- Congenital anomalies: malformations and deformations
- Congenital anomalies associated with teratogens
- Congenital malformation secondary to maternal infections
- Consequences of maternal substance misuse
- Neonatal manifestations of maternal medical diseases
Introduction
The developing fetus is hugely influenced by its mother – 50% of its genes and all of its mitochondria are from the mother. Her womb provides the nurturing supportive environment and all the nutrition required during fetal development. It is therefore not surprising that if this environment is disturbed by maternal disease or behaviour, there may be consequences for the fetus, especially if that disturbance occurs in the first trimester during critical organ development. This chapter will consider some of the fetal consequences of maternal conditions. Genetic conditions are discussed in Chapter 8.
Congenital Anomalies: Malformations and Deformations
Estimates of the incidence of congenital anomalies vary widely and range from 1% to 7% of live births, depending on the definition of what constitutes an anomaly. In about 3% there is a major congenital anomaly, but the incidence is 7% if minor lesions such as skin haemangiomas and preauricular skin tags are included. It is highest in preterm and small for gestational age (SGA) infants. Congenital anomalies are the leading cause of perinatal mortality (20–25% of all perinatal deaths) and postneonatal deaths (25–30%). In addition, they constitute 25–30% of admissions to children’s hospitals and have major financial costs for society.
Congenital anomalies may be classified into deformations and malformations. Deformations result from late changes in previously normal structures by destructive pathological processes or intrauterine (extrinsic) forces; for example, talipes, hydrocephalus and bowel atresia. Malformations result from a disturbance of growth during embryogenesis; for example, congenital heart disease. Some defects may arise by both mechanisms.
Deformations
Deformations may be single or multiple. They have many common aetiological factors, which are listed in Box 4.1.
- Oligohydramnios
- Uterine abnormalities, e.g. fibroids, bicornuate or septate uterus
- Multiple pregnancy
- Abnormal presentation, e.g. breech position
- Intrauterine growth restriction
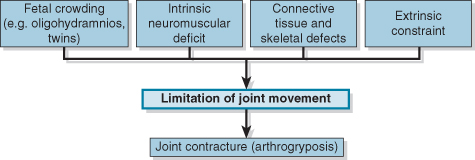
Extrinsic forces may cause a single localized deformation, such as talipes equinovarus or a deformation sequence. Examples of the latter are the oligohydramnios sequence, with contractures, facial dysmorphism and pulmonary hypoplasia, or the breech deformation sequence. Intrauterine contractures that give rise to joint fixation are known as arthrogryposis. The types of problems that lead to prenatal joint contractures are shown in Fig. 4.1.
Malformations
Incidence
Major congenital anomalies are either lethal or significantly affect the individual’s function or appearance. Minor anomalies have no functional or major cosmetic importance.
National registers of congenital malformations are available, but it is difficult to compare overall rates because of reporting differences. Most registers only include abnormalities present at birth. Due to miscarriage, stillbirth or termination of pregnancy the overall incidence may be much higher. There may also be large regional variations within a single country. Registers are increasingly including metabolic disorders and genetic disorders (e.g. cystic fibrosis) even if they have no physical characteristics present at birth.
The incidence of congenital malformations reported for South Australia from 1986 to 2003 was 5.7%, with annual variations from 4.5% to 6.0%. The UK figures are similar. The commonest major congenital anomalies involve the central nervous and cardiovascular systems. Table 4.1 lists the incidence of some congenital malformations.
Table 4.1 Major congenital anomalies by major anatomical systems (Australia 2002–2003)
| Congenital anomaly | Rate (per 1000 total births, including fetal deaths) | Rate (per 1000 total births and ToP before 20 weeks) |
| Central nervous system | ||
| Spina bifida | 0.27 | 0.47 |
| Anencephaly | 0.12 | 0.41 |
| Encephalocoele | 0.05 | 0.1 |
| Congenital hydrocephalus | 0.54 | 0.68 |
| Cardiovascular system | ||
| Transposition of great vessels | 0.40 | 0.47 |
| Hypoplastic left heart | 0.16 | 0.21 |
| Coarctation of aorta | 0.38 | 0.41 |
| Respiratory system | ||
| Congenital diaphragmatic hernia | 0.25 | 0.28 |
| Gastrointestinal system | ||
| Cleft lip ± cleft palate | 0.91 | 0.97 |
| Oesophageal atresia | 0.2 | 0.22 |
| Gastroschisis | 0.22 | 0.25 |
| Urogenital system | ||
| Hypospadias | 0.47 | 0.47 |
| Cystic kidney | 0.47 | 0.53 |
| Renal agenesis/dysgenesis | 0.48 | 0.56 |
| Limb | ||
| Polydactyly | 0.92 | 0.97 |
| Chromosomal | ||
| Trisomy 21 | 1.1 | 2.6 |
| Trisomy 13 | 0.07 | 0.26 |
| Trisomy 18 | 0.2 | 0.7 |
ToP, termination of pregnancy.
Causes of Congenital Malformations
Congenital anomalies result from a wide variety of mechanisms ranging from genetic (monogenic and polygenic) to environmental factors (teratogenesis), maternal metabolic disease, drugs and chemicals, infectious agents and irradiation (Table 4.2).
Table 4.2 Causes of congenital malformations
| Cause | Estimated contribution (%) |
| Genetic (mendelian inheritance) | 20 |
| Chromosomal | 10 |
| Polygenic | 25–30 |
| Teratogenic effect: | 6–9 |
| Congenital infection | 2–3 |
| Drugs and environmental pollutants/insecticides | 2–3 |
| Maternal metabolic disease | 1–2 |
| Radiation exposure | <1 |
| Unknown/idiopathic | 35–40 |
Genetic Malformations
These are discussed in Chapters 6 and 8.
Congenital Anomalies Associated with Teratogens
A teratogen is an agent (chemical, drug, virus or radiation) that affects the well-being of the fetus. A fetotoxin is an agent causing damage of any kind to the fetus, and a mutagen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree