- Physiology
- Apnoea
- Acute life-threatening events
- Sudden infant death syndrome or sudden unexpected death in infancy
- Upper airway obstruction
Introduction
Normal respiratory function is essential for successful transition to the extrauterine environment. The control of breathing is complex and is not fully developed at birth, particularly if the infant is preterm. Apnoea is one of the commonly encountered problems in the neonatal intensive care unit (NICU), and considerable time and effort goes into monitoring, preventing and treating babies with apnoea. The aetiology, investigation and management of apnoea is therefore discussed in detail in this chapter. Acute life-threatening events (ALTE) and sudden infant death syndrome (SIDS) are uncommon but serious events which are more commonly encountered in graduates of the intensive care nursery. Obstruction to gas flow in the upper airway can present in babies as apnoea, respiratory distress, coughing, a hoarse cry, or stridor. Common causes of airway obstruction and their management will be discussed.
Physiology
The onset of breathing begins early in fetal life. It is initially intermittent, irregular and occurs only during periods of active rapid eye movement (REM) sleep. The function of fetal breathing is not fully understood but, along with adequate amniotic fluid volume, it probably has an essential role in lung growth. Fetuses that do not breathe (due to either neurological or muscular disorders) are at significant risk of lung hypoplasia (see Chapter 13).
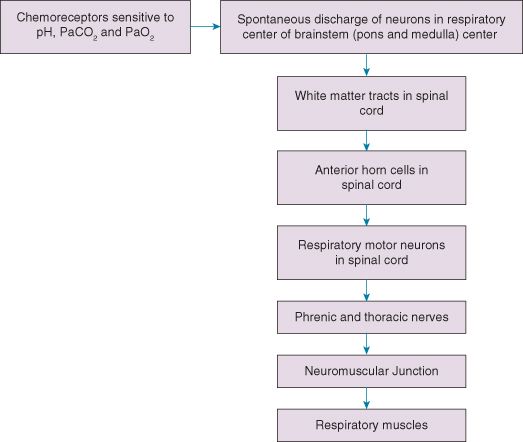
Successful transition to the extrauterine environment requires a marked change from the intermittent breathing of a fetus to the continuous breathing of a newborn baby. The control of breathing is complex (see Fig. 14.1), but we know that respiration is initiated in the respiratory nuclei found in the brainstem (pons and medulla). Hypercapnia increases respiratory activity and hypoxia causes an initial increase in respiratory activity lasting several minutes, followed by a decrease in ventilatory frequency. Preterm infants have less well-developed chemoreceptor responses to hypoxia and hypercapnia.
Breathing patterns in the newborn can be divided into four different types:
- Regular: there are nearly equal breath-to-breath intervals; this is infrequent
- Irregular: unequal breath-to-breath intervals; this is particularly common in preterm infants
- Periodic breathing: cycles of hyperventilation alternating with periods of hypoventilation and pauses in breathing lasting about 3 s
- Apnoea (see below).
With advancing gestation to term, the proportion of time the infant is breathing regularly increases, and phases of irregular, periodic and apnoeic periods decline. Further maturation occurs in the months after birth.
Apnoea
Clinically significant apnoea is defined as a cessation of breathing (absence of respiratory airflow) lasting for 20 s or more. Apnoea lasting for 10 s or more is also significant if accompanied by a desaturation (cyanosis or decreased SpO2), or bradycardia of less than 100 beats/min.
Apnoea is most common in preterm babies, particularly those born at less than 34 weeks’ gestation. It is seen in 25% of infants of birthweight less than 2500 g, and in over 80% of infants with birthweight below 1000 g. It is uncommon in the first 24 h of life, increasing towards the end of the first week of life, and then tends to become less frequent as the baby matures.
Types of Apnoea
Central Apnoea
Central apnoea accounts for 25% of all cases of neonatal apnoea. It is due to factors affecting the respiratory centre in the brainstem or the higher centres in the cerebral cortex.
Obstructive Apnoea
Complete obstruction of the airways will cause obstructive apnoea. Nasal obstruction (by bone/mucus/milk) will cause obstructive apnoea in babies as they are obligatory nose breathers. Obstructive apnoea is characterized initially by increased respiratory effort (baby attempts to overcome the obstruction) before the cessation of breathing. Obstructive apnoea accounts for 15% of cases and occurs with congenital malformations, such as choanal atresia and the Pierre Robin sequence. Preterm infants with small upper airways may have apnoea when in the supine position, especially during active (REM) sleep. Apnoea of this type may be minimized by nursing the infant in the prone position. Presence of milk, mucus or meconium in the upper airway is likely to provoke severe episodes of obstructive apnoea.
Mixed Apnoea
Mixed apnoea accounts for the majority (approximately 60%) of cases particularly in preterm infants, but may be difficult to diagnose clinically. Superficially it resembles central apnoea initially, with cessation of respiration, but then the baby makes intermittent respiratory efforts without achieving gas exchange.
Reflex Apnoea
Babies may develop reflex apnoea or vagally mediated apnoea due to vigorous suction of the pharynx, passage of a nasogastric tube, physiotherapy or sometimes even in response to defecation. Apnoea associated with gastro-oesophageal reflux may be reflex and/or obstructive.
Aetiology of Apnoea
A number of factors can increase the frequency of apnoea. Common causes are listed in Box 14.1. In the term infant the aetiology is usually identified. In the preterm infant, ‘apnoea of prematurity’ is the primary cause, but should be considered a diagnosis of exclusion. Apnoea of prematurity is predominantly a mixed apnoea.
- Apnoea of prematurity
- Lung disease (e.g. RDS, pneumothorax)
- Infection
- Airway obstruction (e.g. secretions, micrognathia, choanal atresia)
- Hypoxia
- Intracranial haemorrhage
- Metabolic causes (acidosis, hypoglycaemia, hypocalcaemia, hypomagnesaemia)
- Drugs (e.g. maternal narcotics, trishydroxyaminonethane (THAM), prostin (PGE1), magnesium sulphate)
- Gastro-esophageal reflux
- Seizures
- NEC
- Patent ductus arteriosus
- Temperature instability
- Polycythaemia with hyperviscosity syndrome
- CNS abnormalities (including Ondine’s curse – see Clinical Tip)
Investigation of Apnoea
Investigations are carried out to determine treatable causes of apnoea and will depend on the prevailing clinical condition. Investigations are listed in Box 14.2.
- Full blood count
- Blood culture
- Other cultures as indicated (urine, CSF, tracheal aspirate, nasal/pharyngeal, surface swabs, etc.)
- Chest radiograph
- Blood glucose
- Serum electrolytes, including calcium, magnesium and sodium
- Blood gas (arterial, venous or capillary)
- Continuous monitoring of oxygen saturation
- Ultrasound examination of the brain
- (In special circumstances) further neurological investigations, i.e. electroencephalogram (EEG), polygraphic sleep studies; PCR for the PHOX2B gene may identify cases of PAHS
Apnoea Monitoring
A variety of respiratory monitors are available, including a pressure-sensitive pad on which the infant lies, an air-filled plastic blister attached to the abdomen (SIMS Graseby Medical Ltd, Watford, UK) and impedance monitors using electrodes attached to the chest wall. None of these will detect obstructive apnoea until the infant stops fighting for breath. The use of an oxygen saturation monitor or an ECG monitor together with an apnoea monitor is recommended in high-risk infants in order to recognize bradycardia occurring with an obstructed airway.
Treatment of Apnoea
General Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree