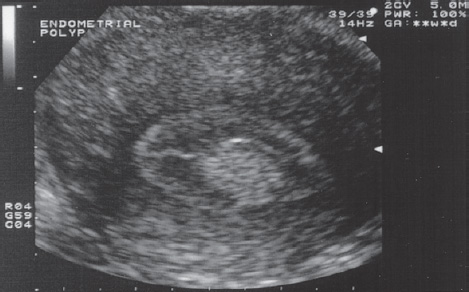
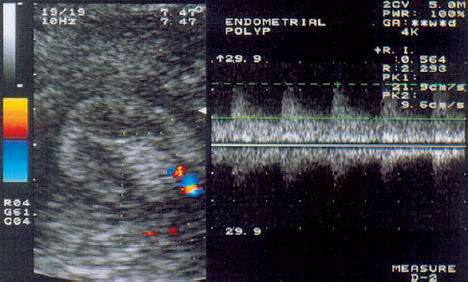
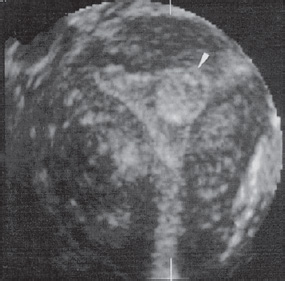
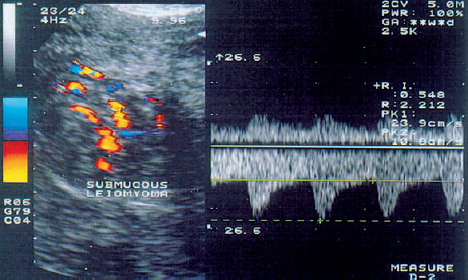
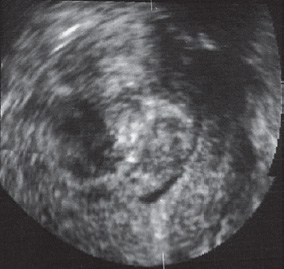
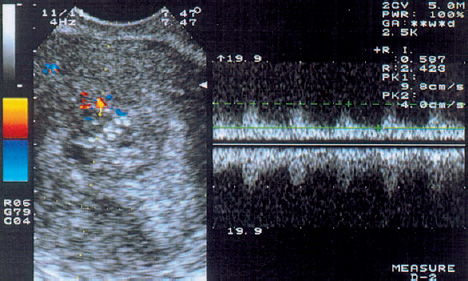
4 Uterine Causes of Infertility For fertilization to occur, the uterine cavity must create an optimum environment for the successful transport of spermatozoa from the cervix to the fallopian tubes. A normal structure of the uterine mucosa, with normal glandular secretions and blood flow, is also essential for implantation and placentation. Uterine abnormalities such as polyps, leiomyomas, malignant tumors, infections, and intrauterine adhesions and synechiae can contribute to fertility problems. Accordingly, numerous studies have been done to look for a correlation between sonographic parameters (endometrial thickness and echogenicity) and uterine receptivity to conception. This chapter explores the role of transvaginal and color Doppler sonography in evaluating endometrial changes during the menstrual cycle and in the detection of uterine abnormalities. Congenital anomalies of the uterus are diagnosed in 38–55% of women with habitual abortion33,47. Examination during the secretory phase. The ultrasound diagnosis of uterine anomalies such as a septate uterus, bicornuate uterus, or uterus didelphys is most sensitive and specific during the secretory phase of the menstrual cycle. The accuracy of the ultrasound diagnosis depends on the severity of the anomaly23. The endometrium is most clearly defined during the secretory phase, when separate echogenic lines demarcate the endometrium from the surrounding hypoechoic myometrium, making it easier to detect contour abnormalities (Fig. 4.1). Accordingly, a careful transvaginal ultrasound examination in a patient with a unicornuate uterus can demonstrate a single uterine cornu with an atypical endometrial echo24. Large intracavitary fluid collections should raise suspicion of hymenal or even vaginal atresia. Fig. 4.1 Uterine duplication anomaly demonstrated by transvaginal color Doppler sonography. Two separate endometrial images can be seen during the secretory phase of the menstrual cycle. Sonohysterography. Sonohysterography refers to the continuous sonographic visualization of the uterine cavity during and after the instillation of contrast medium into the uterus11. This method can accurately demonstrate uterine septa, for example, and can define their extent. In a study by Randolph et al.41, the results of sonohysterography agreed with hysteroscopic findings in 53 of 54 patients, corresponding to a sensitivity of 98% and a specificity of 100%. The interested reader can find more information on the ultrasound and color Doppler evaluation of uterine anomalies in Chapter 26 (p. 259 – 265). Endometrial polyps are known to have causal significance in habitual abortion and infertility. The polyps appear sonographically as diffuse or focal sites of endometrial thickening. On sonohysterography, an intracavitary polyp appears surrounded by echo-free fluid, and its site of attachment can generally be identified11 (Fig. 4.2). If the examination is performed in the follicular phase of the cycle, it is unnecessary to instill fluid in order to detect increased endometrial thickness (Fig. 4.3). Generally, however, polyps can be detected more easily in the periovulatory and secretory phases of the cycle by fluid instillation. The use of transvaginal color Doppler sonography makes it possible to identify small arteries that supply the endometrial polyps (Fig. 4.4). Three-dimensional ultrasound permits an accurate examination of the uterine cavity in which the polyps can be clearly visualized and delineated from the uterine wall (Fig. 4.5). Fig. 4.2 Transvaginal ultrasound examination of the uterus after the instillation of isotonic saline solution in an infertile patient with acyclic bleeding episodes. The area of increased endometrial thickness is a polyp. Fig. 4.3 Transvaginal ultrasound examination of the uterus shows a focal area of increased echogenicity: an endometrial polyp. Fig. 4.4 Transvaginal color Doppler examination shows a focal area of increased echogenicity bounded by an area with a normal vascular distribution. This pattern is typical of an endometrial polyp. The moderate to slightly increased resistance index in pulsed color Doppler (RI = 0.69) is consistent with a benign uterine mass. Fig. 4.5 Endometrial polyp demonstrated by three-dimensional ultrasound. The polyp appears as a localized area of endometrial thickening that does not completely fill the uterine cavity. Sonographic appearance. The diagnosis of a submucous leiomyoma (fibroid) is based on a distortion of the uterine contour, uterine enlargement, and a change in echo pattern (Fig. 4.6). Because leiomyomas contain variable amounts of smooth muscle and connective tissue, these benign tumors vary in their sonographic features41. They range from hypoechoic to hyperechoic, depending on the proportions of smooth muscle and connective tissue. Central ischemia can occur as the tumor grows and outstrips its blood supply, generally followed by varying stages of degeneration. The most frequent source of calcifications in the uterus is the degenerative calcification of a leiomyoma. Cystic, myxomatous, and hyaline forms of degeneration can also occur. Given the large range of variation in tumor appearance, it is not uncommon to confuse submucous leiomyomas with endometrial polyps, endometrial carcinoma, blood, or even mucus. Fig. 4.6 Transvaginal scan in a patient with an isoechoic submucous leiomyoma. Fig. 4.7 Same patient as in Fig. 4.6. Color Doppler demonstrates a large vessel in proximity to the leiomyoma. Fig. 4.8 Same patient as in Fig. 4.7. The color signals on pulsed Doppler examination (right) indicate moderate vascular resistance (RI = 0.55). Fedele et al.20 investigated the accuracy of transvaginal sonography in the detection of small submucous leiomyomas in patients who underwent transvaginal ultrasound scanning and hysteroscopy as a prelude to hysterectomy. The sensitivity/specificity of transvaginal sonography in this study was comparable to that of hysteroscopy. Effects on the endometrium. The uterine environment does not appear to be conductive to implantation of the fertilized ovum in patients with submucous leiomyomas. The blood supply may also be inadequate for this purpose30. Deligdish and Loewenthal13 conducted a histological study of the endometrium in patients with submucous leiomyomas. Atrophic changes were found in the endometrial glands and stroma in areas of endometrium that were located over or opposite to the leiomyoma, while the glands at the tumor margins tended to be hyperplastic. Increased vascularity and elevated estrogen levels were also observed. Farrer-Brown et al.19 were able to detect arterial obstruction and venous dilatation within the endometrium overlying a leiomyoma. This suggests that submucous leiomyomas cause a reduction in blood flow, which suppresses the release of hormones that are necessary for normal endometrial development. Ultimately these changes can lead to endometrial atrophy and inadequate placentation. Additionally, submucous leiomyomas can hamper both the growth of the fetus and the normal enlargement of the uterus50. Blood supply. Leiomyomas grow centripetally by the proliferation of smooth muscle cells and connective tissue, and they form a pseudocapsule consisting of compressed muscle fibers. As a result, most blood vessels are found at the periphery of the mass on color Doppler examination (Fig. 4.7). Blood vessels located at the center of leiomyomas are usually associated with necrosis, degenerative changes, or inflammatory processes. These vessels show a lower resistance index (RI) than peripherally located vessels and are occasionally misinterpreted as malignant tumor angiogenesis32. The flow resistance in the vessels supplying leiomyomas depends not only on their size but also on their location in the uterus. The blood flow characteristics of leiomyoma-feeding vessels show significant differences between the vessels of subserous, intramural, and submucous leiomyomas. The low resistance found in subserous leiomyomas can be attributed to the fact that blood vessels are distributed to these tumors over a very small area (Fig. 4.8). These vessels are surrounded by loose connective tissue and are therefore dilated with very little resistance to flow. This contrasts with the higher-resistance vessels that supply submucous and intramural leiomyomas. The high basal tonus of the myometrium, which surrounds intramural and submucous leiomyomas, could account for the difference in hemodynamic parameters. Fig. 4.9 A submucous leiomyoma completely fills the uterine cavity. Visualized by 3 D ultrasound. Three-dimensional ultrasound is most accurate for defining the spatial relationship between submucous leiomyomas and the uterine cavity (Fig. 4.9). Kurjak et al.32 performed transvaginal color-flow Doppler examinations in 101 patients with palpable uterine leiomyomas and in 60 healthy women. The mean RI measured at the periphery of the leiomyomas was 0.54, and the mean PI was 0.89. Histopathological examination confirmed benign uterine tumors in all cases, even when the RI was very low. Low RI values were found in cases with necrotic, degenerative, or inflammatory changes within the leiomyoma. Increased blood flow velocity and a decreased RI (mean RI = 0.74) were found in both uterine arteries of the leiomyoma patients. Adenomyosis, characterized by the ingrowth of endometrial tissue into the myometrium, is usually asymptomatic but may be associated with uterine bleeding, pain, and infertility. At ultrasound, a diffusely enlarged uterus with no signs of leiomyomas and an intact endometrium should suggest the possibility of adenomyosis9. Occasionally the middle layers of the myometrium may show altered echogenicity in severe cases. Numerous small cysts have also been described within the myometrium as an expression of adenomyosis47. The sensitivity and specificity of transvaginal sonography in the detection of this benign condition are 86% and 50%, respectively9. Color Doppler imaging can demonstrate increased vascularity, which is characterized chiefly by a moderate vascular resistance (Fig. 4.10). Chronic endometritis is characterized by increased echogenicity, thickness, and vascularity of the endometrium30. The most 4 frequent cause of chronic endometrial infection is tuberculosis. The active phase of the infection is associated with increased rates of ectopic pregnancy and abortion. Transvaginal sonography can demonstrate calcified pelvic lymph nodes or even small, irregular calcifications in the adnexal region as well as suggestive deformities of the uterine cavity with no prior history of abortion or curettage that would indicate intrauterine adhesions. In the acute stage of endometritis, the vascular resistance at the periphery of the endometrium is low to moderate. Once irreversible tissue destruction has occurred, no blood flow can be observed. Transvaginal scanning can demonstrate the abnormal morphology of the endometrium, making it necessary to take bacterial cultures and institute broad-spectrum antibiotic treatment. A 1- to 2-month course of conjugated estrogens should be administered for the prevention of intrauterine adhesions after endomyometritis. This treatment promotes regeneration of the endometrium, and pulsed Doppler flowmetry can confirm this response by showing a marked rise of end-diastolic blood flow velocity in the spiral arteries. Fig. 4.10 Diffusely enlarged uterus with a thickened “Swiss cheese” endometrium shows increased vascularity (left). Doppler flow analysis (right) indicates a low blood flow velocity and moderate flow resistance (RI = 0.59).
Ultrasound Detection of Uterine Abnormalities
Congenital Anomalies
Endometrial Polyps
Submucous Leiomyomas
Adenomyosis
Endometritis
Asherman Syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree