- Placental function
- Fetal homeostasis
- Fetal circulation
- Assessment of fetal well-being
- Screening during pregnancy
- Fetal monitoring during labour
- Fetal compromise
Introduction
The discipline of ‘perinatal medicine’ spans the specialties of fetal medicine and neonatology. The obstetrician must have a thorough knowledge of pregnancy and its effects on the mother and fetus, as well as fetal development and physiology. The neonatologist specializes in the medical care of the infant immediately after birth but must also have a thorough understanding of fetal development and physiology. This chapter reviews fetal assessment and physiology to provide the paediatrician and neonatal nurse with a better understanding of normal perinatal adaptation and the adverse consequences arising from maladaptation.
Placental Function
The placenta is a fetal organ that has three major functions: transport, immunity and metabolism.
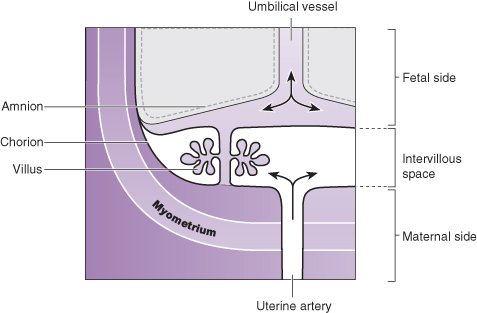
The uterus is supplied with blood from the uterine arteries, which dilate throughout pregnancy, increasing blood supply 10-fold by term. Maternal blood bathes the intervillous space and is separated from fetal blood by the chorionic plate. Transport of nutrients and toxins occurs at this level. Oxygenated fetal blood in the capillaries of the chorionic plate leaves the placenta via the umbilical vein to the fetus (Fig. 1.1).
Transport
The placenta transports nutrients from the mother to the fetus, and waste products in the other direction. This occurs in a number of ways, including simple diffusion (for small molecules) and active transport, which is used for larger molecules. The placenta is crucially also responsible for gaseous exchange of oxygen and carbon dioxide. Oxygen diffuses from the mother (PO2 = 10–14 kPa, 75–105 mmHg) to the fetus (PO2 = 2–4 kPa, 15–30 mmHg) where it binds to fetal haemoglobin. This has a higher affinity for oxygen than maternal haemoglobin for a given PO2. This off-loading of maternal haemoglobin is also facilitated by a change in maternal blood pH.
Immunity
The placenta trophoblast prevents the maternal immune system from reacting against ‘foreign’ fetal antigens. Rejection does not occur because the trophoblastic cells appear to be non-antigenic, although it is known that fetal cells can cross into the maternal circulation where they can trigger an immune reaction (e.g. rhesus haemolytic disease). Maternal IgG antibody, the smallest of the immunoglobulins, can cross the placenta where it provides the newborn with innate immunity to infectious diseases. These IgG antibodies can also cause perinatal disease such as transient hyperthyroidism (see Chapter 21).
Metabolism
The placenta is metabolically active and produces hormones, including human chorionic gonadotropin (hCG) and human chorionic thyrotropin (hCT). It also detoxifies drugs and metabolites. Oestriol cannot be produced by the placenta alone. This is done by the fetal liver and adrenal glands. The metabolites are then sulphated by the placenta to form oestrogens, one of which is oestriol.
Because of its metabolic activity, the placenta has very high energy demands and consumes over 50% of the total oxygen and glucose transported across it.
Fetal Homeostasis
The placenta is an essential organ for maintaining fetal homeostasis but the fetus is capable of performing a variety of physiological functions:
- The liver produces albumin, coagulation factors and red blood cells.
- The kidney excretes large volumes of dilute urine from 10–11 weeks’ gestation, which contributes to amniotic fluid.
- Fetal endocrine organs produce thyroid hormones, corticosteroids, mineralocorticoids, parathormone and insulin from 12 weeks’ gestation.
- Some immunoglobulins are produced by the fetus from the end of the first trimester.
Fetal Circulation
The fetal circulation is quite different from the newborn or adult circulation. The umbilical arteries are branches of the internal iliac arteries. These carry deoxygenated blood from the fetus to the placenta where it is oxygenated as it comes into close apposition with maternal blood in the intervillous spaces. Oxygenated fetal blood is carried in the single umbilical vein which bypasses the liver via the ductus venosus to reach the inferior vena cava. It then passes into the inferior vena cava and enters the right atrium as a ‘jet’, which is shunted to the left atrium across the foramen ovale (Fig. 1.2). From here it passes into the left ventricle and is pumped to the coronary arteries and cerebral vessels. In this way the fetal brain receives the most oxygenated blood. Some deoxygenated blood is pumped by the right ventricle into the pulmonary artery, but the majority bypasses the lungs via the ductus arteriosus to flow into the aorta where it is carried back to the placenta. Only 7% of the combined ventricular output of blood passes into the lungs. The right ventricle is the dominant ventricle, ejecting 66% of the combined ventricular output.
Figure 1.2 Diagram of the fetal circulation through the heart and lungs, showing the direction of flow through the foramen ovale and ductus arteriosus (DA).
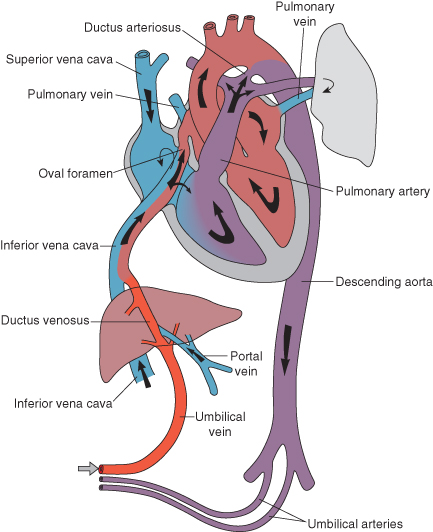
In summary, there are three shunts:
The last two shunts only occur because of the very high fetal pulmonary vascular resistance and the high pulmonary artery pressure that is characteristic of fetal circulation.
Umbilical Vessels
There are two umbilical arteries and one umbilical vein, surrounded by protective ‘Wharton’s jelly’. In 1% of babies there is only one umbilical artery, and this may be associated with growth retardation and congenital malformations, especially of the renal tract. Chromosomal anomalies are also slightly more common.
Assessment of Fetal Well-Being
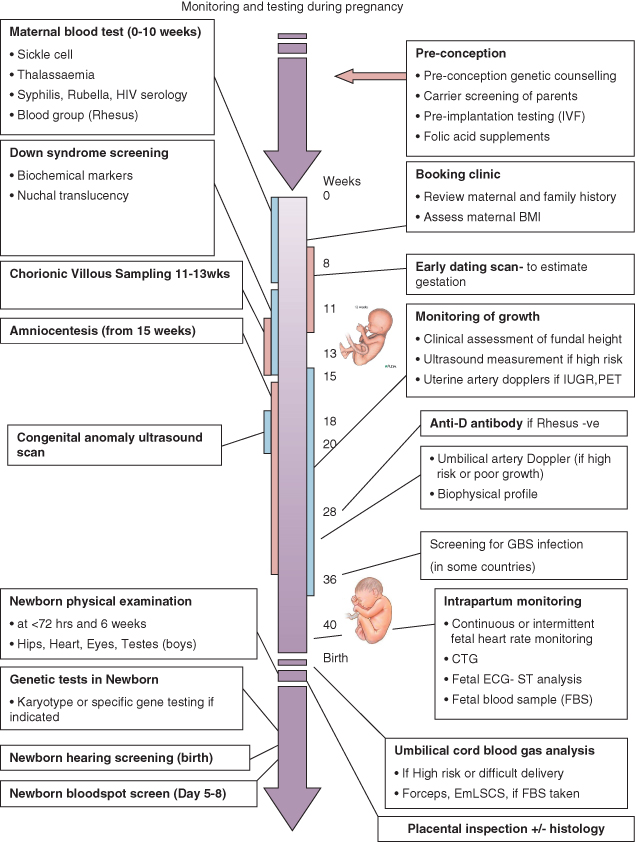
Assessment of fetal well-being is an integral part of antenatal care. It includes diagnosis of fetal abnormality, assessment of the fetoplacental unit and fetal maturity, monitoring of growth and well-being monitoring in the third trimester and during labour (Fig. 1.3).
Assessment of Maturity
Clinical Assessment
Assessment of gestational age depends on the date of the last menstrual period (LMP) and clinical measurement of fundal height: fundal height (cm) = gestational age (weeks). This is most accurate in early pregnancy. Fetal ‘quickening’ can help in dating the duration of pregnancy: in primiparas movements are first felt at about 20–21 weeks, and in multiparas at 18 weeks.
Ultrasound
Early measurement of fetal size is the most reliable way to estimate gestation and is considered to be even more reliable than calculation from the date of the LMP. Ultrasound measurements that correlate well with gestational age include crown–rump length (until 14 weeks), biparietal diameter (BPD) and femur length. The BPD measurement at 14–18 weeks appears to be the best method for assessing the duration of pregnancy.
Assessment of Fetal Growth and Well-Being
Clinical Assessment
Monitoring fundal height is a time-honoured method of assessing fetal growth. Unfortunately, up to 50% of growth-restricted infants are not detected clinically.
Ultrasound
Serial estimates of BPD, head circumference, abdominal circumference and femur length are widely used to monitor growth, often on customized fetal growth charts. In fetuses suffering IUGR, head growth is usually the last to slow down. Estimating fetal weight by ultrasound has become very accurate and provides critical information for perinatal decision-making about the timing of delivery.
 Link to Nursing the Neonate: Obstetric issues relating to neonatal care. Chapter 2, pp.14–19.
Link to Nursing the Neonate: Obstetric issues relating to neonatal care. Chapter 2, pp.14–19.Ultrasound Imaging and Doppler Blood Flow
The location of the placenta can be confidently established by ultrasound. Doppler flow velocity waveforms of the umbilical artery are now used as a major determinant of fetal well-being. In IUGR fetuses, abnormal Doppler waveforms are a reliable prognostic feature. As fetal blood flow become compromised there is reduced, then absent or reversed flow during diastole. Reversed diastolic flow is an ominous sign and is associated with a high risk of imminent fetal demise (see Fig. 1.4). If end-diastolic flow (EDF) is absent, detailed Doppler studies of the middle cerebral artery (MCA) and ductus venosus are indicated. Evidence of cerebral redistribution should trigger intensive regular monitoring. Timing of delivery will be based on Dopplers, gestation and estimated fetal weight. Recently, Doppler measurement of peak systolic blood flow velocity in the MCA has become a part of the assessment of fetal anaemia and isoimmunization. As anaemia becomes severe the velocity increases (see Chapter 20).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree