- History of exposure to smoke in a confined space
- Burns around the mouth and nose
- Carbonaceous sputum
- Cough
- Hoarseness
- Weak voice
- Stridor
The rapid oedema that follows thermal injury above the larynx can cause obstruction within hours. Thus even a suspicion of airway compromise, or the discovery of injuries that might be expected to cause problems with the airway at a later stage, should lead to immediate consideration of tracheal intubation. This procedure increases in difficulty as oedema progresses; it is therefore important to perform it as soon as possible. All but the most experienced should seek expert help urgently, unless apnoea requires immediate intervention.
If there is any suspicion of cervical spine injury, or if the history is unobtainable, appropriate precautions should be taken until such injury is excluded.
Breathing
Once the airway has been secured, the adequacy of breathing should be assessed. Signs that should arouse suspicion of inadequacy include abnormal rate, abnormal chest movements and cyanosis (a late sign). Circumferential burns to the chest or abdomen (the latter in infants) may cause breathing difficulty by mechanically restricting chest movement.
All children who have suffered burns should be given high-flow oxygen. If there are signs of breathing problems, then intubation and ventilation should be commenced.
Circulation
In the first few hours following injury, signs of hypovolaemic shock are rarely attributable to burns. Therefore any such signs should raise the suspicion of bleeding from elsewhere and the source should be actively sought. Intravenous access should be established with two cannulae during resuscitation, and fluids started. If possible, intravenous lines should be put up in unburnt areas, but burned skin (eschar) can be used if necessary. Remember that the intraosseous route can be used. Blood should be taken for haemoglobin, haematocrit, electrolytes and urea, blood glucose and cross-matching. Many blood gas analysers provide carboxyhaemoglobin levels, which may be elevated and require specific treatment.
Disability
A reduced conscious level following burns may be due to hypoxia (remember that smoke-filled rooms may contain little oxygen), carbon monoxide or hydrogen cyanide poisoning, head injury or hypovolaemia. It is essential that a quick assessment is made during the primary survey as described in Chapter 13, because this provides a baseline for later observations.
Exposure
Exposure should be complete. Burned children lose heat especially rapidly, and should be kept in a warm environment and be covered with blankets when not being examined.
18.3 SECONDARY SURVEY AND LOOKING FOR KEY FEATURES
As well as being burned, children may suffer the effects of blast, may be injured by falling objects, or may fall while trying to escape from the fire. Thus other injuries are not uncommon and a thorough head-to-toe secondary survey must be carried out. This is described in Chapter 13. Any injuries discovered, including the burn, should be treated in order of priority.
Assessing the Burn
The severity of a burn depends on its relative surface area and depth. Burns to particular areas require special attention.
Surface Area
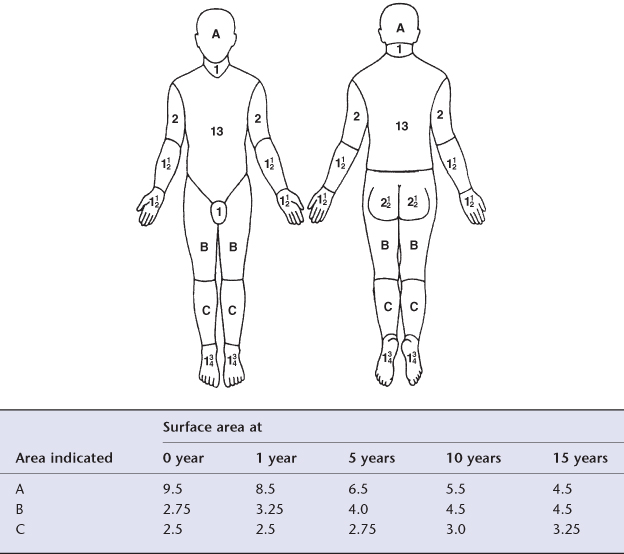
Surface area estimation is essential early during the child’s care as it guides initial resuscitation. At this stage it does not have to be accurate to the last 1–2%. Surface area is usually estimated using burns charts. It is important to use a paediatric chart when assessing burn size in children, because the relative surface areas of the head and lower limbs change with age. This variation is illustrated in Figure 18.1 and the table accompanying it.
Figure 18.1 Body surface area (percent).
(Reproduced courtesy of Smith & Nephew Pharmaceuticals Ltd)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


