9.4 APPROACH TO THE CHILD IN SHOCK
The child may present with fever, rash, pallor, poor feeding, drowsiness, a history of trauma or poisoning. Other than certain obvious causes of shock like external haemorrhage, signs and symptoms of early compensated shock can be easily missed. Early recognition of shock is crucial and requires a high index of suspicion and knowledge of the conditions that predispose children of different ages and co-morbidities to shock. For example, it is important to know any history of congenital heart disease, immunodeficiency, trauma, surgery, toxin ingestion or allergies. The initial clinical assessment should identify the child in shock.
9.5 PRIMARY ASSESSMENT
This is dealt with in Chapter 7. Below is a summary.
Airway
- Assess vocalising – crying or talking indicate ventilation and some degree of airway patency.
- Assess airway patency by:
- looking for chest and/or abdominal movement, symmetry and recession,
- listening for breath sounds and stridor, and
- feeling for expired air.
- looking for chest and/or abdominal movement, symmetry and recession,
- Reassess after any airway-opening manoeuvres. If there is still no evidence of air movement then airway patency can be assessed by giving rescue breaths (see Chapter 4).
Breathing
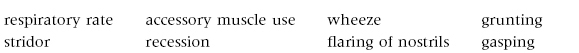
- Effort of breathing:
- Efficacy of breathing:
- chest expansion/abdominal excursion,
- breath sounds – reduced or absent, and symmetry on auscultation, and
- SpO2 in air.
- chest expansion/abdominal excursion,
- Effects of respiratory failure on other physiology:
- heart rate,
- skin colour, and
- mental status.
- heart rate,
Circulation
- Vital signs:
- heart rate,
- pulse volume, and
- blood pressure.
- heart rate,
- Skin and mucous membrane perfusion:
- capillary refill time (central and peripheral),
- temperature, and
- colour.
- capillary refill time (central and peripheral),
- Blood pressure
- Organ perfusion:
- effects on breathing,
- mental status, and
- urine output.
- effects on breathing,
Monitor the heart rate/rhythm, blood pressure, capillary refill time, core temperature and urine output. If the heart rate is above 200 beats/min in an infant or above 150 in a child, or if the rhythm is abnormal, perform a standard electrocardiogram (ECG). It is also important to check the blood gas for lactate, base excess and gas exchange.
Disability
- Mental status/conscious level (AVPU score).
- Pupillary size and reaction.
- Posture: children in shock are usually hypotonic.
Exposure
- Rash: this may be a key clinical indicator for the cause of shock (see Sections 9.9 and 9.10). There is a pathognomonic haemorrhagic rash associated with meningococcal septicaemia. In a child with non-specific symptoms there should be a thorough examination for a petechial/purpuric rash.
- Fever: suggests an infective cause.
- Injury: evidence of trauma.
- Consider poisoning.
9.6 RESUSCITATION
Airway
- Use an airway-opening manoeuvre, if airway is not patent or partially obstructed. If there is improvement, use airway adjuncts to support the airway.
- Suction.
- The airway may need to be secured by tracheal intubation.
Breathing
- All children in shock should receive high-flow oxygen through a face mask with a reservoir as soon as the airway has been demonstrated to be adequate.
- If the child is hypoventilating, respiration should be supported with oxygen via a bag–valve–mask device and experienced, senior help should be summoned for early tracheal intubation and mechanical ventilation.
Circulation
- Gain intravenous or intraosseous access:
- insert two short, wide-bore IV cannulae if possible,
- insert an intraosseous line if peripheral venous access is difficult due to poor perfusion,
- femoral venous access can be used in situations where peripheral or intraosseous access is impossible,
- using neck veins for access should ideally be reserved for experienced personnel, as there is a risk of pneumothorax, haemorrhage or exacerbation of an unsuspected neck injury, and
- techniques for vascular access are described in Chapter 21.
- insert two short, wide-bore IV cannulae if possible,
- Take blood for blood gas (including lactate and ionised calcium), bedside glucose and laboratory tests including full blood count (FBC), urea and electrolytes (U&Es), renal and liver function, C-reactive protein (CRP), blood culture, cross-match and coagulation studies.
- Give a 20 mL/kg rapid bolus of crystalloid (caution in those with primary cardiogenic shock and in those with signs of raised intracranial pressure (ICP)). Children with cardiac aetiology (i.e. myocarditis) leading to shock may still benefit from a cautious fluid bolus to optimise preload and, instead of 20 mL/kg, a 10 mL/kg fluid bolus should be considered.
- In children with signs suggestive of raised ICP (i.e. relative bradycardia and hypertension, posturing or seizures), hypotension is detrimental for cerebral perfusion, but excessive fluids carry the theoretical risk of worsening the cerebral oedema. Hence fluids should be given cautiously in 10 mL/kg aliquots with careful reassessment of clinical signs after each fluid bolus.
- Reassess the child after each fluid bolus to look for signs of improvement such as: fall in heart rate, improvement in skin perfusion and urine output, improved conscious level, increase in blood pressure and improvement in metabolic acidosis and lactate.
- Early tracheal intubation and mechanical ventilation should be considered in patients who have received more than 40 mL/kg and have signs of ongoing shock. Mechanical ventilation decreases the energy requirements of the heart and respiratory muscles, allows delivery of adequate concentrations of oxygen and helps reduce the risk of development of pulmonary oedema. It also facilitates placement of indwelling catheters for arterial and central venous access.
- Renal perfusion should be monitored with a urinary catheter and hourly urine output measurement as it is an important marker of renal perfusion.
- Give an antibiotic such as ceftriaxone or cefotaxime 50 mg/kg for those with an obvious or suspected diagnosis of septicaemia, e.g. in the presence of a purpuric rash, or in those where the aetiology is unknown.
- In paediatric practice, septicaemia is the commonest cause of shock. Unless an alternative diagnosis is very obvious (such as trauma, anaphylaxis or poisoning), antibiotics should be given as soon as possible, preferably after doing a blood culture.
- A third-generation cephalosporin, such as cefotaxime or ceftriaxone, is usually used, but an antistaphylococcal antibiotic (flucloxacillin, vancomycin) should be considered in possible toxic shock syndrome. (The latter is suggested by high fever, diffuse erythema, mucous membrane changes such as conjunctivitis, strawberry tongue, cracked lips and shock – findings may also include a trivial injury such as infected wound, cut, scratch, minor burn or scald, surgical wound infection or coexistent deep-seated infection such as pneumonia or bone/joint infection.)
- In children with trauma, haemorrhage must be looked for and controlled for effective management of shock. If there are no obvious wounds or fractures accounting for blood loss, thoracic, abdominal and pelvic cavities need to be assessed thoroughly for any signs of internal bleeding. If there are no signs of bleeding anywhere, spinal shock must be considered in patients with ongoing shock.
- If an arrhythmia is identified as a cause of shock, see Chapter 10.
- If anaphylaxis is obvious give adrenaline 10 micrograms/kg IM.
Disability
If there is coexistent evidence of raised intracranial pressure, manage as in Chapter 11.
‘Don’t Ever Forget Glucose’ (DEFG)
Hypoglycaemia may give a similar clinical picture to that of compensated shock. This must always be excluded by urgent bedside glucose and blood glucose estimation. Shock and hypoglycaemia may coexist due to limited glycogen reserves and the fact that ill children may not have had adequate nutritional intake.
9.7 KEY FEATURES OF THE CHILD IN SHOCK
While the primary assessment and resuscitation are being carried out, a focused history of the child’s health and activity over the previous 24 hours and any significant previous illness should be gained. Certain key features that will be identified from this – and the initial blood test results – can point the clinician to the likeliest working diagnosis for emergency treatment.
| • A history of vomiting and/or diarrhoea points to fluid loss either externally (e.g. gastroenteritis) or into the abdomen (e.g. volvulus, intussusception) | Section 9.8 |
| • The presence of fever and/or rash points to septicaemia | Section 9.9 |
| • The presence of urticaria, angioneurotic oedema or history of allergen exposure points to anaphylaxis | Section 9.10 |
| • The presence of cyanosis unresponsive to oxygen or a grey colour with signs of heart failure in a baby under 4 weeks points to duct-dependent congenital heart disease | Section 9.11 |
| • The presence of heart failure in an older infant or child points to cardiomyopathy or myocarditis | Section 9.12 |
| • A history of sickle cell disease or a recent diarrhoeal illness and a very low haemoglobin points to acute haemolysis. A history of sickle cell disease, abdominal pain and enlarged spleen points to acute splenic sequestration | Sections 9.13 and 9.14 |
| • An immediate history of major trauma points to blood loss and, more rarely, tension pneumothorax, haemothorax, cardiac tamponade or spinal cord transection | Part 4 |
| • The presence of severe tachycardia and an abnormal rhythm on the ECG points to a cardiac cause for shock | Chapter 10 |
| • A history of polyuria and the presence of acidotic breathing and a very high blood glucose points to diabetes ketoacidosis | Appendix B |
| • A history of drug ingestion points to poisoning | Appendix H |
9.8 APPROACH TO THE CHILD WITH FLUID LOSS
Infants are more likely than older children to present with shock due to sudden and rapid fluid losses due to gastroenteritis or with concealed fluid loss secondary to a ‘surgical abdomen’ such as a volvulus. This is due both to the infant’s low physiological reserve and increased susceptibility to these conditions.
In infants, gastroenteritis may occasionally present as circulatory collapse with little or no significant history of vomiting or diarrhoea. This is due to sudden massive loss of fluid from the bowel wall into the gut lumen, causing depletion of intravascular volume. The infecting organism can be any of the usual diarrhoeal pathogens, of which viruses are the most common. Having completed the primary assessment and resuscitation and identified by means of the key features that fluid loss is the most likely diagnosis, the child is reassessed to identify the response to the first fluid bolus.
Emergency Treatment of Fluid Loss
- Reassess ABC.
- Check that the child has had one fluid bolus of 20 mL/kg IV.
- If signs of shock persist after the first bolus, give a second fluid bolus of crystalloid or colloid:
- in gastroenteritis, one to two boluses usually restore circulating volume, and
- in gastroenteritis, initiate enteral or gastric tube oral rehydration solution (see Appendix B).
- in gastroenteritis, one to two boluses usually restore circulating volume, and
- Recheck acid–base status and electrolytes:
- acidosis will usually be corrected by treatment of shock; bicarbonate losses need to be corrected only in children who could have had large bicarbonate losses in the stool, and
- sodium imbalance may occur, and this may cause convulsions (see Appendix B).
- acidosis will usually be corrected by treatment of shock; bicarbonate losses need to be corrected only in children who could have had large bicarbonate losses in the stool, and
- Consider diagnostic possibilities:
- abdominal X-ray or ultrasound scan to detect distended bowel, intra-abdominal air or fluid,
- consider urgent surgical referral especially if bile-stained vomiting or abdominal guarding is present. Ensure that the child has had antibiotics as sepsis or toxic shock syndrome may mimic an acute abdomen, and
- consider sepsis (secondarily to the surgical abdomen) and give appropriate IV antibiotics.
- abdominal X-ray or ultrasound scan to detect distended bowel, intra-abdominal air or fluid,
- Consider tracheal intubation and mechanical ventilation, particularly if more than 40 mL/kg of fluid is required.
- Consider a third fluid bolus if still shocked; at this stage, colloid (4% human albumin solution) is commonly used.
- Consider the need for inotropes and monitoring of central venous pressure (CVP) – these will usually be essential if a third fluid bolus is given.
- The child’s bladder should have been catheterised in order to assess accurately the urinary output.
9.9 APPROACH TO THE CHILD WITH SEPTIC SHOCK
The incidence of septic shock varies with age and is highest in infants. It carries significant mortality and morbidity. Septic shock is the classic example of a combination of several factors contributing to the shock. These include:
- Hypovolaemia: fever, often associated diarrhoea, vomiting and anorexia, together with alterations in capillary permeability leading to capillary leakage.
- Cardiogenic elements: impaired cardiac function due to hypovolaemia and direct myocardial suppressive factors from infecting organisms and the host inflammatory response.
- Distributive elements: alterations in vascular tone with vasoconstriction in some vascular beds and vasodilatation in others.
- Dissociative elements: there is a non-specific sepsis-induced mitochondrial dysfunction impairing cellular oxygen utilisation.
Septic shock is defined as sepsis with cardiovascular organ dysfunction.
Infection with Neisseria meningitidis (meningococcus) is the commonest cause of community-acquired septicaemia in infants and children. In countries where a vaccine against meningococcus C has been introduced, there has been a significant fall in the number of cases of infection due to this organism. Other causes of septicaemia in children include group B streptococcal infection in young infants, Gram-negative sepsis in relation to underlying urinary tract or gut problems and group A streptococcal sepsis. In children with underlying co-morbidities, respiratory or neurological infection is important, and infection of long-term indwelling devices (such as venous catheters) is becoming increasingly prevalent.
The cardinal sign of meningococcal septicaemia is a purpuric rash in an ill child. At the onset, however, the rash may be absent, or mistaken for viral exanthem and a careful search should be made for purpura in any unwell child. In about 15% of patients with meningococcal septicaemia, a blanching erythematous rash replaces or precedes a purpuric one, and in 7% of cases no rash occurs.
In toxic shock syndrome, the initial clinical picture includes a high fever, headache, confusion, conjunctival and mucosal hyperaemia, scarlatiniform rash, subcutaneous oedema, vomiting and watery diarrhoea. Early administration of antistaphylococcal and antistreptococcal antibiotics, concurrent with initial resuscitation, is vital. Intravenous immunoglobulin should be considered along with urgent drainage of any localised pus. Early adequate fluid resuscitation is the key to survival in children with septic shock; however, indiscriminate or overaggressive fluid resuscitation can be harmful. The choice of fluid is still debated; septic children requiring multiple fluid boluses could be given colloid after the initial 20–40 mL/kg of crystalloid fluid if available. Having completed the primary assessment and resuscitation and identified by means of the key features that septicaemia is the most likely diagnosis, the child is reassessed.
Emergency Treatment of Septicaemia
- Reassess ABC.
- Give fluid bolus(es) of 0.9% saline:
- subsequent boluses should be either 0.9% saline or colloid, and
- children often require repeated boluses of fluid to achieve relative stability (up to 200 mL/kg in the first 24 hours has been used to treat severe shock, i.e. 2.5 times the blood volume).
- subsequent boluses should be either 0.9% saline or colloid, and
- After 40 mL/kg, if there are signs of ongoing shock and a continuing need for fluid resuscitation, tracheal intubation and mechanical ventilation should be considered. It will be necessary to consider inotropes and ideally to monitor CVP.
- Ensure that appropriate broad-spectrum antibiotics have been given (Table 9.2).
- Central venous access will be valuable, particularly in shock needing ≥40 mL/kg. It should ideally be achieved using a multilumen catheter. The femoral approach is most commonly used, and if expertise is available, the internal jugular vein can also be used. Adult data suggest that the optimal CVP is 8 cmH2O (0.8 kPa). Optimising CVP can improve cardiac output with less risk of inducing heart failure. Cardiac failure may be induced by excessive IV fluids, especially if severe anaemia, malnutrition or a primary cardiac disorder is present. Inotropic support will be required. Recent data suggest that the measurement of central venous oxygen saturation (SCVO2) from a central vein in the neck is useful to determine oxygen delivery and utilisation to guide resuscitation, aiming for a SCVO2 of >70%.
- Consider tracheal intubation by rapid sequence induction of anaesthesia and provide assisted ventilation:
- positive pressure ventilation can improve oxygenation, and prevents/treats pulmonary oedema; it can improve cardiac output,
- all intubated children must have continuous SpO2 and capnography, with frequent blood gas monitoring.
- positive pressure ventilation can improve oxygenation, and prevents/treats pulmonary oedema; it can improve cardiac output,
- Consider an inotrope if a third bolus of fluid is required.
- Inotropes can temporarily be given through a peripheral vein until central venous access or intraosseous access is obtained. Do not hesitate to increase the infusion rapidly in the face of a poor response.
Table 9.2 Antibiotics in sepsis.
| Antibiotic | Dose | Comment |
| Cefotaxime | 50 mg/kg (max. 2 g) | Doses of up to 100 mg/kg may be used in suspected meningitis |
| or | ||
| Ceftriaxone | 50 mg/kg (max. 2 g) | |
| And | ||
| Flucloxacillin | 50 mg/kg (max. 2 g) | To cover Staphylococcus aureus |
| or | ||
| Vancomycin | 15 mg/kg (max. 500mg) over 1 hour | Use in areas with high incidence of MRSA |
| Consider | ||
| Clindamycin | 10 mg/kg (max. 600 mg) over 1 hour | Use if toxic shock |
MRSA, meticillin-resistant Staphylococcus aureus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


