CHAPTER 10 ischemic necrosis of tubular cells; most common cause of renal failure. benign tumor composed of blood vessels, smooth muscle, and fat. cortical bulge on the lateral aspect of the kidney. fibrous connective membrane of the body that may be separate from other structures. immaturity of renal development resulting in a lobulated renal contour. protective covering of tissue surrounding each kidney. inflammation of the glomerulus of the kidney. structure composed of blood vessels or nerve fibers. hypertrophied column of Bertin enlargement of a column of Bertin that extends into the renal pyramid. embryonic remnant of the fusion site between the upper and lower poles of the kidney. blunt apex of the renal pyramid. cyst beside the renal pelvis; may obstruct the kidney. cyst around the renal pelvis; does not obstruct the kidney. sharp, severe flank pain radiating to the groin. the inability of the kidneys to excrete waste, concentrate urine, and conserve electrolytes. partial kidney function failure characterized by less than normal urine output. the functional tissue of the kidney consisting of the nephrons. excessive accumulation of fat in the renal sinus. renal enzyme that affects blood pressure. quick fluctuating color Doppler signal from a rough surface or highly reflective object. epithelial tube connecting the apex of the urinary bladder to the umbilicus. • 25 to 34 cm long tubular structure connecting the renal pelvis to the urinary bladder. • Course vertically with retroperitoneum along the psoas muscles. • Insert posterior and inferiorly at the trigone of the bladder. Support Structure of the Kidneys • Paired bean-shaped structures lying in a sagittal oblique plane in the retroperitoneal cavity. • Located between the first and third lumbar vertebrae. • Superior poles lie more posterior and medial. • Inferior poles lie more anterior and lateral. • Anterior to the psoas and quadratus lumborum muscles. • Medial to the transverse abdominis muscle and liver or spleen. Normal Sonographic Appearance—Adult Kidney Normal Sonographic Appearance—Pediatric Kidney • Kidneys—patient should be hydrated. • Renal vessels—nothing by mouth for 6 to 8 hours before the examination. • Bladder—drink 8 to 16 ounces of water 1 hour before the examination. • Use the highest-frequency abdominal transducer possible to obtain optimal resolution for penetration depth. • Place gain settings to display the normal adult renal cortex as moderate or low-level echogenicity and the renal sinus as the most echogenic with adjustments to reduce echoes within the vessels. • Position the focal zone(s) at or below the region of interest. • Sufficient imaging depth to visualize structures posterior to the region of interest. • Harmonic imaging and decreasing the compression (dynamic range) can be used to reduce artifactual echoes within anechoic structures and improve prominence of posterior acoustic shadowing. • Spatial compounding can be used to improve visualization of structures posterior to a highly attenuating structure. • Evaluation and documentation of the superior, inferior, medial, and lateral aspects of each kidney in the coronal or sagittal plane. • Evaluation and documentation of the superior pole, renal hilum, and inferior pole of each kidney in the transverse plane. • Measurements of maximum length, thickness, and width of each kidney. • Measurement of the cortical thickness of each kidney. • Evaluation and documentation of the bladder wall. • Prevoid and postvoid bladder volumes may be included. • Kidneys are best evaluated with an empty urinary bladder. • Documentation and measurement of any abnormality in two scanning planes with and without color Doppler should be included. • A waste product produced from meat protein and normal wear and tear on the muscles in the body. • More specific in determining renal dysfunction than BUN levels. • Elevated in renal failure, chronic nephritis, or urinary obstruction.
Urinary system
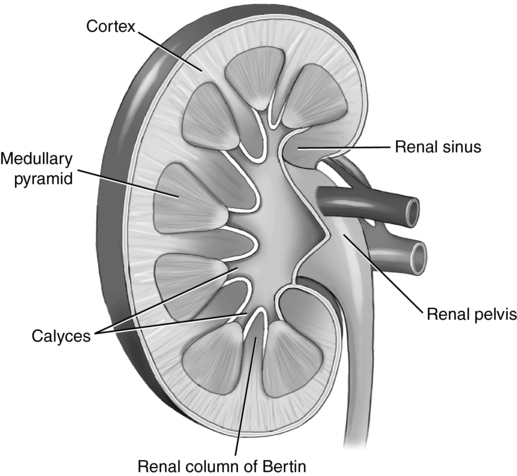
Anatomy
ANATOMY
DESCRIPTION
Renal capsule
Fibrous capsule (true capsule) surrounding the cortex
Renal cortex
Outer portion of the kidney
Bound by the renal capsule and arcuate vessels
Contains glomerular capsules and convoluted tubules
Medulla
Inner portion of the renal parenchyma
Within the medulla lie the renal pyramids
Renal pyramids contain tubules and the loops of Henle
Column of Bertin
Inward extension of the renal cortex between the renal pyramids
Renal sinus
Central portion of the kidney
Contains the major and minor calyces, peripelvic fat, fibrous tissues, arteries, veins, lymphatics, and part of the renal pelvis
Renal hilum
Contains the renal artery, renal vein, and ureter
RENAL VESSEL
DESCRIPTION
Main Renal Artery
The right renal artery arises from the anterolateral aspect of the aorta; the left renal artery arises from the posterolateral aspect of the aorta
May have multiple ipsilateral arteries
A single ipsilateral artery may divide into multiple renal arteries at the hilum
Courses posterior to the renal vein
Main renal artery arises 1.0-1.5 cm inferior to the origin of the superior mesenteric artery
Right renal artery is longer than the left renal artery
Demonstrates low-resistance blood flow
Supplies the kidney, ureter, and adrenal gland
Segmental artery
After entering the renal hilum, the artery divides into 4 to 5 segmental arteries
Demonstrates low-resistance blood flow
Interlobar artery
Branch of the segmental artery
Course alongside the renal pyramids
Demonstrates low-resistance blood flow
Arcuate artery
Boundary between the cortex and medulla
Branch of the interlobar artery located at the base of the medulla
Arcuate arteries give rise to the interlobular arteries
Demonstrates low-resistance blood flow
Interlobular artery
Branch of the arcuate arteries entering the renal glomeruli
Main Renal Vein
Formed from the junction of tributaries in the renal hilum
Courses anterior to the renal artery
Left renal vein receives the left suprarenal and left gonadal vein
Left renal vein is longer than the right renal vein
Dilatation of the left renal vein, caused by mesenteric compression, may be demonstrated
Ureter anatomy
Arterial supply to the ureter
Psoas muscle
Major groin muscle
Primary flexor of the hip joint
Lies posterior to the inferior pole of each kidney
Quadratus lumborum muscle
Muscle of the posterior abdominal wall
Lies posterior and medial to each kidney
Transversus abdominis muscle
Deepest layer of flat muscles of the anterolateral wall
Lies lateral to each kidney
Gerota’s fascia
Fibrous covering of tissue surrounding each kidney
Also known as Gerota’s capsule; renal fascia
Perinephric fat
Fatty tissue surrounding each kidney
Renal capsule
Protective connective tissue capsule surrounding each kidney
Location
Each kidney is located
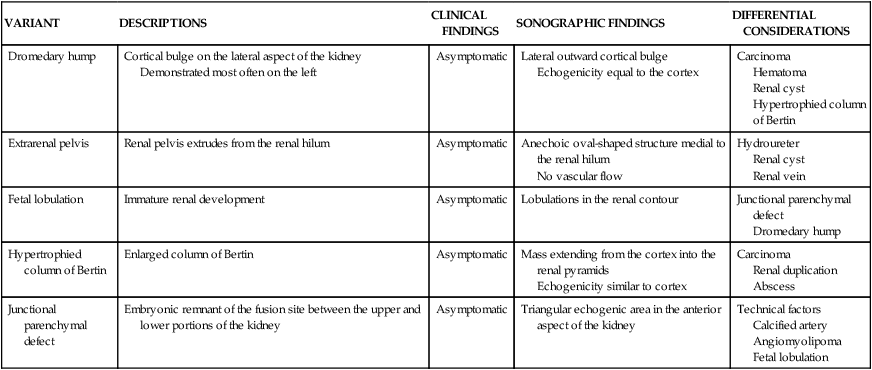
VARIANT
DESCRIPTIONS
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Dromedary hump
Cortical bulge on the lateral aspect of the kidney
Demonstrated most often on the left
Asymptomatic
Lateral outward cortical bulge
Echogenicity equal to the cortex
Carcinoma
Hematoma
Renal cyst
Hypertrophied column of Bertin
Extrarenal pelvis
Renal pelvis extrudes from the renal hilum
Asymptomatic
Anechoic oval-shaped structure medial to the renal hilum
No vascular flow
Hydroureter
Renal cyst
Renal vein
Fetal lobulation
Immature renal development
Asymptomatic
Lobulations in the renal contour
Junctional parenchymal defect
Dromedary hump
Hypertrophied column of Bertin
Enlarged column of Bertin
Asymptomatic
Mass extending from the cortex into the renal pyramids
Echogenicity similar to cortex
Carcinoma
Renal duplication
Abscess
Junctional parenchymal defect
Embryonic remnant of the fusion site between the upper and lower portions of the kidney
Asymptomatic
Triangular echogenic area in the anterior aspect of the kidney
Technical factors
Calcified artery
Angiomyolipoma
Fetal lobulation
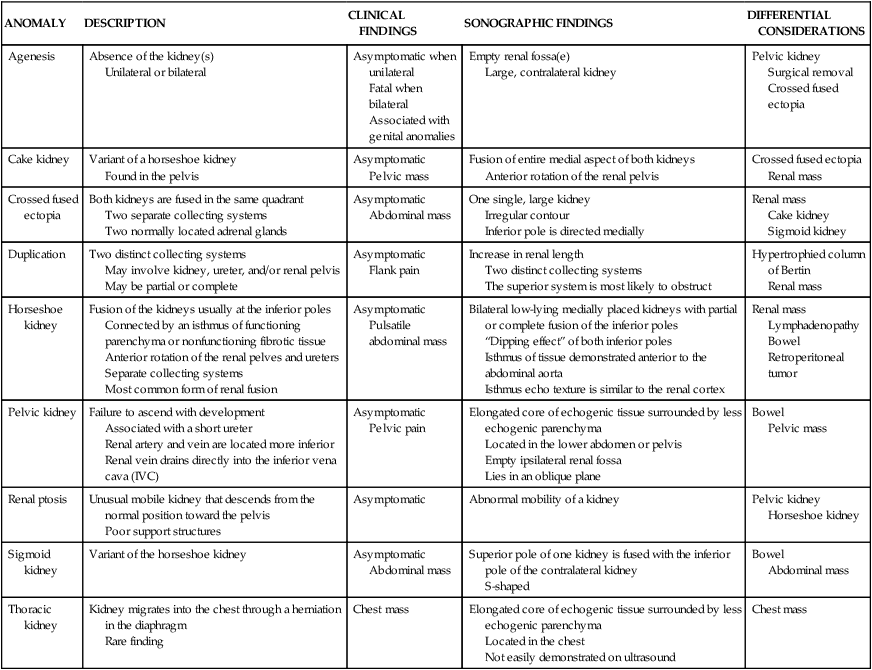
ANOMALY
DESCRIPTION
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Agenesis
Absence of the kidney(s)
Unilateral or bilateral
Asymptomatic when unilateral
Fatal when bilateral
Associated with genital anomalies
Empty renal fossa(e)
Large, contralateral kidney
Pelvic kidney
Surgical removal
Crossed fused ectopia
Cake kidney
Variant of a horseshoe kidney
Found in the pelvis
Asymptomatic
Pelvic mass
Fusion of entire medial aspect of both kidneys
Anterior rotation of the renal pelvis
Crossed fused ectopia
Renal mass
Crossed fused ectopia
Both kidneys are fused in the same quadrant
Two separate collecting systems
Two normally located adrenal glands
Asymptomatic
Abdominal mass
One single, large kidney
Irregular contour
Inferior pole is directed medially
Renal mass
Cake kidney
Sigmoid kidney
Duplication
Two distinct collecting systems
May involve kidney, ureter, and/or renal pelvis
May be partial or complete
Asymptomatic
Flank pain
Increase in renal length
Two distinct collecting systems
The superior system is most likely to obstruct
Hypertrophied column of Bertin
Renal mass
Horseshoe kidney
Fusion of the kidneys usually at the inferior poles
Connected by an isthmus of functioning parenchyma or nonfunctioning fibrotic tissue
Anterior rotation of the renal pelves and ureters
Separate collecting systems
Most common form of renal fusion
Asymptomatic
Pulsatile abdominal mass
Bilateral low-lying medially placed kidneys with partial or complete fusion of the inferior poles
“Dipping effect” of both inferior poles
Isthmus of tissue demonstrated anterior to the abdominal aorta
Isthmus echo texture is similar to the renal cortex
Renal mass
Lymphadenopathy
Bowel
Retroperitoneal tumor
Pelvic kidney
Failure to ascend with development
Associated with a short ureter
Renal artery and vein are located more inferior
Renal vein drains directly into the inferior vena cava (IVC)
Asymptomatic
Pelvic pain
Elongated core of echogenic tissue surrounded by less echogenic parenchyma
Located in the lower abdomen or pelvis
Empty ipsilateral renal fossa
Lies in an oblique plane
Bowel
Pelvic mass
Renal ptosis
Unusual mobile kidney that descends from the normal position toward the pelvis
Poor support structures
Asymptomatic
Abnormal mobility of a kidney
Pelvic kidney
Horseshoe kidney
Sigmoid kidney
Variant of the horseshoe kidney
Asymptomatic
Abdominal mass
Superior pole of one kidney is fused with the inferior pole of the contralateral kidney
S-shaped
Bowel
Abdominal mass
Thoracic kidney
Kidney migrates into the chest through a herniation in the diaphragm
Rare finding
Chest mass
Elongated core of echogenic tissue surrounded by less echogenic parenchyma
Located in the chest
Not easily demonstrated on ultrasound
Chest mass
Size
Adult
Infant
DIVISION
SONOGRAPHIC APPEARANCE
Renal capsule
Well-defined echogenic line surrounding the kidney
Renal cortex
Fine, moderate, to low-level echogenicity
Less echogenic compared to the normal liver parenchyma
Medulla
Hypoechoic; may appear anechoic
Columns of Bertin
Moderate to low-level echogenicity
Renal sinus
Hyperechoic; most echogenic
Arcuate vessels
Small echogenic foci at the corticomedullary junction
Cortical thickness
Minimum 1 cm
DIVISION
SONOGRAPHIC APPEARANCE
Renal capsule
Sparse amount of perinephric fat makes it difficult to distinguish the capsule
Renal cortex
Moderate to highly echogenic
Medulla
Commonly anechoic
Do not mistake for hydronephrosis
Renal sinus
Barely visible in infants
Technique
Preparation
Examination technique and imaging optimization
PATIENT POSITION
DEMONSTRATES/BENEFITS
Supine
Right superior pole with intercostal approach
Right inferior pole with subcostal approach
Left posterior oblique (LPO)
Allows bowel to move away from right kidney
Subcostal or intercostal approach
Left lateral decubitus
Liver and kidney “fall” from the rib cage
Aids in obese or gassy patients
Right posterior oblique (RPO)
Left superior pole with intercostal approach
Posterior subcostal approach for left inferior pole
Right lateral decubitus
Left posterior approach with deep inspiration
Prone
Demonstrates mid and inferior poles of both kidneys
Great for infants and small children
Superior poles may be visualized
Used in renal biopsies
Laboratory values
Creatinine