Key topics
- Definitions of terms commonly used in perinatal medicine
- The role of perinatal and neonatal audit
- Factors affecting perinatal death rates
- Prevention of perinatal mortality and low birth weight
Introduction
Conception, embryonic and fetal development, parturition and subsequent neonatal growth and development form a continuum. Obstetricians and neonatologists have, however, arbitrarily divided this into rigid categories, which are used to audit standards of care during the perinatal and subsequent periods. Unfortunately, international agreement regarding some of the terminology is lacking, and definitions within this developmental continuum given here are those used in the UK and Australia.
Definitions of Terms Commonly used in Perinatal Medicine
- Gestational age: this is calculated from the first day of the last normal menstrual period to the date of birth, and is expressed in completed weeks.
- Term delivery occurs when the infant is born at or after 37 and before 42 weeks’ gestation.
- Preterm delivery occurs if the infant is born less than 37 weeks’ gestation. In the UK and Australia, 6–9% of infants are born preterm.
- Post-term delivery occurs if the infant is born at or after 42 completed weeks of gestation. Approximately 1% of infants are born post-term.
- A live birth is one in which there are signs of life (breathing, heartbeat or spontaneous movement) after complete expulsion from the mother, irrespective of the gestational age or birthweight.
- A stillbirth, or fetal death, is defined as an infant expelled from the birth canal at or after 24 weeks of pregnancy who shows no signs of life and has no heartbeat. In Australia, stillbirth is defined as an infant born at or after 20 weeks’ gestation and/or weighing 400 g with no signs of life. As the definition varies from country to country, comparison of figures may be misleading.
The stillbirth rate is expressed as the number of infants born dead at or after 24 weeks per 1000 live births and stillbirths.
- Low birthweight (LBW) refers to any infant who weighs less than 2500 g at birth (WHO). In the UK and Australia, approximately 6% of live births are LBW. These infants are either born too early (preterm), or have grown inadequately in the uterus and are classed as ‘small for gestational age’. Some low birthweight infants may be both preterm and small for gestational age.
- Very low birthweight (VLBW) infants are those who weigh less than 1500 g at birth. Approximately 1–1.5% of liveborn infants are VLBW.
- Extremely low birthweight (ELBW) infants are those who weigh less than 1000 g at birth. This category accounts for approximately 0.7% of all births.
- Small for gestational age (SGA). This term is generally synonymous with the fetus who has suffered intrauterine growth restriction (IUGR). Diagnosis depends on accurate assessment of gestational age (see p. 4) and plotting of weight on an appropriate growth chart. There is no international consensus on the definition of SGA, which varies from less than the 10th, 5th or 3rd percentiles or more than two standard deviations below the mean birthweight. Accordingly, incidence figures will vary. In the UK, SGA is defined as a baby weighing below the 10th centile for gestational age. Asymmetrical SGA refers to a baby whose weight is below the 10th centile, but whose head is above the 10th centile. This usually indicates late-onset IUGR (p. 139).
- Perinatal mortality rate (PMR):
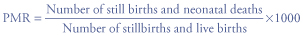
Different definitions are used depending upon location (see Table 2.1).
- Neonatal death

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


