- Weight
- Anatomical – size and shape
- Physiological – cardiovascular, respiratory and immune function
- Psychological – intellectual ability and emotional response
2.2 WEIGHT
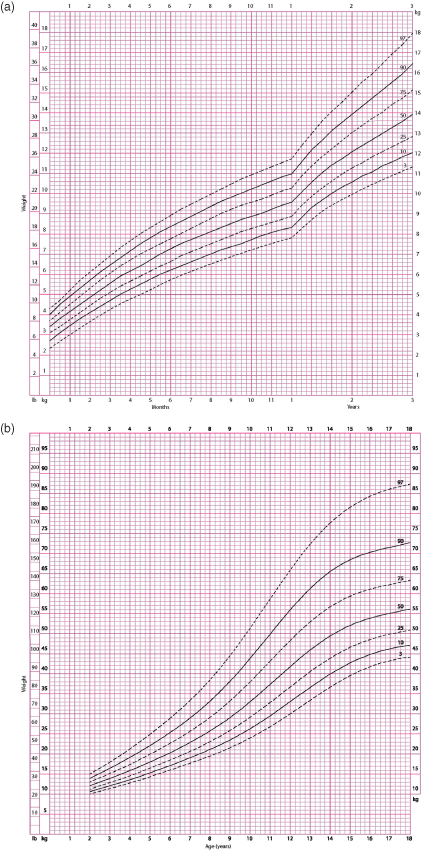
The most rapid changes in weight occur during the first year of life. An average birth weight of 3.5 kg will have increased to 10 kg by the age of 1 year. After that time weight increases more slowly until the pubertal growth spurt. This is illustrated in the weight charts shown in Figure 2.1.
Figure 2.1 (a) Weight percentile for girls aged 0–3 years, and (b) weight percentile for girls aged 2–18 years.
(Data source: Centers for Disease Control and Prevention, www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.htm.)
As most drugs and fluids are given as the dose per kilogram of body weight, it is important to determine a child’s weight as soon as possible. Clearly the most accurate method for achieving this is to weigh the child on scales; however, in an emergency this may be impractical. Often, especially with infants, the child’s parents or carer will be aware of a recent weight.
If weighing the child is not possible, various formulae or measuring tapes are available. The Broselow tapes use the height (or length) of the child to estimate weight. The tape is laid alongside the child and the estimated weight read from the calibrations on the tape. This is a quick, easy and relatively accurate method. Various formulae may also be used although they should be validated to the population in which they are being used.
If a child’s age is known the formulae given in Table 2.1 may be useful. The formula method has the added advantage of allowing an estimation of the weight to be made before the child arrives in hospital so that the appropriate equipment and drugs may be available.
Table 2.1 Weight formulae in different age groups.
| Works best for… | Formula |
| 0–12 months | Weight (in kg) = (0.5 × age in months) + 4 |
| 1–5 years | Weight (in kg) = (2 × age in years) + 8 |
| 6–12 years | Weight (in kg) = (3 × age in years) + 7 |
Whatever the method used, it is essential that the carer is sufficiently familiar with it to be able to use it quickly and accurately under pressure.
2.3 ANATOMICAL DIFFERENCES
As the child’s weight increases with age the size, shape and proportions of various organs also change. Particular anatomical changes are relevant to emergency care.
Airway
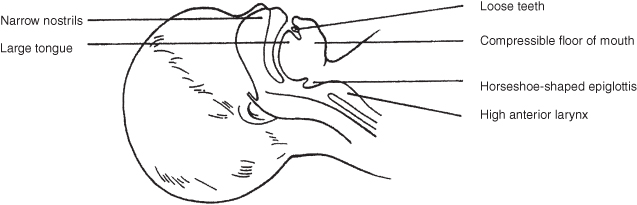
The airway is influenced by anatomical changes in the tissues of the mouth and neck. In a young child the head is large and the neck short, tending to cause neck flexion and airway narrowing. The face and mandible are small, and teeth or orthodontic appliances may be loose. The tongue is relatively large and not only tends to obstruct the airway in an unconscious child, but may also impede the view at laryngoscopy. Finally, the floor of the mouth is easily compressible, requiring care in the positioning of fingers when holding the jaw for airway positioning. These features are summarised in Figure 2.2.
The anatomy of the airway itself changes with age, and consequently different problems affect different age groups. Infants less than 6 months old prefer to breathe via their noses. As the narrow nasal passages are easily obstructed by mucous secretions, and as upper respiratory tract infections are common in this age group, these children are at particular risk of airway compromise. In 3–8-year-olds, adenotonsillar hypertrophy may be a problem. This not only tends to cause obstruction, but also causes difficulty when the nasal route is used to pass pharyngeal, gastric or tracheal tubes.
