Worldwide mortality rates in children have fallen substantially and consistently over the last 100 years. The World Health Organisation has estimated that the global infant mortality rate has fallen from 180 in 1950 to around 50 in 2010. In some developed countries the fall has been even more dramatic. For example in Australia the infant mortality rate in 1902 was 107; 100 years later in 2002 the figure had reduced to 5 where it stayed for the next 5 years. Even with figures at such low levels, the rates in developed countries have recently continued to fall. In England and Wales the infant mortality rates have more than halved in the last 28 years, falling from 12 in 1980 down to 4.5 in 2008: the lowest on record.
These dramatic improvements in infant mortality are due largely to improvements in living conditions such as sanitation, shelter, quality of drinking water and better nutrition. Some medical measures such as better obstetric and neonatal care and the advent of mass vaccination have also played substantial roles. The delivery of better acute care for seriously ill and injured children is likely to assist in reducing mortality rates further.
The mortality rate decreases significantly with the increasing age of the child, with the highest death rate occurring in the first 28 days, and indeed most deaths occur on the first day of life. Male children are more likely to die than females in all age groups, a trend which is not reversed until much later in life.
1.3 CAUSES OF DEATH IN CHILDHOOD
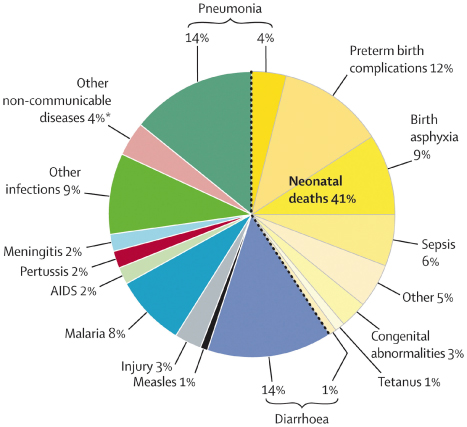
The causes of death in childhood in any country vary with age. Figure 1.1 shows the top worldwide causes of death for children under 6 years of age. In the newborn period the most common causes are congenital abnormalities, antepartum infections and factors associated with prematurity, such as respiratory immaturity, cerebral haemorrhage and infection due to immaturity of the immune response.
Figure 1.1 Top causes of death worldwide in children under 6 years of age.
(From The Lancet Vol. 375, 5 June 2010.)
In children aged 1–12 months, congenital abnormalities, conditions related to prematurity and sudden unexplained death each contribute around 20% to mortality. This is in contrast to a number of years ago when sudden infant death syndrome (as it was known then) was much more prevalent.
Congenital abnormalities contribute significantly to mortality rates during all stages of childhood. Complex congenital heart disease, central nervous system malformations, metabolic disorders and chromosomal anomalies are the commonest lethal disorders. After 1 year of age, trauma is a frequent cause of death and remains so until well into adult life. Deaths from trauma have been described as falling into three groups. In the first group there is overwhelming damage at the time of the trauma, and the injury caused is incompatible with life; children with such massive injuries will die within minutes whatever is done. Those in the second group die because of progressive respiratory failure, circulatory insufficiency or raised intracranial pressure secondary to the effects of injury; death occurs within a few hours if no treatment is administered, but may be avoided if treatment is prompt and effective. The final group consists of late deaths from raised intracranial pressure, infection or multiple organ failure. Appropriate management in the first few hours will also decrease mortality in this group.
In developing countries, infectious diseases are still major causes of death. Seven out of 10 childhood deaths can be attributed to just five main causes: pneumonia, diarrhoea, measles, malaria and malnutrition. Three out of every four children seen by health services are suffering from at least one of these conditions. Human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) have contributed to this and also been associated with increasing deaths from tuberculosis in countries affected. As these societies become more urbanised the mortality from trauma, especially from motor vehicle accidents, increases. In South Africa, a country that, although developing rapidly, has large areas of severe poverty, the under-fives mortality rate has recently been shown to include 40% (42,749) of deaths from HIV/AIDS, 11% (11,876) from low birth weight, 21% (22,680) from infections and 3% (3506) from trauma. In older South African children, trauma, especially road traffic accidents, homicide and suicide are leading causes of death. In Trinidad, children under 1 year of age accounted for 4% of deaths in 1997, with infant mortality at 17 per 1000 live births. In Trinidadian school children, the foremost cause of death was injury, with infections causing one-fifth of deaths.
In developed countries, many children with diseases that were once invariably fatal – such as complex congenital heart disease, inborn errors of metabolism, haematological malignancies or cystic fibrosis – are now treated with drugs, operations, diet, transplant or, soon, even gene therapy. In these children, common acute illnesses such as varicella or chest infections have potentially lethal consequences. They require a low threshold for rapid aggressive treatment delivered by a team with an understanding of their underlying disease.
Only a minority of childhood deaths, such as those due to end-stage neoplastic disease, are expected and ‘managed’. There should be timely discussions among the child, family and health carers to identify whether and in what manner resuscitation should be carried out to prevent unwanted and inappropriate resuscitation and interventions.
1.4 PATHWAYS LEADING TO CARDIORESPIRATORY ARREST
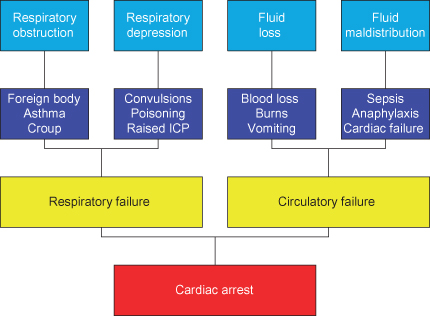
As the outcome from cardiorespiratory arrest in children is poor the only effective way to prevent death and permanent disability is to understand its antecedent events, and be able to recognise and treat them vigorously.
Cardiac arrest in children is rarely due to primary cardiac disease. This differs from the situation in an adult where the primary arrest is often cardiac, and circulatory and respiratory function may remain near normal until the moment of arrest.
In children, most cardiorespiratory arrests are secondary to hypoxia caused by respiratory pathology, including birth asphyxia, inhalation of foreign bodies, bronchiolitis and asthma. Respiratory arrest also occurs secondary to neurological dysfunction caused by such events as convulsion or poisoning. Raised intracranial pressure (ICP) due to head injury or acute encephalopathy eventually leads to respiratory arrest, but severe neuronal damage has already been sustained before the arrest occurs.
Whatever the cause, by the time of cardiac arrest the child has had a period of respiratory insufficiency that will have caused hypoxia and respiratory acidosis. The combination of hypoxia and acidosis causes cell damage and death (particularly in more sensitive organs such as the brain, liver and kidney) before myocardial damage is severe enough to cause cardiac arrest.
Most other cardiac arrests in children are secondary to circulatory failure. This will have resulted often from fluid or blood loss, or from fluid maldistribution within the circulatory system. The former may be due to gastroenteritis, burns or trauma, whilst the latter is often caused by sepsis or anaphylaxis. Because all organs are deprived of essential nutrients and oxygen as shock progresses to cardiac arrest, circulatory failure, like respiratory failure, causes tissue hypoxia and acidosis. In fact, both pathways may occur in the same condition. The pathways leading to cardiac arrest in children are summarised in Figure 1.2.
Figure 1.2 Pathways leading to cardiac arrest in childhood (with examples of underlying causes). ICP, intracranial pressure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


