Four cardiac arrest rhythms will be discussed in this chapter:
The four are divided into two groups: two that do not require defibrillation (called ‘non-shockable’) and two that do require defibrillation (‘shockable’).
6.2 NON–SHOCKABLE RHYTHMS
This includes asystole and pulseless electrical activity.
Asystole
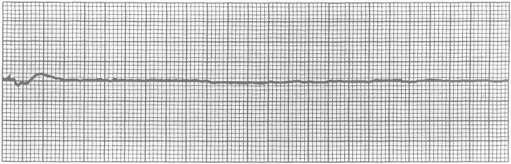
This is the most common arrest rhythm in children, because the response of the young heart to prolonged severe hypoxia and acidosis is progressive bradycardia leading to asystole (Figure 6.2). The electrocardiogram (ECG) will distinguish asystole from ventricular fibrillation, ventricular tachycardia and pulseless electrical activity (PEA). The ECG appearance of ventricular asystole is an almost straight line; occasionally P-waves are seen. Check that the appearance is not caused by an artifact, e.g. a loose wire or disconnected electrode. Turn up the gain on the ECG monitor.
Pulseless Electrical Activity
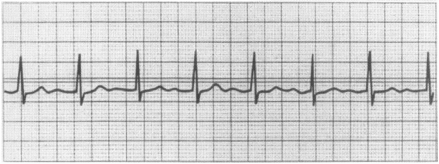
This is the absence of signs of life or a palpable pulse despite the presence on the ECG monitor of recognisable complexes that normally produce perfusion (Figure 6.3). PEA is treated in the same way as asystole and is often a pre-asystolic state.
Pulseless electrical activity may be due to an identifiable and reversible cause. In children, trauma is most often associated with a reversible cause of PEA. This may be severe hypovolaemia, tension pneumothorax or pericardial tamponade. PEA is also seen in hypothermic patients and in patients with electrolyte abnormalities, including hypocalcaemia from a calcium channel blocker overdose. Rarely in children it may be seen after massive pulmonary thromboembolus.
Management of Asystole/Pulseless Electrical Activity
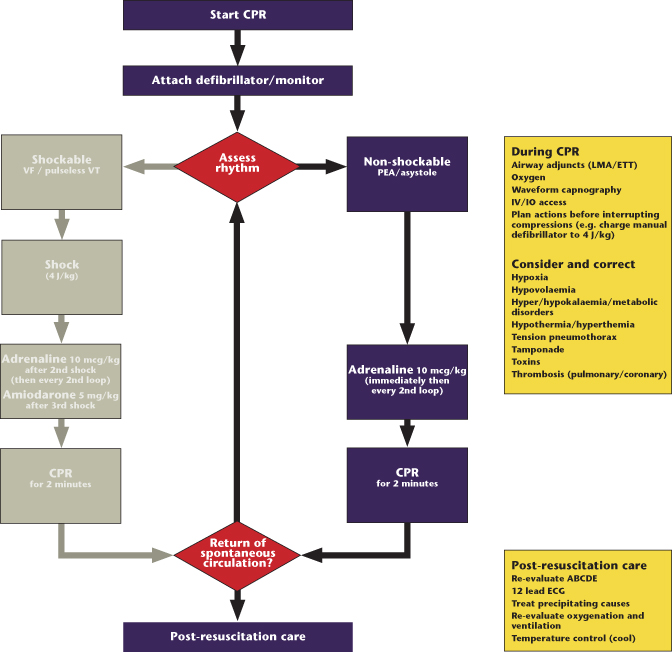
The algorithm for asystole and PEA is shown in Figure 6.4.
Figure 6.4 Algorithm for asystole and pulseless electrical activity (PEA). CPR, cardiopulmonary resuscitation; ECG, electrocardiogram; ETT, endotracheal tube; IO, intraosseous; IV, intravenous; LMA, laryngeal mask airway; VF, ventricular fibrillation; VT, ventricular tachycardia.
(Modified from Australian Resuscitation Council and New Zealand Resuscitation Council for use by trained medical professionals. Original ARC/NZRC algorithm available at www.resus.org.au.)
The essential first action is to establish effective ventilations and chest compressions. Ventilations are provided initially by bag-and-mask with high-concentration oxygen. Ensure a patent airway, initially using an airway manoeuvre to open the airway and stabilising it with an airway adjunct.
Provide effective chest compressions at a rate of 100 per minute with a compression : ventilation ratio of 15 : 2. The depth of compression should be at least one-third of the anteroposterior diameter of the chest. The child should have a cardiac monitor attached and the heart’s rhythm assessed. Although the procedures to stabilise the airway and gain circulatory access are now described sequentially, they should be undertaken simultaneously under the direction of a resuscitation team leader.
If asystole or PEA is identified, give adrenaline 10 micrograms/kg intravenously or intraosseously. Adrenaline is the first-line drug for asystole. Through α-mediated vasoconstriction, its action is to increase aortic diastolic pressure during chest compressions and thus coronary perfusion pressure and the delivery of oxygenated blood to the heart. It also enhances the contractile state of the heart and stimulates spontaneous contractions. The intravenous (IV) or intraosseous (IO) dose is 10 micrograms/kg (0.1 mL/kg of 1 : 10,000 solution). If venous access is not immediately attainable, obtain IO access. Central lines provide more secure long-term access, but compared to IO or peripheral IV access, offer no advantages. In each case the adrenaline is followed by a 0.9% saline flush (2–5 mL).
If circulatory access cannot be gained, the tracheal tube may be used but this is the least satisfactory route because of highly variable absorption and should be avoided. If the route is used, 10 times the intravenous dose (100 micrograms/kg) should be given. The drug should be injected quickly down a narrow-bore suction catheter beyond the tracheal end of the tube and then flushed in with 1 or 2 mL of 0.9% saline.
As soon as is feasible a skilled and experienced operator should intubate the child’s airway. This will both control and protect the airway and enable chest compressions to be given continuously, thus improving coronary perfusion. Both cuffed and uncuffed tracheal tubes are acceptable for infants and children undergoing emergency intubation (see Chapters 5 and 20). Once the child has been intubated and compressions are uninterrupted, the ventilation rate should be 10–12 per minute. This rate of ventilation matches perfusion during CPR. Overventilation during CPR is potentially harmful due to cerebral vasoconstriction from hypocarbia. It is important for the team leader to assess that the ventilations remain adequate when chest compressions are continuous.
During and following the administration of adrenaline, chest compressions and ventilations should continue. It is vital that chest compressions and ventilations continue uninterrupted during advanced life support as they form the basis of the resuscitative effort. The only reason to interrupt BLS is to shock the child if needed and to check the rhythm. It may be necessary to briefly interrupt during difficult intubation. Giving chest compressions is tiring for the operator so the team leader should change the operator every few minutes and continuously ensure that the compressions are achieving the recommended rate of 100 compressions per minute, together with a depression of the chest wall by at least one-third of the anteroposterior diameter of the chest.
At intervals of 2 minutes, briefly pause in the delivery of chest compressions to allow for simultaneous assessment of return of spontaneous circulation (ROSC) and rhythm. ROSC is indicated by the presence of a definite pulse, signs of responsiveness or normal breathing. Unless there is definite ROSC, immediately recommence external cardiac compression and treat the rhythm accordingly. If continued external cardiac compression is required, take the opportunity to change rescuers at the 2-minute check since they tire after 2 minutes.
If there is ROSC, assess for adequacy of breathing and circulation. Until adequate spontaneous breathing returns, ventilate at 12–20 breaths per minute. Continue compressions if the pulse rate is below 60 per minute with poor perfusion.
In addition, if at any time there is regular respiratory effort, coughing, eye opening or a sudden increase in end-tidal carbon dioxide (see below) stop CPR and check the monitor.
Reversible Causes
During CPR continually consider and correct reversible causes of the cardiac arrest based on the history of the event, known underlying illness in the child and any clues that are found during resuscitation. The causes of cardiac arrest in infancy and childhood are multifactorial but the two commonest pathways are through hypoxia and hypovolaemia.
All factors are conveniently remembered as the 4Hs and 4Ts:
- Hypoxia is a prime cause of cardiac arrest in childhood and is key to successful resuscitation.
- Hypovolaemia may be significant in arrests associated with trauma, anaphylaxis and sepsis and requires the infusion of crystalloid (see Chapters 9 and 13).
- Hyperkalaemia, hypokalaemia, hypocalcaemia and other metabolic abnormalities may be suggested by the child’s underlying condition (e.g. renal failure), tests taken during the resuscitation or clues given in the ECG (see Appendices A and B). Intravenous calcium (0.5 mL/kg of 10% calcium gluconate) is indicated in hyperkalaemia, hypocalcaemia and calcium channel blocker overdose.
- Hypothermia is associated with drowning incidents and requires particular care; a low reading thermometer must be used to detect it (see Chapter 19).
- Tension pneumothorax and cardiac tamponade are especially associated with PEA and found in trauma cases (see Chapter 14).
- Toxic substances either as a result of accidental or deliberate overdose or from an iatrogenic mistake may require specific antidotes (see Appendix H).
- Thromboembolic phenomena are much less common in children than in adults.
Adrenaline Dosage
Adrenaline has been used for many years although its place has never been subjected to trial against placebo in children. In adults a prospective randomised study of drugs, including adrenaline, showed an improvement in ROSC but no increase in long-term neurologically intact survival. Its use is supported by animal studies and its known effects in improving relative coronary and cerebral perfusion. There was a trend to the use of higher doses of adrenaline in past years but evidence now links high dosage to poorer outcome, especially in asphyxial arrests. High-dose (100 micrograms/kg) adrenaline should only be used in very specific circumstances, e.g. if necessary after cardiac arrest associated with ß-blocker overdose.
Alkalising Agents
Children with asystole will be acidotic as cardiac arrest has usually been preceded by respiratory arrest or shock. However, the routine use of alkalising agents has not been shown to be of benefit. Sodium bicarbonate therapy increases intracellular carbon dioxide levels so administration, if used at all, should follow assisted ventilation with oxygen and effective BLS. Once ventilation is ensured and adrenaline plus chest compressions are provided to maximise circulation, the use of sodium bicarbonate may be considered for a child with prolonged cardiac arrest. These agents should be administered only in cases where profound acidosis is likely to adversely affect the action of adrenaline. In addition, sodium bicarbonate is recommended in the treatment of patients with hyperkalaemia (see Appendix B) and tricyclics antidepressant overdose (see Appendix H).
In the arrested child, arterial pH does not correlate well with tissue pH. Mixed venous or central venous pH should be used to guide any further alkalising therapy. It should always be remembered that good BLS is more effective than alkalising agents at raising myocardial pH.
Bicarbonate is the most common alkalising agent currently available, the dose being 1 mmol/kg (1 mL/kg of an 8.4% solution). If it must be used remember the following:
- Bicarbonate must not be given in the same intravenous line as calcium because precipitation will occur.
- Sodium bicarbonate inactivates adrenaline and dopamine and therefore the line must be flushed with saline if these drugs are subsequently given.
- Bicarbonate must not be given by the intratracheal route.
Calcium
In the past, calcium was recommended in the treatment of PEA and asystole, but there is no evidence for its efficacy. However there is evidence for harmful effects as calcium is implicated in cytoplasmic calcium accumulation in the final common pathway of cell death. This results from calcium entering cells following ischaemia and during the reperfusion of ischaemic organs.
Administration of calcium in the resuscitation of asystolic children is not recommended. Calcium is indicated only for treatment of documented hypocalcaemia and hyperkalemia, and for the treatment of hypermagnesaemia and of calcium channel blocker overdose.
Atropine
Atropine has no place in the management of cardiac arrest. Its use is to combat excessive vagal tone causing bradycardia in the child who nonetheless has a perfusing rhythm.
6.3 SHOCKABLE RHYTHMS
Ventricular Fibrillation and Pulseless Ventricular Tachycardia
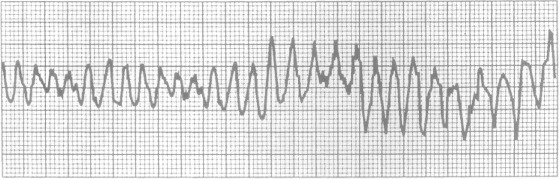
ECGs showing ventricular fibrillation (VF) and ventricular tachycardia (VT) are shown in Figures 6.5 and 6.6, respectively. These arrhythmias are less common in children but either may be suspected in sudden collapse, those suffering from hypothermia, poisoning by tricyclic antidepressants and those with cardiac disease. The algorithm for VF and pulseless VT is the same and is shown in Figure 6.7.
Figure 6.5 Ventricular fibrillation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree