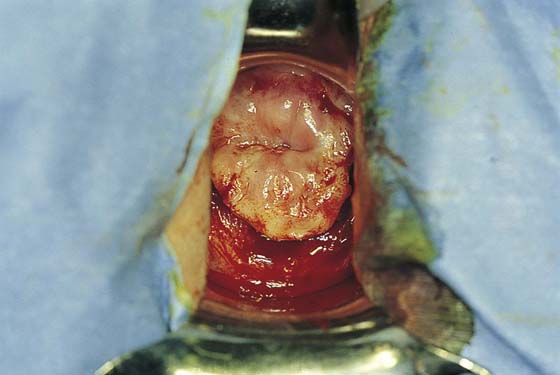
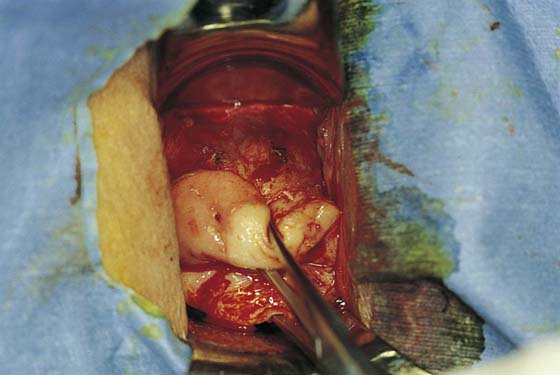
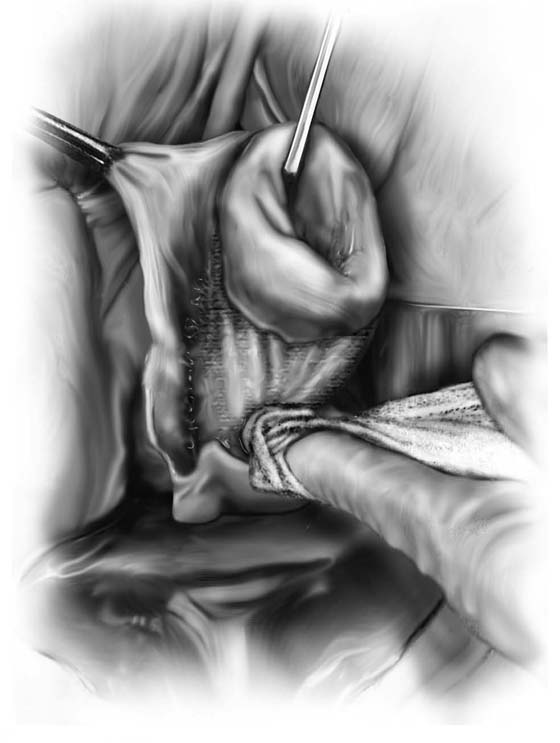
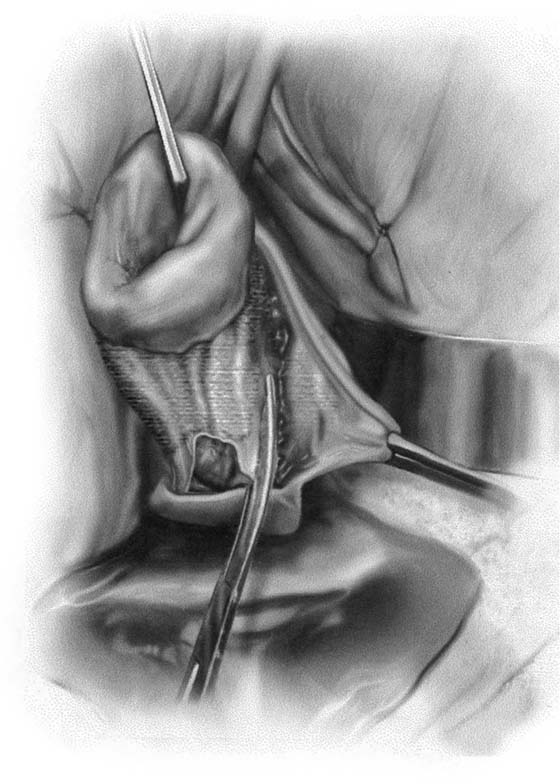
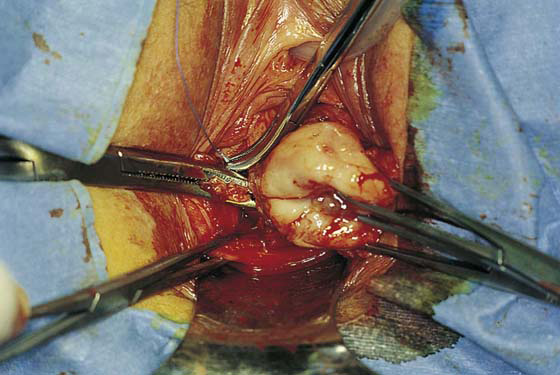
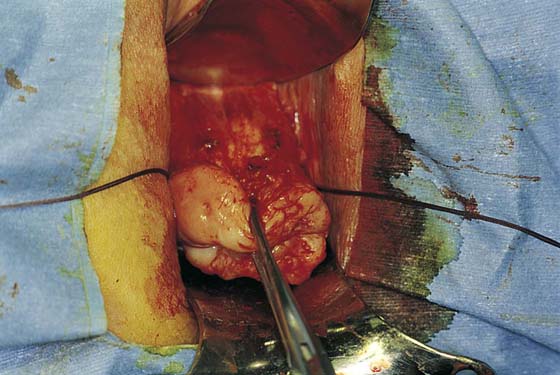
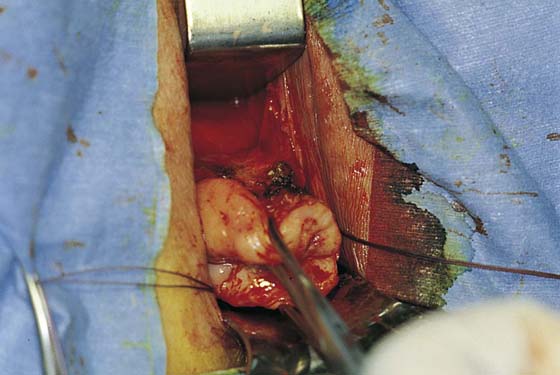
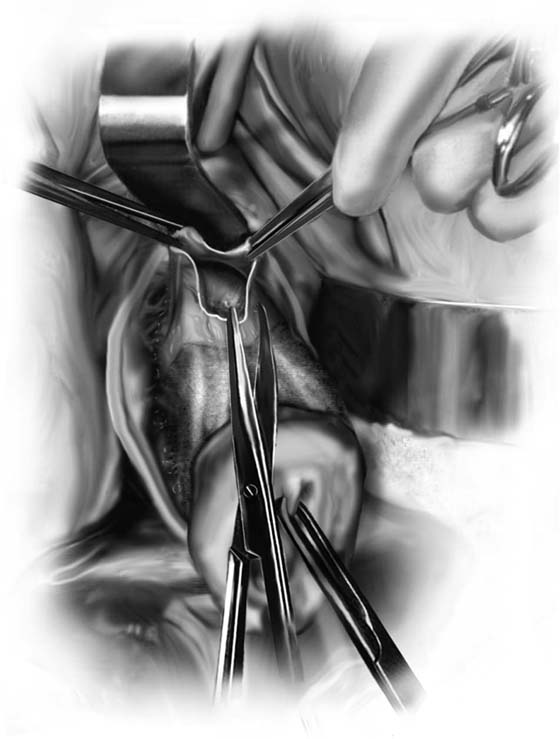
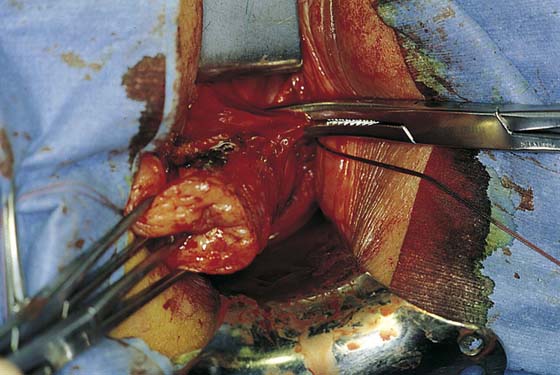
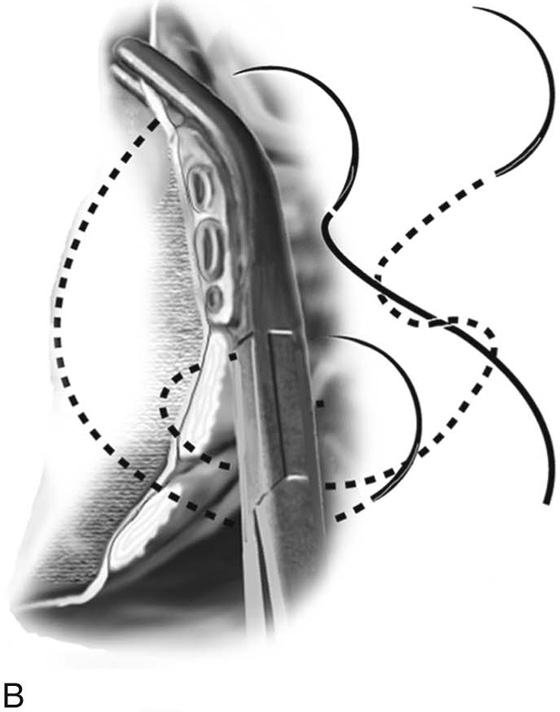
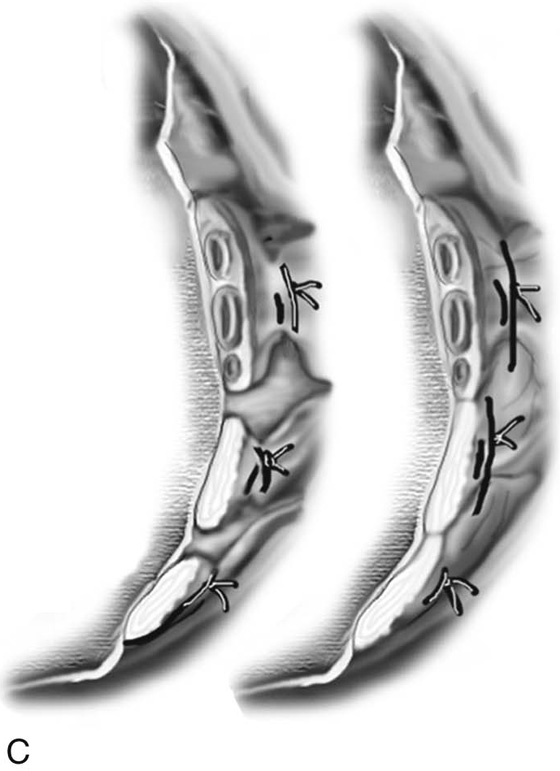
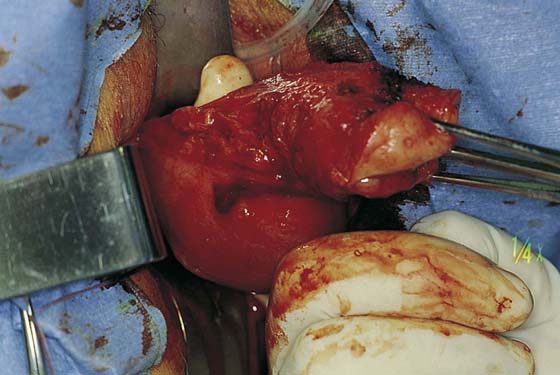
CHAPTER 53 When hysterectomy is indicated, the most appropriate route of removal of the uterus must be chosen. Hysterectomy can be performed transvaginally, abdominally, laparoscopically, or with laparoscopic assistance. The decision to proceed with a vaginal hysterectomy depends on numerous factors. These include the surgeon’s training and comfort level with the procedure, the size and mobility of the uterus, the presence of pelvic relaxation, and the benign or malignant nature of the condition. In general, vaginal hysterectomy is less morbid and results in a quicker recovery time than an abdominal or laparoscopy-assisted approach. In contrast to abdominal hysterectomy, vaginal hysterectomy is limited by the size and particularly the mobility of the uterus and by the capacity and elasticity of the vagina. Both are relative criteria because a large uterus can be morcellated, and a narrow vagina can be enlarged with an episiotomy. Vaginal hysterectomy begins with appropriate positioning of the patient. Vaginal hysterectomy is performed with the patient in the dorsal lithotomy position with her feet in “candy-cane” stirrups. The patient’s buttocks should extend slightly over the edge of the table so that a posterior retractor can be placed easily. The thighs are somewhat abducted and the hips flexed (Fig. 53–1). Excessive flexion and abduction of the thighs should be avoided, as this can lead to position-induced nerve injuries. The lateral aspects of the legs should be clear of the stirrups to avoid pressure on the peroneal nerve. The urinary bladder is then emptied with a catheter, and the vaginal area is prepped in a normal fashion. Examination under anesthesia is performed to confirm the degree of uterine descensus, the width of the vaginal outlet, and the presence or absence of pelvic pathology. 1. With a speculum depressing the posterior vaginal wall, the anterior vaginal wall is lifted with a Dever or Haney retractor. The cervix is grasped with two single-toothed tenacula, and downward traction is placed on the cervix. Vasoconstrictors such as vasopressin (Pitressin), phenylephrine (Neo-Synephrine), or epinephrine may be injected into the paracervical tissue if no medical condition, such as hypertension or heart disease, contraindicates their use. We prefer to use a prepared solution of 1% or 2% lidocaine or 0.5% bupivacaine with 1 : 200,000 epinephrine. Use of these ready-made solutions negates the need for mixing in the operating suite and provides some preemptive analgesic at the surgical site. The surgeon should remember that the maximum amount of lidocaine with epinephrine used should not exceed 7 mg/kg or 500 mg total in the healthy adult, whereas the amount of bupivacaine with epinephrine generally should not exceed 225 mg. The total dosage for vaginal hysterectomy is usually 5 to 10 mL of injection. Should a medical contraindication to the use of vasopressors be present, injectable saline provides the benefits of hydrodistention without the cardiovascular risks. A knife or electrosurgical instrument is used to make the initial incision through the vaginal mucosa (Fig. 53–2). The position and depth of this incision are very important because they determine access to appropriate planes that will lead to the anterior and posterior cul-de-sacs. The appropriate location of the incision is at the site of the bladder reflection, which is indicated by a crease formed in the vaginal mucosa when the cervix is pushed slightly inward. If this location cannot be identified, one should make the incision low rather than high to avoid potential bladder injury. A circumferential cervical incision is accomplished (Fig. 53–3). Downward traction of the tenaculum and countertraction by the retractors help to determine the appropriate depth of the incision (Fig. 53–4). The incision should be continued down to the cervical stroma. Once the appropriate depth of the incision is reached, the vaginal tissue will fall away from the underlying cervical tissue because there is a distinct plane between these two tissues (Figs. 53–5 and 53–6). 2. The vagina is mobilized both anteriorly and posteriorly. Once the appropriate plane has been reached, blunt dissection of the posterior vaginal wall will lead to the posterior cul-de-sac, which can be entered sharply (Figs. 53–7 and 53–8). Once the peritoneum has been entered, the posterior cul-de-sac is explored for adhesive disease or any other potential abnormalities that may lead to difficulty in performing the hysterectomy. A Haney or weighted retractor is then placed in the posterior cul-de-sac. 3. The uterus is pulled outward and somewhat to the opposite side. Half of an open Haney or similar clamp is introduced into the posterior cul-de-sac, and the uterosacral ligament is clamped (Fig. 53–9). The tip of the clamp is advanced as far caudally to the cervix as possible so that the parametrium included in the clamp follows the line between the anterior and posterior incisions of the vagina (Fig. 53–10). The pedicle then is cut with heavy scissors or a scalpel. The author prefers to ligate the pedicle with an absorbable suture, usually 0 Dexon or Vicryl, with a strong needle attached to it (Fig. 53–11). At times, bleeding from the posterior vaginal cuff may be encountered. This usually can be controlled with cauterization or a running interlocking suture. The cut pedicle is suture-ligated with a transfixing-type suture in which the needle enters the upper part of the ligament pedicle just slightly beyond the end of the Haney clamp. It is withdrawn and then reintroduced into the pedicle at its midpoint. These sutures are usually tagged for later identification of the uterosacral ligaments. The author prefers to alternate clamping of pedicles on opposite sides instead of clamping up one side of the uterus and then the other. This will gradually improve uterine mobility and exposure. Sharp dissection is used to mobilize the bladder more anteriorly off the cervix (Figs. 53–12 and 53–13). There is never a benefit in rushing to enter the anterior cul-de-sac. This will only lead to inadvertent cystotomies. No attempt should be made to enter the anterior cul-de-sac until the vesicouterine space has been developed. Once the bladder has been mobilized (Fig. 53–14), the cardinal ligament is clamped on each side (Fig. 53–15). This pedicle, which should include peritoneal tissue posteriorly, is sutured in a similar fashion to the uterosacral ligaments. However, the second pass through the ligament is actually made through the previous pedicle, thus obliterating any dead space between the two pedicles to decrease the potential for bleeding or tearing of tissue. FIGURE 53–1 Proper positioning of the patient in high “candy-cane” stirrups in preparation for vaginal hysterectomy. FIGURE 53–2 The initial incision begins circumferentially at the reflection of the vaginal mucosa onto the cervix. A scalpel or electrosurgical instrument can be utilized. FIGURE 53–3 The circumferential incision has been made around the cervix. FIGURE 53–4 The appropriate depth of the initial incision is demonstrated on the anterior cervix. FIGURE 53–5 Once the appropriate plane is reached, blunt dissection will usually lead to the posterior peritoneal reflection. FIGURE 53–6 Dissection of the posterior vaginal wall off the back of the cervix. FIGURE 53–7 Sharp entrance into the posterior cul-de-sac. FIGURE 53–8 The posterior cul-de-sac has been entered. FIGURE 53–9 Clamping of the right uterosacral ligament. FIGURE 53–10 A Haney clamp is used to clamp the right uterosacral ligament. FIGURE 53–11 Passage of a 0 Vicryl suture through the tip of the Haney clamp after the left uterosacral ligament has been cut. Note that the clamp should be placed as perpendicular as possible to the cervix. FIGURE 53–12 The vagina has been mobilized off the anterior cervix. FIGURE 53–13 Sharp dissection is then needed to incise the pubocervical fascia to enter the vesicouterine space before the anterior cul-de-sac is entered. FIGURE 53–14 The vesicouterine space has been entered. This allows placement of a retractor anteriorly, which mobilizes the bladder off the anterior cervix and exposes the peritoneal reflection of the anterior cul-de-sac. FIGURE 53–15 The cardinal ligament has been clamped and cut and is being sutured. This suture will incorporate the pedicle into the previous uterosacral ligament pedicle. 4. After the cardinal ligaments have been incised, a retractor is placed in the vesicouterine space to elevate the bladder off the uterus (see Fig. 53–14). If the anterior cul-de-sac is easily accessible, it can be entered at this time (Figs. 53–16 through 53–18). The next clamp, which probably will include the uterine vessels, should incorporate the anterior and posterior peritoneal reflections if the anterior cul-de-sac has been entered (Fig. 53–19). These clamps should be placed perpendicular to the longitudinal access of the cervix, and the tips of the clamps should completely slide off the cervix to ensure no inadvertent lateral migration and to avoid excessive bleeding or ureteral injury (see Fig. 53–19). As was previously mentioned, suturing of all pedicles involves passage of the needle through the tissue at the tip of the clamp and then a second pass through the previous pedicle. This will obliterate any dead space and eliminate potential bleeding between pedicles (Fig. 53–20). Extra care should be taken to avoid passage of the needle through a vessel because this may lead to the development of a retroperitoneal hematoma. 5. The uterus is then delivered anteriorly or posteriorly into the vagina (Fig. 53–21). The fundus is grasped with the tenaculum and pulled into the vagina. The utero-ovarian ligament is supported by the index finger on the opposite side, and a clamp is placed close to the uterus. The last pedicle usually includes the fallopian tube and the round and ovarian ligaments. At times, these may be taken with one clamp, but usually a clamp placed from below is required, as well as a clamp placed from above (Fig. 53–22). A finger should be maintained behind this pedicle to ensure that the clamps overlap posteriorly, and that no other tissue has been included in the clamp (Figs. 53–22 through 53–24). Once the final pedicles have been cut, the uterus is handed off to be sent to pathology. These pedicles are then doubly ligated. If one clamp has been used, a free tie is initially placed, followed by a suture-ligature. If two clamps have been used, each pedicle is individually ligated, and then a figure-of-8 suture is placed through both pedicles. These sutures are tagged, and at this time all pedicles are inspected to ensure hemostasis (Fig. 53–25). Because all pedicles have been sutured into the previous pedicle, no tearing or dead space between the pedicles should be noted (see Fig. 53–25). FIGURE 53–16 After the vesicouterine space has been entered, the anterior peritoneal reflection is usually easily accessible. FIGURE 53–17 Sharp dissection into the anterior cul-de-sac. FIGURE 53–18 The anterior cul-de-sac has been entered. FIGURE 53–19 Clamping of the uterine vessels. The clamp incorporates the peritoneal reflections of the anterior and posterior cul-de-sac. Note the placement of the clamp at a right angle to the cervix. FIGURE 53–20 A. The proper technique for clamping of the uterine vessels. B. The pedicle is sutured to ligate the vessels, as well as to incorporate the pedicle into the previously ligated pedicle. A suture is initially passed through the tissue at the tip of the clamp, and then a second pass of the needle is made through the distal end of the previous pedicle. C. This technique of ligating pedicles completely obliterates the dead space between pedicles. This technique is contrasted with the technique of ligating each pedicle individually, which results in gaps between pedicles that may lead to tearing of tissue with bleeding between pedicles. FIGURE 53–21 The uterus is delivered through the posterior cul-de-sac. FIGURE 53–22
Vaginal Hysterectomy
Simple Vaginal Hysterectomy
Surgical Technique
![]()
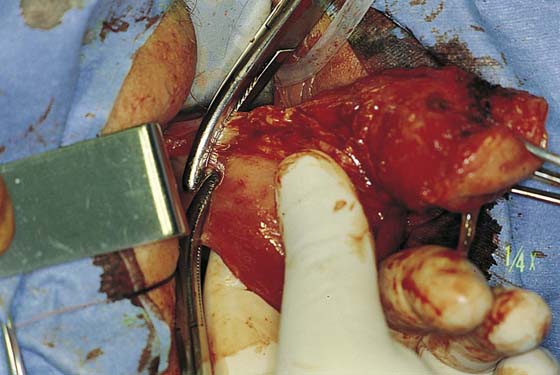
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree