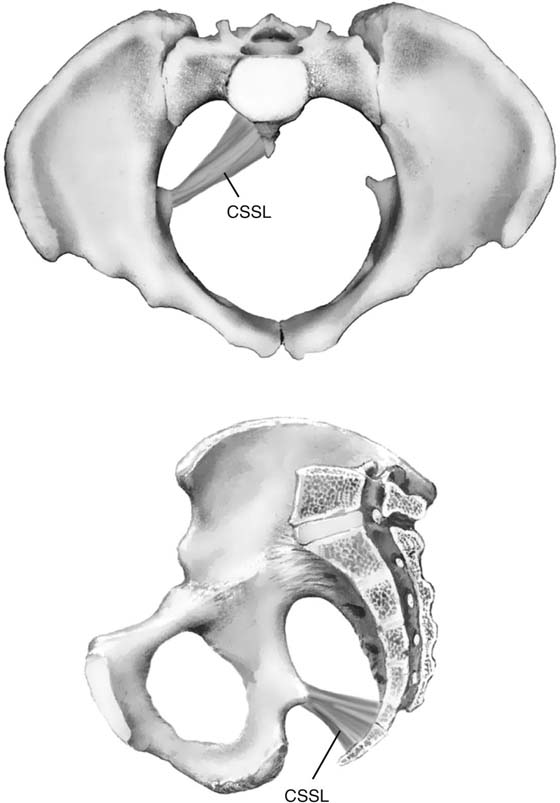
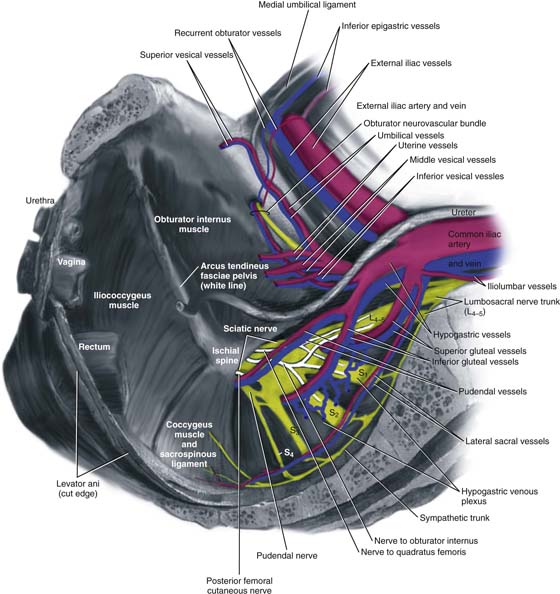
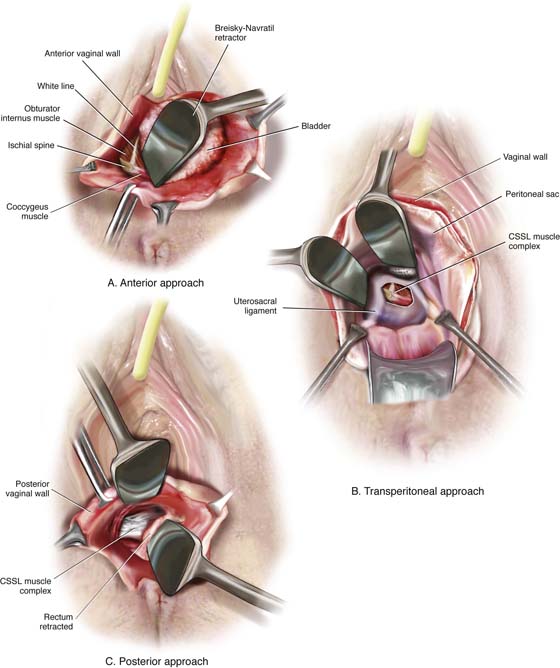
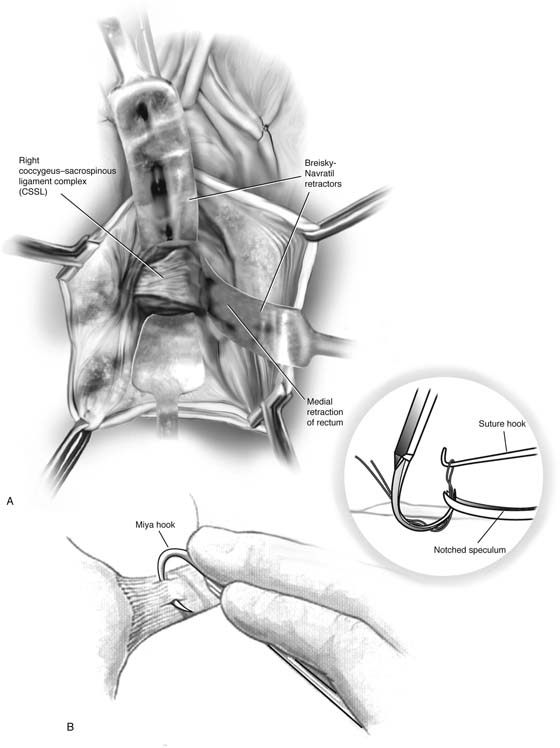
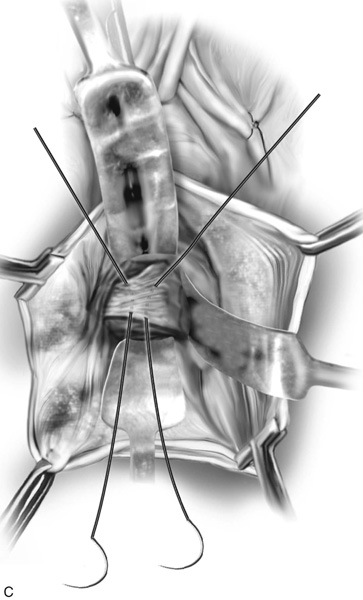
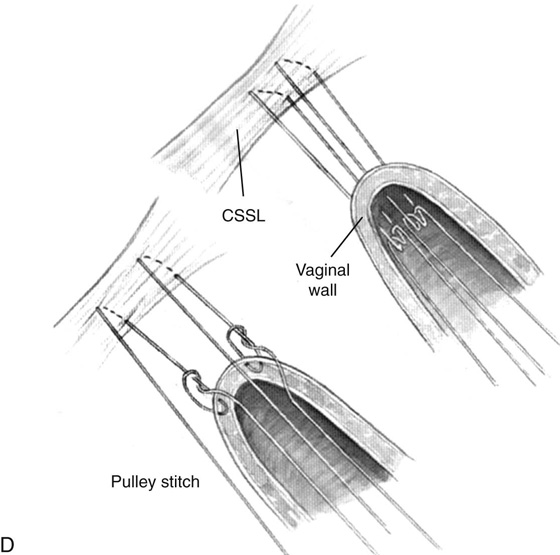
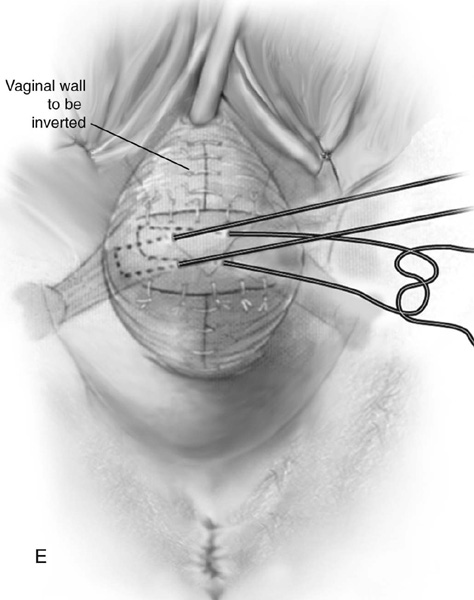
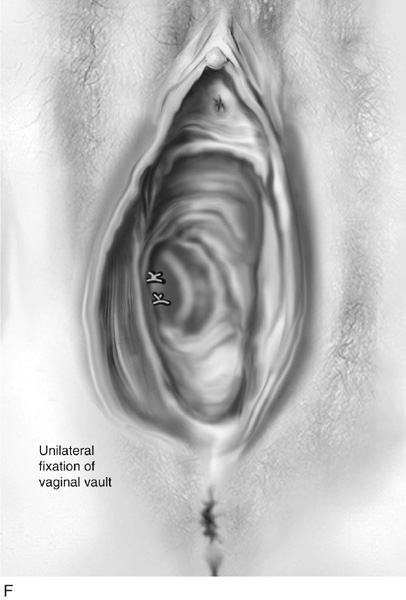
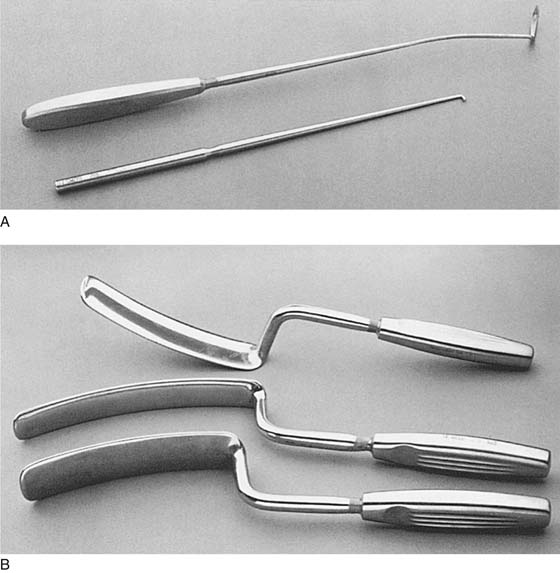
CHAPTER 55 The true incidence and prevalence of vaginal vault prolapse are unknown. Eversion of the vagina probably occurs in about 0.5% of patients who have undergone vaginal or abdominal hysterectomy. Prophylactic measures performed at the time of hysterectomy probably decrease the incidence of vaginal vault prolapse. These measures include routine reattachment of the vaginal vault to the cardinal-uterosacral ligament complex, routine use of culdoplasty sutures, and cul-de-sac obliteration or enterocele excision after removal of the uterus. When isolated uterovaginal prolapse or posthysterectomy vaginal vault prolapse is mild (i.e., the presenting part of the prolapse descends to the midportion of the vagina), vaginal hysterectomy with culdoplasty or a vaginal enterocele repair will usually be sufficient to relieve the patient’s symptoms and to restore normal vaginal function and vaginal length. However, when descent of the vault of the vagina or the uterus is significant, formal suspension of the apex of the vagina is necessary to preserve vaginal function. The vaginal procedures used to suspend the apex of the vagina discussed in this section include sacrospinous ligament suspension, iliococcygeus fascia suspension, and high uterosacral ligament suspension. To perform this procedure correctly and safely, the surgeon must be familiar with pararectal anatomy, as well as the anatomy of the sacrospinous ligament and its surrounding structures. This area at times is difficult to expose, and when vascular complications are encountered, life-threatening hemorrhage can occur. The sacrospinous ligaments extend from the ischial spine on each side to the lower portion of the sacrum and coccyx (Fig. 55–1). The ligament itself is a cordlike structure lying within the substance of the coccygeus muscle. However, the fibromuscular coccygeus muscle and the sacrospinous ligament are basically the same structure and are best referred to as the coccygeus–sacrospinous ligament complex (CSSL). The coccygeus muscle has a large fibrous component that is present throughout the body of the muscle and on its anterior surface, where it appears as white ridges. The CSSL is best identified by palpating the ischial spine and tracing the flat, triangular thickening posterior to the sacrum. The coccygeus muscle and the sacrospinous ligament are directly attached to the underlying sacrotuberous ligament. It is extremely important to appreciate the close proximity of the many vascular structures and nerves to the CSSL (Fig. 55–2). Posterior to the complex are the gluteus maximus muscle and the ischial rectal fossa. The pudendal nerves and vessels lie directly posterior to the ischial spine. The sciatic nerve lies superior and lateral. Also superiorly lies an abundant vascular supply that includes the inferior gluteal vessels and the hypogastric venous plexus (see Fig. 55–2). The CSSL complex can be exposed via posterior perirectal dissection, as well as by anterior paravaginal dissection. The ability to safely identify and palpate this structure is mandatory when a mesh prolapse kit is used (see Chapter 57). The complex also can be palpated easily transperitoneally (see Figs. 55–3 and 55–15). FIGURE 55–1 Coccygeus–sacrospinous ligament complex. Note that the sacrospinous ligament lies within the coccygeus muscle. FIGURE 55–2 Anatomy surrounding the coccygeus–sacrospinous ligament complex (CSSL). FIGURE 55–3 The sacrospinous ligament can be palpated and or exposed via the (A) anterior paravaginal approach, (B) transperitoneal approach, or (C) posterior pararectal approach. 1. With the patient in the dorsal lithotomy position, the vaginal area is prepped and draped, and prophylactic perioperative antibiotics are given on call to the operating room. 2. The apex of the vagina is grasped with two Allis clamps, and downward traction is used to determine the extent of the vaginal prolapse and associated pelvic support defects. The vaginal apex is then reduced to the sacrospinous ligament intended to be used. If bilateral sacrospinous fixation is to be performed, then each side of the vaginal apex should be reduced to the respective ligament on that side. At times, the true apex of the vagina is foreshortened and will not reach the intended area of fixation. This is commonly associated with a shortened anterior vaginal wall and a very prominent enterocele. In this setting, the apex should be moved to a portion of the vaginal wall over the enterocele, thus allowing sufficient vaginal length for suspension to the sacrospinous ligament. The intended apex is tagged with sutures for later identification. If the patient has complete eversion of the vagina that requires anterior vaginal wall repair or bladder neck suspension, the author prefers to do this portion of the operation first. During this procedure, one can separate the bladder base away from the vaginal apex, thus lowering the risk of cystotomy. 3. The upper part of the posterior vaginal wall is then incised, usually at least halfway down the length of the posterior vaginal wall. The enterocele sac is mobilized off the vaginal apex and is entered and excised. If the patient has undergone a vaginal hysterectomy, the peritoneum over the posterior vaginal wall is removed to the level of the neck of the enterocele, and the enterocele is closed as previously described. 4. The next step is entering the perirectal space. The right rectal pillar separates the rectovaginal space from the right perirectal space. The rectal pillar is nothing more than areolar tissue that extends from the rectum to the arcus tendineus fascia pelvis and overlies the levator muscle. It may contain a few small fibers and blood vessels. In most cases, entry into the perirectal space is best achieved by breaking through this fibroareolar tissue just lateral to the enterocele sac at the level of the ischial spine. This maneuver can usually be accomplished by gently mobilizing the rectum medially. At times, however, the use of gauze on the index finger or a tonsil clamp is necessary to break through into the space. 5. Once the perirectal space has been entered, the ischial spine is identified by palpation. With dorsal and medial movement of the fingers, the coccygeus sacrospinous ligament is palpated and its superior edge is identified. 6. Blunt dissection is used to further remove tissue from this area. The surgeon should take care to ensure that the rectum is adequately retracted medially. It is recommended that a rectal examination be performed at this time to ensure that no inadvertent rectal injury has occurred. Breisky-Navratil retractors are used to expose the complex (Fig. 55–4). 7. Two techniques have been popularized for the actual passage of sutures through the ligament. The first involves use of a long-handled Deschamps ligature carrier and nerve hook (Fig. 55–5A). Long straight retractors are used to expose the coccygeus muscle, ideally Breisky-Navratil retractors (Fig. 55–5B). One must take great care that the assistant does not let the tip of the retractor be pushed across the anterior surface of the sacrum, which would risk potential damage to the vessels and nerves. If the right sacrospinous ligament is to be used, the middle and index fingers of the left hand (in a right-handed surgeon) are placed on the medial surface of the ischial spine, and under direct vision, the CSSL is penetrated by the tip of the ligature carrier at a point two fingerbreadths medial to the ischial spine. When the ligature carrier is pushed through the body of the ligament, considerable resistance should be encountered. This must be overcome by forceful, yet controlled rotation of the handle of the ligature carrier. If visualization of the CSSL is difficult, the muscle and the ligament can be grasped in the tip of a long Babcock or Allis clamp, which helps to isolate the tissue to be sutured from underlying vessels and nerves. After the suture has been passed, the fingers of the left hand are withdrawn, the retractor is suitably repositioned, and the tip of the ligature carrier is visualized. The suture is then grabbed with a nerve hook. A second suture is placed similarly 1 cm medial to the first. To avoid a second passage of the ligature carrier, the original long suture can be cut in the center and each end of the cut loop paired with its respective free suture. This obtains two sutures through the ligament with only one penetration of the ligature carrier. To ensure that an appropriate bite of tissue has been obtained, one should be able to gently move the patient on the table with traction of the sutures. A second technique popularized for passing the sutures through the CSSL is the Miyazaki technique (Fig. 55–6). The proposed advantages of this technique are that it is safer and easier because the ligature carrier enters the CSSL under direct palpation of distinct landmarks and is then pulled down into the safe perirectal space below. To perform this modification, the tip of the right middle finger is placed on the CSSL just below its superior margin, approximately two fingerbreadths medial to the ischial spine. The Miya hook in the left hand in a closed position is slid along the palmar surface of the right hand. The hook point should come to rest just beneath the previously positioned tip of the right middle finger. The handles are then opened and lowered to a near horizontal position. This points the hook into the CSSL at about a 45° angle. If a high perineum prevents lowering of the handle, an episiotomy should be performed. With the tip of the middle finger, the hook point is placed two fingerbreadths medial to the ischial spine approximately 0.5 cm below the superior edge (see Fig. 55–4). With experience, the hook point can be passed along the superior edge. With the middle and index fingers, firm pressure is applied downward just behind the hook hump so that the hook point penetrates the CSSL. Downward pressure with two fingers on the tip plus traction with the back of the thumb on the back handle produces enough force to penetrate the ligament. The handle of the Miya hook is closed and elevated, and tissues from the hook point are pushed downward with the index and middle fingers so as to make the suture clearly visible. If too much tissue is in the hook, the hook is simply backed out a little, and a smaller bite taken. An assistant should hold the elevated handles in the closed position. A long retractor is then placed to mobilize the rectum medially, and a notched speculum is inserted by palpation under the hook point. A nerve hook is then used to retrieve the suture (see Fig. 55–4). FIGURE 55–4 A. Breisky-Navratil retractors are used to retract the rectum medially and the bladder superiorly. B. Technique of passage of a Miya hook through the ligament. Inset. Technique of retrieval of the suture. C. Two sutures have been passed through the complex. D. Technique of fixing the vaginal apex to the coccygeus–sacrospinous ligament complex (CSSL). If a pulley stitch is performed, then permanent sutures should be used. If the sutures are passed through the vaginal epithelium and tied in the vaginal lumen, then delayed absorbable sutures should be used. E. The vagina is closed before the suspension sutures are tied. F. Tied sacrospinous sutures. FIGURE 55–5 A. Long-handled Deschamps ligature carrier and nerve hook. Note the slight bend near the tip to facilitate suture placement into the coccygeus–sacrospinous ligament complex (CSSL). B.
Vaginal Repair of Vaginal Vault Prolapse
Sacrospinous Ligament Suspension
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Christine Vaccaro
Christine Vaccaro