In young children the epiglottis is horseshoe-shaped, and projects posteriorly at 45°, making tracheal intubation more difficult. This, together with the fact that the larynx is high and anterior (at the level of the second and third cervical vertebrae in the infant, compared with the fifth and sixth vertebrae in the adult), means that it is easier to intubate an infant using a straight-blade laryngoscope. The cricoid ring is the narrowest part of the upper airway (as opposed to the larynx in an adult). The narrow cross-sectional area at this point, together with the fact that the cricoid ring is lined by pseudo-stratified ciliated epithelium loosely bound to areolar tissue, makes it particularly susceptible to oedema. As tracheal tube cuffs tend to lie at this level, uncuffed tubes are preferred in emergencies and for use by non-experts in pre-pubertal children.
The trachea is short and soft. Overextension of the neck as well as flexion may therefore cause tracheal compression. The short trachea and the symmetry of the carinal angles mean that not only is tube displacement more likely, but a tube or a foreign body may be displaced into the left or right main-stem bronchus.
Breathing
The lungs are relatively immature at birth. The air–tissue interface has a relatively small total surface area in the infant (less than 3 m2). In addition, there is a 10-fold increase in the number of small airways from birth to adulthood. Both the upper and lower airways are relatively small, and are consequently more easily obstructed. As resistance to flow is inversely proportional to the fourth power of the airway radius (halving the radius increases the resistance 16-fold), seemingly small obstructions can have significant effects on air entry in children.
Infants rely mainly on diaphragmatic breathing. Their muscles are more likely to fatigue as they have fewer type I (slow-twitch, highly oxidative, fatigue-resistant) fibres compared with adults. Pre-term infants’ muscles have even less type I fibres. These children are consequently more prone to respiratory failure.
The ribs lie more horizontally in infants, and therefore contribute less to chest expansion. In the injured child, the compliant chest wall may allow serious parenchymal injuries to occur without necessarily incurring rib fractures. For multiple rib fractures to occur the force must be very large; the parenchymal injury that results is consequently very severe and flail chest is tolerated badly.
Circulation
At birth the two cardiac ventricles are of similar weight; by 2 months of age the left ventricle (LV) is twice the weight of the right ventricle (RV). These changes are reflected in the infant’s electrocardiogram (ECG). During the first months of life the RV dominance is apparent, but by 4–6 months of age the LV is dominant. As the heart develops during childhood, the sizes of the P wave and QRS complex increase, and the P–R interval and QRS duration become longer.
The child’s circulating blood volume per kilogram of body weight (70–80 mL/kg) is higher than that of an adult, but the actual volume is small. This means that in infants and small children, relatively small absolute amounts of blood loss can be critically important.
Body Surface Area
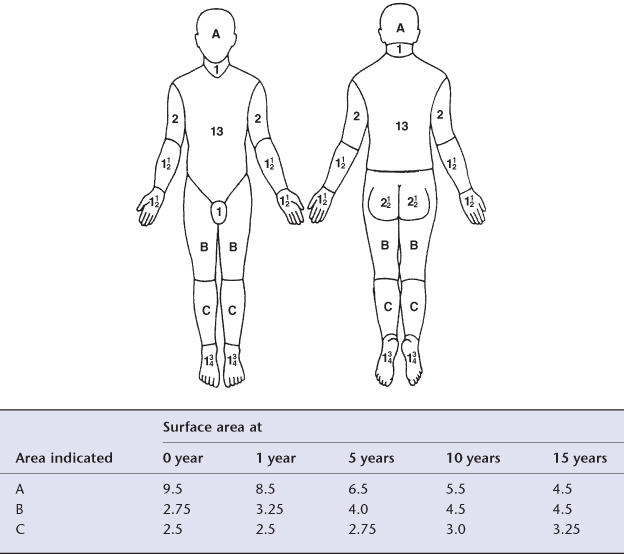
The body surface area (BSA) to weight ratio decreases with increasing age. Small children, with a relatively high surface area, lose heat more rapidly and consequently are relatively more prone to hypothermia. At birth the head accounts for 19% of BSA; this falls to 9% by the age of 15 years. Figure 2.3 shows these changes.
Figure 2.3 Body surface area (%).
(Reproduced courtesy of Smith & Nephew Pharmaceuticals.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree