Arrest of descent:
 No descent of fetal presenting part after 1 hour in the second stage of labor
No descent of fetal presenting part after 1 hour in the second stage of labor
• Prolonged second stage of labor (4–6)
• Nulliparous patient without regional analgesia: greater than 2 hours
• Nulliparous patient with regional analgesia: greater than 3 hours
• Multiparous patient without regional analgesia: greater than 1 hour
• Multiparous patient with regional analgesia: greater than 2 hours
• Precipitous labor—rapid labor (7)
• Delivery of the fetus in less than 3 hours
Table 10-1 Labor Duration
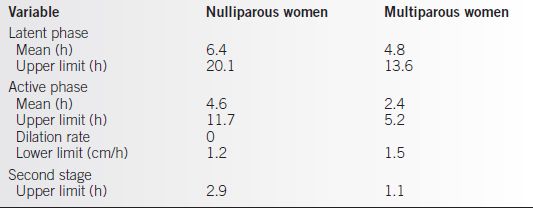
From Friedman EA. Labor: clinical evaluation and management. 2nd ed. New York: Appleton-Century-Crofts, 1978, with permission.
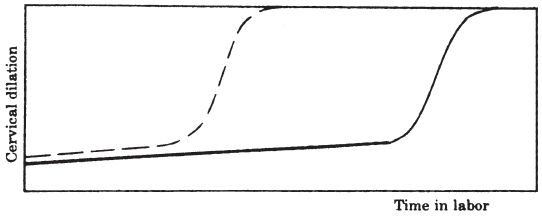
Figure 10-1. Prolonged latent phase pattern (solid line). Broken line illustrates average dilation curve for nulliparous women. (From Friedman EA. Labor: clinical evaluation and management. 2nd ed. New York: Appleton-Century-Crofts, 1978, with permission.)
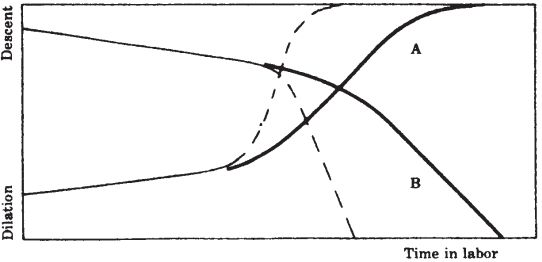
Figure 10-2. Protraction disorders of labor. A: Protracted active phase. B: Prolonged descent pattern. Broken lines illustrate average normal dilation and descent patterns. (From Friedman EA. Labor: clinical evaluation and management. 2nd ed. New York: Appleton-Century-Crofts, 1978, with permission.)
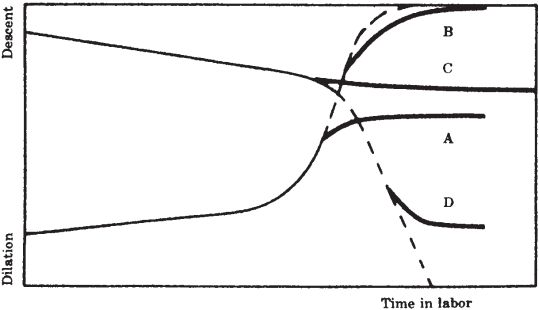
Figure 10-3. Arrest disorders of labor. A: Secondary arrest of dilation. B: Prolonged deceleration. C: Failure of descent. D: Arrest of descent. Broken lines illustrate normal dilation and descent curves. (From Friedman EA. Labor: clinical evaluation and management. 2nd ed. New York: Appleton-Century-Crofts, 1978, with permission.)
Epidemiology
• The leading indication for primary CD in the United States is dystocia or “failure to progress” (8,9).
• Approximately 50% to 60% of CD may be attributable to dystocia (9).
• Successful management of abnormal labor and adhering to the appropriate definitions of dystocia will help decrease the CD rate.
Pathophysiology
• Dystocia results from the abnormal functions and interactions between
• Uterine contractions and maternal effort: Power
• Fetal size, presentation, and position: Passenger
• Maternal bony pelvis and soft tissues: Passage
Etiology
• Associated risk factors for dystocia include (9–15):
• Advanced maternal age
• Maternal diabetes mellitus and/or hypertension
• Short maternal stature
• Maternal pelvic contractures or tumors (leiomyomas)
• Infertility or nulligravidity
• Premature rupture of membranes (PROM) or oligohydramnios
• Chorioamnionitis
• High station at complete cervical dilation
• Fetal malposition
• Prior perinatal death
• Large for gestational age (LGA)/macrosomia
• Epidural analgesia
• Physician and/or patient anxiety due to prior or current pregnancy complications can result in prematurely labeling the labor as “failure to progress.”
EVALUATION
History and Physical
• During antepartum visits:
• Obtain an accurate history to identify risk factors for dystocia.
• Perform a physical examination to assess pelvic anatomy, which may help predict pelvic outlet abnormalities.
• Perform Leopold maneuvers to help determine fetal presentation.
• During labor:
• Perform Leopold maneuvers and/or ultrasound to determine fetal presentation.
• Estimate fetal size with abdominal palpation and/or ultrasound.
• Perform physical examination to determine:
 Fetal position
Fetal position
 Progress of cervical dilation, effacement, and station
Progress of cervical dilation, effacement, and station
Diagnostic Studies
• Ultrasound evaluation is frequently used to assess
• Estimated fetal weight (EFW)
• Amniotic fluid index (AFI)
• Fetal presentation and position
• Placental location
• Uterine anomalies or pelvic tumors
• Biophysical profile (BPP)
DYSTOCIA—UTERINE FUNCTION
Diagnosis
• The clinician must first distinguish between the latent and active phases of labor before deciding on treatment.
Etiologies
• Causes of uterine dysfunction:
• Müllerian anomalies (uterine septum or didelphys)
• Pelvic tumors (leiomyomas or large ovarian tumors)
• Cervical abnormalities resulting from a loop electrosurgical excision procedure (LEEP), cold knife cone (CKC), cerclage, trauma, or other injuries
• Uterine overdistension (LGA/macrosomia, multiple gestation, polyhydramnios)
Clinical Manifestations
• Effective contractions are obvious clinically if progression of cervical dilation and effacement occurs.
• External monitoring using either palpation or a displacement transducer provides information about the frequency of uterine contractions.
• Internal monitoring using an intrauterine pressure catheter (IUPC) provides information about the frequency, duration, and intensity of uterine contractions in millimeters of mercury (mm Hg).
• Montevideo units (MVUs) equal the mean amplitude (mm Hg) of contractions multiplied by the number of contractions in 10 minutes.
• Two hundred to two hundred and fifty montevideo units are commonly used to define adequate contractions in the active phase of labor (16,17).
Treatment
Medications
• Prolonged latent phase recommendations
• Augmentation of labor (18–21):
 Oxytocin
Oxytocin
 Misoprostol
Misoprostol
• Therapeutic rest (22):
 Nubain, 10 to 15 mg intramuscularly (IM)
Nubain, 10 to 15 mg intramuscularly (IM)
 Morphine, 10 to 20 mg IM
Morphine, 10 to 20 mg IM
 Vistaril, 100 mg orally
Vistaril, 100 mg orally
• Active management of labor
• Limited to nulliparous women with (9):
 Term pregnancies
Term pregnancies
 Singleton gestations
Singleton gestations
 Cephalic presentation
Cephalic presentation
 No evidence of fetal compromise
No evidence of fetal compromise
• The Dublin or O’Driscoll protocol (23):
 Patient education on signs and symptoms of labor
Patient education on signs and symptoms of labor
 Strict admission criteria—only patients in active labor admitted
Strict admission criteria—only patients in active labor admitted
 Amniotomy within 1 hour of admission if unruptured
Amniotomy within 1 hour of admission if unruptured
 Strict criteria for recognition of abnormal labor patterns
Strict criteria for recognition of abnormal labor patterns
 Oxytocin infusion if abnormal pattern ascertained:
Oxytocin infusion if abnormal pattern ascertained:
– Six milliunits per minute to start
– Six milliunits per minute increase every 15 minutes
– Maximum of 40 milliunits per minute or seven contractions in 15 minutes or adequate progress
 Nurse/patient ratio of 1:1
Nurse/patient ratio of 1:1
 Intermittent or continuous monitoring of contractions and fetal heart tones
Intermittent or continuous monitoring of contractions and fetal heart tones
 CD if undelivered 12 hours after admission or if fetal compromise ascertained
CD if undelivered 12 hours after admission or if fetal compromise ascertained
 Protocol resulted in CD rate of 4.8%
Protocol resulted in CD rate of 4.8%
– A second trial in Ireland using the same protocol showed a doubling of the CD rate over the first trial (24).
– Lopez-Zeno et al. (25) repeated the study in the United States and reported a decrease in the CD rate, length of labor, and febrile morbidity (25).
– Frigoletto et al. (11) repeated the study and reported no decrease in CD rate but a decrease in labor length and febrile morbidity (11).
– The American College of Obstetricians and Gynecologists (ACOG) concluded that active management of labor may shorten labor but has not consistently led to a decrease in the CD rate (9).
• Protracted labor and arrest of labor
• Use O’Driscoll protocol or Seitchik protocol (26).
 Oxytocin, 5 milliunits per minute with increase every 40 minutes
Oxytocin, 5 milliunits per minute with increase every 40 minutes
 Twenty to forty minutes is needed for plasma levels of oxytocin to reach a steady state.
Twenty to forty minutes is needed for plasma levels of oxytocin to reach a steady state.
– Satin et al. (27) analyzed 1773 cases of augmented labor. Individual patient variables prevented accurate prediction of oxytocin dosage or rate needed to affect adequate labor (27).
Procedures
• Benefits
 Reduction in labor duration
Reduction in labor duration
 Reduction in abnormal 5-minute Apgar score (less than 5)
Reduction in abnormal 5-minute Apgar score (less than 5)
 Decreased need for oxytocin
Decreased need for oxytocin
 No increase in CD rate
No increase in CD rate
• Risks
 Increase in abnormal fetal heart rate patterns (without increase in CD rate)
Increase in abnormal fetal heart rate patterns (without increase in CD rate)
 Increase in febrile morbidity
Increase in febrile morbidity
Complications
• Treatment of tachysystole: (32,33)
• Decrease or stop oxytocin.
• Administer oxygen.
• Increase intravenous fluid rate (IVF).
• Administer tocolytics (β2-adrenergic agents such as terbutaline).
• Treatment of fetal heart rate abnormalities (33,34)
• Discontinue any labor stimulating agent if possible (stop oxytocin, remove prostaglandin insert).
• Administer oxygen.
• Change maternal position.
• Perform cervical exam (check for umbilical cord prolapse, rapid cervical change, or fetal descent).
• Monitor maternal blood pressure (treat hypotension if present with volume expansion and/or intravenous ephedrine).
• Assess for uterine tachysystole (treat as above).
• May perform amnioinfusion (AI) for recurrent variable decelerations.
• Perform CD if abnormality cannot be corrected.
• Occurs in approximately 1 in 2000 deliveries.
• Risk factors include prior CD, transfundal uterine surgery, obstructed labor, multiparity, and uterine overdistension.
• May occur spontaneously without risk factors.
• Clinical manifestations include abnormal fetal heart rate patterns (most common finding), loss of fetal station, abdominal pain, vaginal bleeding, cessation of uterine contractions, and signs of hemodynamic instability.
• Can be catastrophic for mother and/or fetus.
• Immediate CD should be performed once recognized.
• Water intoxication—rare side effect of oxytocin
• Postpartum hemorrhage (see Chapter 4 for management)
DYSTOCIA—FETAL FACTORS
Malpresentations
Diagnosis
Clinical Manifestations
• Asynclitism (36)
• Fetal sagittal suture is not midway between the maternal symphysis and sacral promontory (lateral deflection of the sagittal suture).
• Parietal bone is palpated as presenting structure.
• Brow presentation (Fig. 10-4) • Partially deflexed cephalic attitude (halfway between full extension and flexion)
• Diagnosed by palpation (feel brow, orbital ridges, eyes, frontal sutures, anterior fontanelle)
• Occurs in 0.2% of all deliveries
• Face presentations (Fig. 10-5)
• Fetal head is hyperextended (fetal occiput in contact with fetal back).
• Diagnosed by palpation (feel facial features).
• Reference point for description is the mentum (chin)—mentum anterior (MA) or posterior (MP).
• Occurs in 0.2% of all deliveries.
• Breech presentations (36,37)
• Higher incidence of congenital anomalies in breech versus cephalic (6.3% vs. 2.4%)
• Diagnosed by Leopold maneuvers, vaginal examination, or ultrasound
• Affects 3% to 4% of all deliveries
• Conditions that predispose to breech presentation:
 Prematurity
Prematurity
 Multiple gestation
Multiple gestation
 Abnormal placental implantation (fundal–cornual or previa)
Abnormal placental implantation (fundal–cornual or previa)
 Uterine anomalies or pelvic tumors
Uterine anomalies or pelvic tumors
 Polyhydramnios or oligohydramnios
Polyhydramnios or oligohydramnios
 Increased parity
Increased parity
• Three types of breech presentations (Fig. 10-6)
 Frank breech—flexion of hips, extension at knees
Frank breech—flexion of hips, extension at knees
 Complete breech—flexion at both hips and knees
Complete breech—flexion at both hips and knees
 Incomplete or footling breech—one or both hips deflexed with fetal knee or foot below fetal buttock
Incomplete or footling breech—one or both hips deflexed with fetal knee or foot below fetal buttock
• Transverse lie (Fig. 10-7)
 Diagnosed by Leopold maneuvers or ultrasound
Diagnosed by Leopold maneuvers or ultrasound
 Occurs in 0.3% of deliveries
Occurs in 0.3% of deliveries
 Occurs more commonly in similar situations that predispose to breech presentation (see above)
Occurs more commonly in similar situations that predispose to breech presentation (see above)
• Compound presentation
 More than one presenting part—an extremity prolapses beside the presenting part (most common is the head and an upper extremity)
More than one presenting part—an extremity prolapses beside the presenting part (most common is the head and an upper extremity)
 May be delivered vaginally if the vertex precedes the extremity
May be delivered vaginally if the vertex precedes the extremity
• Persistent occiput posterior (OP) position
• Diagnosed by vaginal examination
• May deliver vaginally (spontaneous, manual rotation, operative vaginal delivery)
• Occurs in approximately 5% at delivery (38)
• Persistent occiput transverse (OT) position
• Usually associated with pelvic abnormality (platypelloid or android pelvis)
• May delivery vaginally (spontaneous, manual, or forceps rotation)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


