Chapter 112 Adolescent Pregnancy
Epidemiology
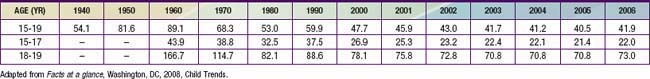
Before 2006, adolescent birthrates in the USA had steadily decreased since the early 1990s for all ages, races, and ethnic groups (Table 112-1), with the most dramatic decreases noted in African-American teens. In spite of the 3% increase from 2005 to 2006, the 2006 birthrate for teens ages 15-19 yr is considerably lower than the 1991 rate of 61.8. Pregnancy rates, which include births, miscarriages, stillbirths, and induced abortions, also decreased during this time frame, indicating that the decline in birthrates was not due to an increase in pregnancy terminations. The improvement in U.S. teen birthrates is attributed to 3 factors: more teens are delaying the onset of sexual intercourse, more teens are using some form of contraception when they begin to have sexual intercourse, and there is increased use of the new, long-lasting hormonal contraceptives.
Diagnosis (Table 112-2)
Table 112-2 DIAGNOSIS OF PREGNANCY DATED FROM FIRST DAY OF LAST MENSTRUAL CYCLE
CLASSIC SYMPTOMS
Missed menses, breast tenderness, nipple sensitivity, nausea, vomiting, fatigue, abdominal and back pain, weight gain, urinary frequency
Teens may present with unrelated symptoms that enable them to visit the doctor and maintain confidentiality
LABORATORY DIAGNOSIS
Tests for human chorionic gonadotropin in urine or blood may be positive 7-10 days after fertilization, depending on sensitivity
Irregular menses make ovulation/fertilization difficult to predict. Home pregnancy tests have a high error rate.
PHYSICAL CHANGES
2-3 wk after implantation: cervical softening and cyanosis
8 wk: uterus size of orange
12 wk: uterus size of grapefruit and palpable suprapubically
20 wk: uterus at umbilicus
If physical findings are not consistent with dates, ultrasound will confirm