Introduction
Preterm birth remains the leading cause of neonatal morbidity and mortality worldwide. The March of Dimes reports a preterm birth rate of 9.6% in the United States. Currently, the ability to identify women at risk of spontaneous preterm birth (sPTB) is limited and includes a detailed history, transvaginal ultrasound (TVU), or symptoms such as preterm contractions. We now have several interventions to decrease the risk of sPTB when at-risk women are identified, including progesterone supplementation, cerclage placement, and vaginal pessary insertion.
Mechanisms underlying sPTB are complex. Cervical tissue, composed of a matrix of collagen fibers, is supported by the cardinal and uterosacral ligaments. The cervix experiences pressures from surrounding pelvic organs and withstands forces from the growing uterus. A combination of physiologic pressures and individual anatomy affect the internal os and cervical function. Clinical cervical function can be described through cervical structure integrity as is displayed through ultrasonographic cervical length (CL) and uterocervical angle (UCA). A wide, or obtuse, UCA lends a more direct, linear outlet of uterine contents onto the cervix. A narrower, or acute, UCA supports an anatomical geometry that would exert less direct force on the internal os, which may be protective from cervical deformation.
As early as the 1950s, pessaries were thought to create an immunological barrier and mechanically change the inclination of the cervical canal, thereby distributing pelvic force away from the cervix. Altered UCA to a more acute, or narrowed, angle after vaginal pessary placement has been confirmed by magnetic resonance imaging.
Pelvic angles can be visualized and measured during TVU examination performed in pregnancy. Sochacki-Wojcicka et al suggested that angles between the uterus and cervix may be related to gestational age at delivery. In many practices, second-trimester universal TVU screening for CL is offered to identify women at increased risk of preterm birth. Our objective was to evaluate whether UCA can predict risk of sPTB in a general population of singletons and to evaluate its performance for predicting sPTB relative to CL.
Materials and Methods
This retrospective cohort study was designed to evaluate the performance of UCA measurement during routine TVU screening for CL in singleton gestations. Institutional review board approval was obtained with exemption prior to initiating the study. Consecutive women who delivered at our institution from May 1, 2014, through May 30, 2015 by university-associated practitioners were eligible. Women were identified from institutional computerized lists of deliveries by provider and date of delivery.
TVU CL screening is routinely performed in all women with singleton gestations who are scheduled for an ultrasound between 16 0/7-23 6/7 weeks’ gestation in our practice. TVU CL was performed in a uniform fashion according to CL Education and Review criteria by Registered Diagnostic Medical Sonographer–accredited sonographers monitored by maternal-fetal medicine attending staff. Transvaginal images were obtained with 4- to 9-MHz IC5-9D (Voluson e8; GE Healthcare, Milwaukee, WI) or 4- to 8-MHz C8-4v (IU22; Phillips Healthcare, Andover, MD) wide-view transducers. Images used to report CL from visits for anatomical survey studies were accessed and remeasured for UCA.
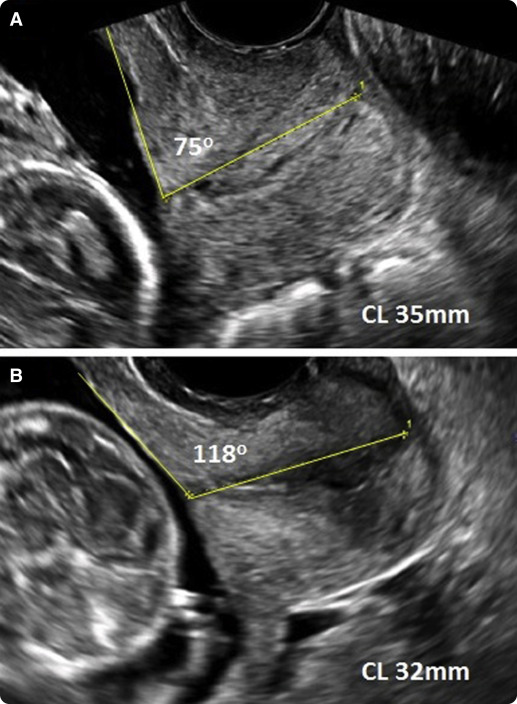
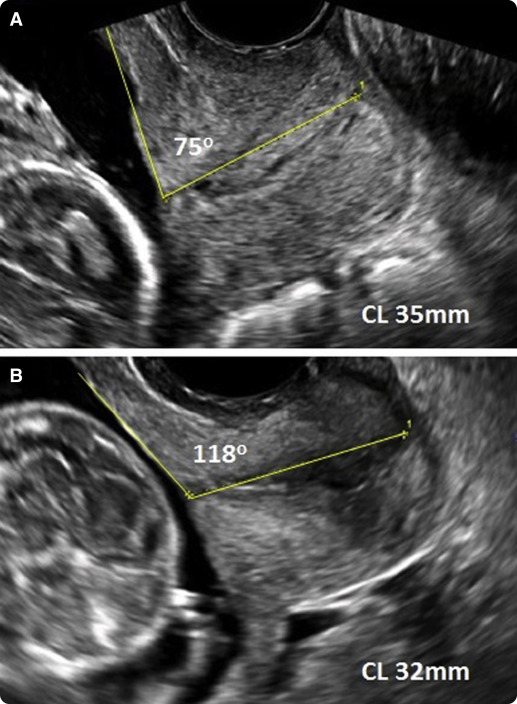
The UCA is the triangular segment measured between the lower uterine segment and the cervical canal, yielding a measurable angle ( Figure 1 ). The first ray was placed from the internal os to the external os. The calipers were placed where the anterior and posterior walls of the cervix touch the internal and external os along the endocervical canal. If the cervix was curved, the first ray was also drawn from the internal os to the external os as a straight line. A second ray was then drawn to delineate the lower uterine segment. This ray was traced up the anterior uterine segment to a distance allowed by the preloaded image. Ideally, the second ray would reach 3 cm up the lower uterine segment to establish an adequate measurement. The anterior angle between the 2 rays was measured with a protractor.
In the presence of funneling, the first ray was placed to measure the length of remaining cervix. The second caliper was placed from the innermost portion of measurable cervix and extended to the lower uterine segment. In the event that the lower uterine segment was found to be irregular, the second caliper was placed centrally along the segment. In the event of a retroverted uterus, the angle should be measured in a similar fashion with the first ray along the measurable cervix and the second ray traced along the lower uterine segment. Unlike in an anteverted or axial positioned uterus, however, the posterior side of the angle closer to the intrauterine contents should then be measured. Interobserver and intraobserver UCA measurements were compared for variability.
Women were included in the analysis if they were between the ages of 18-50 years; carrying a singleton gestation; delivered at our institution from May 1, 2014, through May 30, 2015; and had TVU CL screening images performed at our antenatal care center between 16 0/7-23 6/7 weeks. Women were excluded from the study if no TVU CL image was available for review or if an available image was considered suboptimal due to an inability to visualize landmarks defined by Iams et al, such as the lower uterine segment anteriorly or if there was excess compression of the cervix. Women were also excluded from analysis if they experienced medically indicated preterm birth. Demographic and pregnancy outcome data were collected via chart review.
Our primary outcome was the prediction of sPTB <34 and <37 weeks’ gestation by UCA measured during routine TVU for CL during the second trimester. A secondary outcome formulated prior to data collection included evaluation of sPTB predicted by TVU CL ≤25 mm. Receiver operating characteristic (ROC) curves were developed to determine an optimal UCA for prediction of sPTB at <34 and <37 weeks’ gestation. Fisher exact test, χ 2 test, Student t test, Kappa coefficient, Spearman correlation, likelihood ratios, and stepwise linear regression were performed as appropriate with P < .05 defined as significance using software (SPSS 21.0, Version 21; IBM Corp, Armonk, NY).
Materials and Methods
This retrospective cohort study was designed to evaluate the performance of UCA measurement during routine TVU screening for CL in singleton gestations. Institutional review board approval was obtained with exemption prior to initiating the study. Consecutive women who delivered at our institution from May 1, 2014, through May 30, 2015 by university-associated practitioners were eligible. Women were identified from institutional computerized lists of deliveries by provider and date of delivery.
TVU CL screening is routinely performed in all women with singleton gestations who are scheduled for an ultrasound between 16 0/7-23 6/7 weeks’ gestation in our practice. TVU CL was performed in a uniform fashion according to CL Education and Review criteria by Registered Diagnostic Medical Sonographer–accredited sonographers monitored by maternal-fetal medicine attending staff. Transvaginal images were obtained with 4- to 9-MHz IC5-9D (Voluson e8; GE Healthcare, Milwaukee, WI) or 4- to 8-MHz C8-4v (IU22; Phillips Healthcare, Andover, MD) wide-view transducers. Images used to report CL from visits for anatomical survey studies were accessed and remeasured for UCA.
The UCA is the triangular segment measured between the lower uterine segment and the cervical canal, yielding a measurable angle ( Figure 1 ). The first ray was placed from the internal os to the external os. The calipers were placed where the anterior and posterior walls of the cervix touch the internal and external os along the endocervical canal. If the cervix was curved, the first ray was also drawn from the internal os to the external os as a straight line. A second ray was then drawn to delineate the lower uterine segment. This ray was traced up the anterior uterine segment to a distance allowed by the preloaded image. Ideally, the second ray would reach 3 cm up the lower uterine segment to establish an adequate measurement. The anterior angle between the 2 rays was measured with a protractor.
In the presence of funneling, the first ray was placed to measure the length of remaining cervix. The second caliper was placed from the innermost portion of measurable cervix and extended to the lower uterine segment. In the event that the lower uterine segment was found to be irregular, the second caliper was placed centrally along the segment. In the event of a retroverted uterus, the angle should be measured in a similar fashion with the first ray along the measurable cervix and the second ray traced along the lower uterine segment. Unlike in an anteverted or axial positioned uterus, however, the posterior side of the angle closer to the intrauterine contents should then be measured. Interobserver and intraobserver UCA measurements were compared for variability.
Women were included in the analysis if they were between the ages of 18-50 years; carrying a singleton gestation; delivered at our institution from May 1, 2014, through May 30, 2015; and had TVU CL screening images performed at our antenatal care center between 16 0/7-23 6/7 weeks. Women were excluded from the study if no TVU CL image was available for review or if an available image was considered suboptimal due to an inability to visualize landmarks defined by Iams et al, such as the lower uterine segment anteriorly or if there was excess compression of the cervix. Women were also excluded from analysis if they experienced medically indicated preterm birth. Demographic and pregnancy outcome data were collected via chart review.
Our primary outcome was the prediction of sPTB <34 and <37 weeks’ gestation by UCA measured during routine TVU for CL during the second trimester. A secondary outcome formulated prior to data collection included evaluation of sPTB predicted by TVU CL ≤25 mm. Receiver operating characteristic (ROC) curves were developed to determine an optimal UCA for prediction of sPTB at <34 and <37 weeks’ gestation. Fisher exact test, χ 2 test, Student t test, Kappa coefficient, Spearman correlation, likelihood ratios, and stepwise linear regression were performed as appropriate with P < .05 defined as significance using software (SPSS 21.0, Version 21; IBM Corp, Armonk, NY).
Results
A total of 1109 women were eligible for inclusion during the study period. After 137 (12%) women were excluded, 115 for lack of adequate TVU image availability and 22 due to medically indicated preterm birth, 972 (88%) women remained for inclusion. The Kappa coefficient was 0.94 for masked interobserver variability and 0.90 for masked intraobserver variability, both evident of strong agreement between measured UCA.
The rate of sPTB <37 weeks was 9.6% (n = 84) and 4.5% (n = 43) at <34 weeks. Women who delivered preterm were similar to those who delivered ≥37 weeks with respect to age, race, nulliparity, mode of conception, smoking, cervical procedures, maternal diabetes, and maternal hypertension. However, compared with women who delivered ≥37 weeks, women who delivered preterm were more likely to have had a prior sPTB, a history of dilation and curettage, a shorter CL in the second trimester, a higher body mass index, and a cesarean delivery ( Table 1 ).
| Demographic | Birth ≥37 wk n = 888 [91.4%] | Birth <37 wk n = 84 [8.6%] | P value |
|---|---|---|---|
| Mean maternal age, y | 33 (±5) | 33 (±5) | 1 |
| Race/ethnicity | .41 | ||
| White | 615 (69) | 54 (64) | |
| Non-white | 273 (31) | 30 (36) | |
| Nulliparous | 548 (62) | 50 (60) | .77 |
| Prior spontaneous preterm birth | 58 (6.5) | 13 (16) | .005 |
| Natural conception | 785 (88) | 73 (87) | .82 |
| Tobacco use | 6 (0.6) | 1 (1) | .46 |
| Prior dilation and curettage | 165 (19) | 25 (30) | .01 |
| Prior cervical conization | 6 (0.7) | 2 (2.4) | .14 |
| Prior cervical LEEP | 47 (5.3) | 4 (4.8) | .54 |
| Abnormal pap smear | 207 (23) | 17 (20) | .61 |
| Mean gestational age at TVU, wk | 20 (±3) | 21 (±3) | <.001 |
| Mean CL at TVU, cm | 40 (±7) | 36 (±9) | <.001 |
| Mean UCA at TVU | 93 (±26) | 120 (±27) | <.001 |
| Mean body mass index at conception, kg/m 2 | 24 (±5) | 26 (±5) | <.001 |
| Mean body mass index at delivery, kg/m 2 | 29 (±13) | 33 (±30) | .04 |
| Diabetes | 59 (6) | 10 (12) | .11 |
| Hypertensive disorder | 115 (13) | 13 (15) | .62 |
| Cesarean delivery, primary | 295 (33) | 45 (54) | <.001 |
| Cesarean delivery, repeat | 56 (6.5) | 8 (9) | .36 |
| Mean gestational age at delivery | 39 (±2.5) | 33 (±4) | <.001 |
| Female fetus | 729 (48) | 38 (45) | .60 |
| NICU admission | 94 (11) | 54 (64) | <.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


