Chapter 642 Vascular Disorders
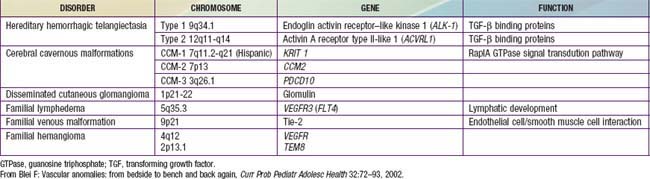
Vascular lesions of childhood may be divided into vascular birthmarks (malformations and tumors), benign acquired disorders, and genetic diseases. Familial disorders may involve arterial, capillary, lymph, or venous malformations (Table 642-1).
Vascular Malformation
Vascular malformations are developmental errors in blood vessel formation. Malformations do not regress but slowly enlarge. They should be named after the predominant blood vessel forming the lesion (Table 642-2). Table 642-3 helps differentiate vascular malformations from true hemangiomas.
Table 642-2 VASCULAR MALFORMATIONS
| TYPE | EXAMPLE(S) |
|---|---|
| Capillary | Port-wine stain |
| Venous | Venous malformation |
| Angiokeratoma circumscriptum (hyperkeratotic venule) | |
| Cutis marmorata telangiectasia congenita (congenital phlebectasia) | |
| Arterial | Arteriovenous malformation |
| Lymphatic | Superficial lymphatic malformation (lymphangioma circumscriptum) |
| Deep lymphatic malformation with macrocysts and/or microcysts (cystic hygroma) |
Table 642-3 MAJOR DIFFERENCES BETWEEN HEMANGIOMAS AND VASCULAR MALFORMATIONS
| HEMANGIOMAS | VASCULAR MALFORMATIONS (CAPILLARY, VENOUS, LYMPHATIC, ARTERIAL, AND ARTERIOVENOUS, PURE, OR COMPLEX-COMBINED) | |
|---|---|---|
| Clinical | Variably visible at birth | Usually visible at birth (AVMs may be quiescent) |
| Subsequent rapid growth | Growth proportionate to the skin’s growth (or slow progression); present lifelong | |
| Slow, spontaneous involution | ||
| Sex ratio F:M | 3 : 1 to 5 : 1; 7 : 1 in severe cases | 1 : 1 |
| Pathology | Proliferating stage: hyperplasia of endothelial cells and smooth muscle cell actin–positive cells | Flat endothelium |
| Multilaminated basement membrane | Thin basement membrane | |
| Higher mast cell content in involution | Often irregularly attenuated walls (VM, LM) | |
| Radiology | Fast-flow lesion on Doppler sonography | Slow flow (CM, LM, VM) or fast flow (AVM) on Doppler ultrasonography |
| Tumoral mass with flow voids on MRI | MRI: Hyperintense signal on T2-weighted images when slow-flow (LM, VM); flow voids on T1- and T2-weighted images when fast-flow (AVM) | |
| Lobular tumor on arteriogram | Arteriography of AVM demonstrates AV shunting | |
| Bone changes | Rarely mass effect with distortion but no invasion | Slow-flow VM: distortion of bones, thinning, underdevelopment |
| Slow-flow CM: hypertrophy | ||
| Slow-flow LM: distortion, hypertrophy, and invasion of bones | ||
| High-flow AVM: destruction, rarely extensive lytic lesions | ||
| Combined malformations (e.g., slow-flow [capillary lymphatic venous malformation, Klippel-Trenaunay syndrome] or fast-flow [capillary arteriovenous malformation Parkes-Weber syndrome]): overgrowth of limb bones, gigantism | ||
| Immunohistochemistry on tissue samples | Proliferating hemangioma: high expression of PCNA, type IV collagenase, VEGF, urokinase, and bFGF, Glucose transporter-1 | |
| Involuting hemangioma: high levels of tissue inhibitor of metalloproteinase-1, bFGF | ||
| Hematology | No coagulopathy (Kasabach-Merritt syndrome is a complication of other vascular tumors of infancy, e.g., kaposiform hemangioendothelioma and tufted angioma) | Slow-flow VM, LM, or LVM may have an associated localized intravascular coagulopathy with risk of bleeding (disseminated intravascular coagulation) |
AVM, Arteriovenous malformation; bFGF, basic fibroblast growth factor; CM, capillary malformation/port-wine stain; LM, lymphatic malformation; LVM, lymphovenous malformation; PCNA, proliferating cell nuclear antigen; VEGF, vascular endothelial growth factor; VM, venous malformation.
From Eichenfield LF, Frieden IJ, Esterly NB: Textbook of neonatal dermatology, Philadelphia, 2001, WB Saunders, p 337.
Capillary Malformation (Port-Wine Stain)
Port-wine stains are present at birth. These vascular malformations consist of mature dilated dermal capillaries. The lesions are macular, sharply circumscribed, pink to purple, and tremendously varied in size (Fig. 642-1). The head and neck region is the most common site of predilection; most lesions are unilateral. The mucous membranes can be involved. As a child matures into adulthood, the port-wine stain may become darker in color and pebbly in consistency; it may occasionally develop elevated areas that bleed spontaneously.
True port-wine stains should be distinguished from the most common vascular malformation, the salmon patch of neonates, which, in contrast, is a relatively transient lesion (Chapter 639). When a port-wine stain is localized to the trigeminal area of the face, specifically around the eyelids, the diagnosis of Sturge-Weber syndrome (glaucoma, leptomeningeal venous angioma, seizures, hemiparesis contralateral to the facial lesion, intracranial calcification) must be considered (Chapter 589.3). Early screening for glaucoma is important to prevent additional damage to the eye. Port-wine stains also occur as a component of Klippel-Trenaunay syndrome and with moderate frequency in other syndromes, including Cobb (spinal arteriovenous malformation, port-wine stain), Proteus, Beckwith-Wiedemann, and Bonnet-Dechaume-Blanc syndromes. In the absence of associated anomalies, morbidity from these lesions may include a poor self-image, hypertrophy of underlying structures, and traumatic bleeding.
Venous Malformation
Malformations consisting of veins only run the gamut from nodules containing a mass of venules (Fig. 642-2) to diffuse large vein abnormalities that may consist of either a superficial component resembling varicose veins, deeper venous malformations, or both. Nodular venous malformations are frequently confused with hemangiomas. Venous malformations may be differentiated by their presence at birth, lack of rapid growth phase, and no tendency toward regression. The treatment of choice for superficial nodular vascular malformations is surgical excision. Treatment of larger vein malformations is at best difficult and often impossible. Percutaneous sclerotherapy with direct injection of polidocanol microfoam, with color Doppler ultrasonographic guidance, is helpful in many patients, including those with Klippel-Trenaunay syndrome.
Cutis Marmorata Telangiectatica Congenita (Congenital Phlebectasia)
Cutis marmorata telangiectatica congenita is benign vascular anomaly that represents dilatation of superficial capillaries and veins and is apparent at birth. Involved areas of skin have a reticulated red or purple hue that resembles physiologic cutis marmorata but is more pronounced and relatively unvarying (Fig. 642-3). The lesions may be restricted to a single limb and a portion of the trunk or may be more widespread. Port-wine stain may also be associated. The lesions become more pronounced during changes in environmental temperature, physical activity, or crying. In some cases, the underlying subcutaneous tissue is underdeveloped, and ulceration may occur within the reticulated bands. Rarely, defective growth of bone and other congenital abnormalities may be present. No specific therapy is indicated. Mild vascular-only cases may show gradual improvement. Adams-Oliver syndrome and cutis marmorata telangiectatica congenita–macrocephaly syndrome are rarely associated disorders.
Arteriovenous Malformation
Arteriovenous malformations (AVMs) are direct connections of artery to vein that bypass the capillary bed (Fig. 642-4). AVMs of the skin are very rare. They are diagnosed from their obvious arterial palpation. Many physicians mistakenly call all vascular malformations AVMs.
Klippel-Trenaunay and Klippel-Trenaunay-Weber Syndromes
Klippel-Trenaunay syndrome (KT) is a cutaneous vascular malformation that, in combination with bony and soft tissue hypertrophy and venous abnormalities, constitutes the triad of defects of this nonheritable disorder (Fig. 642-5). The anomaly is present at birth and usually involves a lower limb but may involve more than one as well as portions of the trunk or face. Enlargement of the soft tissues may be gradual and may involve the entire extremity, a portion of it, or selected digits. The vascular lesion most often is a capillary malformation, generally localized to the hypertrophied area. The deep venous system may be absent or hypoplastic. Venous blebs and/or vesicular lymphatic lesions may be present on the malformation’s surface. Thick-walled venous varicosities typically become apparent ipsilateral to the vascular malformation after the child begins to ambulate. If there is an associated AVM, the disorder is called Klippel-Trenaunay-Weber syndrome (KTW).

Figure 642-5 Overgrowth of the right arm and hand in and adolescent with Klippel-Trenaunay syndrome.