- Face masks
- Airways including laryngeal mask airways
- Self-inflating bag–valve–mask devices
- Tracheal tubes, introducers and connectors
- Suction devices
- Cricothyroidotomy cannulae
The airway equipment indicated in the above box should be available in all resuscitation areas. It is crucial that familiarity with it is gained before an emergency situation occurs.
Pharyngeal Airways
There are two main types of pharyngeal airway: oropharyngeal and nasopharyngeal.
The oropharyngeal or Guedel airway is used in the unconscious or obtunded patient to provide a patent airway channel between the tongue and the posterior pharyngeal wall. It may also be used to stabilise the position of an oral endotracheal tube. In the awake patient with an intact gag reflex, it may not be tolerated and may induce vomiting.
The oropharyngeal airway is available in a variety of sizes. To estimate the correct size of the airway, place its flange at the centre of the incisor. It should then curve around the face to reach the angle of the mandible (Figure 5.1). Too small an airway may be ineffective, too large an airway may cause laryngospasm. Either may cause mucosal trauma or may worsen airway obstruction. Reassessment following placement is therefore a vital part of safe insertion of an airway device. Techniques for insertion are described in Chapter 20.
The nasopharyngeal airway is often better tolerated than the Guedel airway. It is contraindicated in fractures of the anterior base of the skull. It may also cause significant haemorrhage from the vascular nasal mucosa. A suitable length can be estimated by measuring from the lateral edge of the nostrils to the tragus of the ear. An appropriate diameter is one that just fits into the nostril without causing sustained blanching of the nostril. As small-sized nasopharyngeal airways may not be available, shortened endotracheal tubes may be used.
The acid test of success, as in all therapeutic interventions, is that insertion of one or other of these devices should result in improvement in the patient’s condition. If it does not occur then a reappraisal of the choice or size of airway is urgently required.
Laryngoscopes
Two principal designs of laryngoscope for use in children exist: straight bladed and curved bladed.
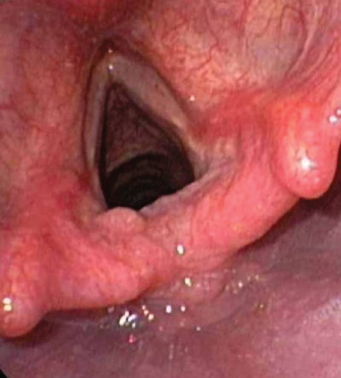
The straight-bladed laryngoscope is usually employed to directly lift the epiglottis, thereby uncovering the vocal folds (Figure 5.2). The advantage of this approach is that the epiglottis is moved sufficiently so that it does not obscure the cords. The disadvantage potentially is vagal stimulation causing laryngospasm or bradycardia.
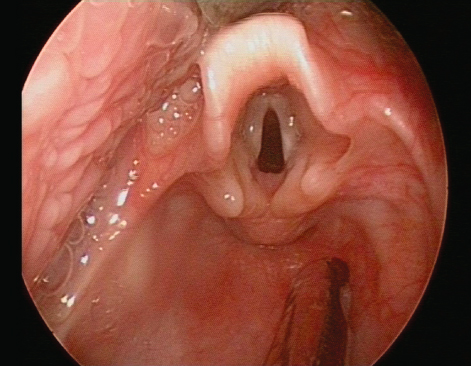
The curved-bladed laryngoscope is designed to move the epiglottis forward by lifting it from in front (Figure 5.3). The tip of the blade is inserted into the mucosal pocket, known as the vallecula, anterior to the epiglottis and the epiglottis is then moved forward by pressure in the vallecula. This may be equally effective at obtaining a view of the cords and has the advantage that less vagal stimulation ensues, as the mucosa of the vallecula is innervated by the glossopharyngeal nerve.
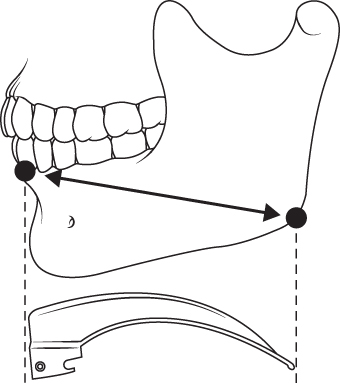
A laryngoscope blade should be chosen appropriate for age. It is possible to intubate with a blade that is too long but not one that is too short. An easy way to estimate the appropriate laryngoscope size is to measure the length of the blade (excluding handle insertion block) from the incisors to the angle of the jaw (Figure 5.4).
Laryngoscopes are notoriously unreliable pieces of equipment which may develop flat batteries and unserviceable bulbs very quickly between uses. It is vital, therefore, that a spare should be available at all times and that equipment should be regularly checked to ensure it is in good working order.
Tracheal Tubes
Both cuffed and uncuffed tubes are acceptable in infants and children undergoing emergency intubation, but not in neonates.
Until the age of about 10 years, the larynx is circular in cross-section and the narrowest part of it is at the cricoid ring, rather than the vocal cords. An appropriately sized tube should give a relatively gas-tight fit in the larynx but should not be so tight that no leak is audible when the bag is compressed. Failure to observe this condition may lead to damage to the mucosa at the level of the cricoid ring and to subsequent oedema following extubation.
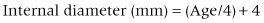
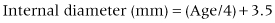
For uncuffed tracheal tubes, an estimate of the appropriate internal diameter for children from 1 year of age is carried out as follows:
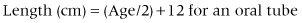
These formulae are appropriate for ages over 1 year. Neonates usually require a tube of internal diameter 3–3.5 mm, although pre-term infants may need one of diameter 2.5 mm. Cuffed tubes should not be used in neonates.
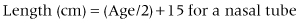
For cuffed tracheal tubes, an estimate of the appropriate internal diameter for children from 2 years is carried out as follows:
For infants of more than 3 kg and up to 1 year a size 3 cuffed tube, and from 1 to 2 years a size 3.5 cuffed tube, are usually acceptable. Tracheal tubes are measured in sizes by their internal diameter in millimetres. They are provided in whole- and half-millimetre sizes. The clinician should select a tube of appropriate size but also prepare one a size smaller and one a size larger.
In the circumstance of resuscitation in a young child where the lungs are very ‘stiff’, for example in a cardiac arrest from severe bronchiolitis, a cuffed tube rather than an uncuffed tube may be used by a non-expert but the risk of airway damage from the cuff must be balanced against the risk of failure to inflate the lungs.
Tracheal Tube Introducers
Intubation can be facilitated by the use of a stylet or introducer, placed through the lumen of the tracheal tube. There are two types: soft and flexible or firm and malleable. The former can be allowed to project out of the tip of the tube, as long as it is handled very gently. The latter is used to alter the shape of the tube, but can easily damage the tissues if allowed to protrude from the end of the tracheal tube. Tracheal tube introducers should not be used to force a tracheal tube into position.
Tracheal Tube Connectors
In adults, the proximal end of tube connectors is of standard size, based on the 15–22 mm system, ensuring that they can be connected to a standard self-inflating bag. The same standard Portex system exists for children, including neonates. Smaller connectors may be used later in intensive care units (in infants) but should be avoided in the resuscitation setting.
Magill Forceps
The Magill forceps is angled to allow a view around the forceps when in the mouth. It may be useful to help position a tube through the cords by lifting it anteriorly, or to remove pharyngeal or supraglottic foreign bodies.
Suction Devices
In the resuscitation room, the usual suction device is the pipeline vacuum unit. It consists of a suction hose inserted into a wall terminal outlet, a controller (to adjust the vacuum pressure), a reservoir jar, suction tubing and a suitable sucker nozzle or catheter. In order to aspirate vomit effectively, it should be capable of producing a high negative pressure and a high flow rate, although these can be reduced in non-urgent situations, so as not to cause mucosal injury.
The most useful suction ending is the Yankauer sucker, which is available in both adult and paediatric sizes. It may have a side hole, which can be occluded by a finger, allowing greater control over vacuum pressure. In small infants, a suction catheter and a Y-piece are often preferred, but are less capable of removing vomit.
Portable suction devices are required for resuscitation in remote locations, and for transport to and from the resuscitation room. These are usually battery powered.
Tracheal Suction Catheters
These may be required after intubation to remove bronchial secretions or aspirated fluids. In general, the appropriate size in French gauge is numerically twice the internal diameter in millimetres, e.g. for a 3 mm tube the correct suction catheter is French gauge 6.
Cricothyroidotomy Cannulae and Ventilation Systems
Purpose-made cricothyroidotomy cannulae are available, usually in three sizes: 12 gauge for an adult, 14 gauge for a child and 18 gauge for a baby. They are less liable to kinking than intravenous cannulae and have a flange for suturing or securing to the neck.
In an emergency, an intravenous cannula can be inserted through the cricothyroid membrane. Initially the oxygen flow rate (in litres) should be set at the child’s age (in years) to provide some oxygenation (but no ventilation). A side hole can be cut in the oxygen tubing or a Y-connector can be placed between the cannula and the oxygen supply, to allow intermittent occlusion and achieve partial ventilation, as described in Chapter 20.
5.3 EQUIPMENT FOR PROVIDING OXYGEN AND VENTILATION
The equipment for oxygenation and ventilation indicated in the box should be readily available.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree