Chapter 543 Vulvovaginitis
Etiology
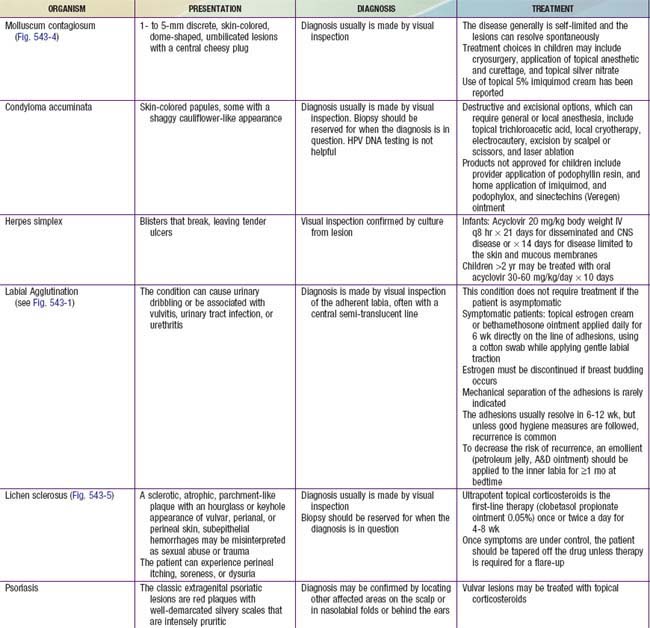
Vulvitis refers to external genital pruritus, burning, redness, or rash. Vaginitis implies inflammation of the vagina, which manifests as a discharge with or without an odor or bleeding. Vaginitis can cause vulvitis. When a child presents with vulvovaginitis, the history should include questions on hygiene (wiping from front to back) and information about possible chemical irritants (bath soaps, laundry detergents, swimming pools, or hot tubs). The caregiver can be asked about a history of diarrhea, perianal itching, or nighttime itching. The possibility of foreign objects being placed into the vagina should also be asked, although the young child is unlikely to remember or recall. Children are especially prone to nonspecific vulvovaginitis for a variety of reasons, including their nonestrogenized state, poor perianal hygiene, and the proximity of the anus to the vagina, which is without geographic barriers given the flattened labia and lack of pubic hair. Labial adhesions occur under similar conditions (Fig. 543-1 and Table 543-1).
Epidemiology
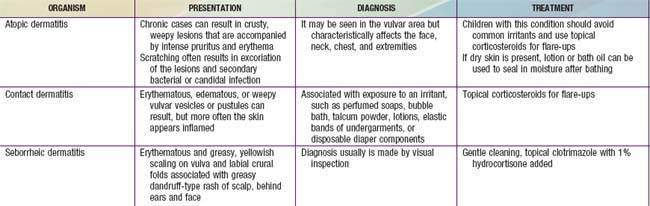
Infectious vulvovaginitis, where a specific pathogen is isolated as the cause of symptoms, may be caused by fecal or respiratory pathogens, and cultures might reveal Escherichia coli (Chapter 192), Streptococcus pyogenes, Staphylococcus aureus (Chapter 174), Haemophilus influenzae (Chapter 186), and, rarely, Candida spp. (Chapter 226). These organisms may be transmitted by the child using improper toilet hygiene and manually from the nasopharynx to the vagina. The children present with perianal redness, an inflamed introitus, and often a yellow-green or mildly bloody discharge. They may be observed to be grabbing their genital area or “digging” in their underwear, which is usually stained with yellow-brown discharge. Attempts to treat these bacterial etiologies with antifungal medication will fail; Table 543-2 gives specific recommendations.
Table 543-2 ANTIBIOTIC RECOMMENDATIONS FOR SPECIFIC VULVOVAGINAL INFECTIONS