Unilateral Small Kidney
Sara M. O’Hara, MD, FAAP
DIFFERENTIAL DIAGNOSIS
Common
Congenital Hypoplasia/Dysplasia
Scarring
Postinfectious Scarring
Postinflammatory Scarring
Obstructive Scarring
Vesicoureteral Reflux (VUR) Scarring
Post-Traumatic
Multicystic Dysplastic Kidney (MCDK)
Less Common
Page Kidney
Renal Vein Thrombosis, Chronic
Other Vascular Insult
Rare but Important
Partial Resection
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Hypoplasia, dysplasia, and scarring are all different from aplasia
Aplasia is congenital absence of renal tissue
Associated ureteral agenesis with absence of ipsilateral trigone and ureteral orifice
Contralateral hypertrophy
Seen commonly with aplasia
Less common with hypoplasia/dysplasia
Also seen following early surgical removal of 1 kidney
Hypoplastic kidney < 1/2 size of contralateral kidney
Calyces and parenchyma are normal in proportion
Architecture should be normal, not scarred or dysplastic
Just smaller version of opposite kidney
Dysplasia: Congenitally malformed parenchyma
Chronic scarring and fibrosis also sometimes called “dysplasia”
All other diagnoses are acquired, typically chronic or recurrent
Differential by location
Prerenal: Arterial stenosis, shock, infarction
Renal: Postinfectious, hypoplasia, dysplasia, MCDK, radiation
Postrenal: Obstructive or vesicoureteral reflux (VUR) atrophy
Helpful Clues for Common Diagnoses
Congenital Hypoplasia/Dysplasia
Hypoplasia results from insufficient branching of ureteric bud
Nephrons formed are normal but deficient in number
Renal parenchymal volume is diminished but does function
Segmental hypoplasia more often associated with hypertension
Hypertension refractory to medical Rx, may require surgical/ablative Rx
Segmental hypoplasia (a.k.a. Ask-Upmark kidney) may actually be segmental scar
Patients are typically female and present with hypertension
Dysplasia results from faulty formation of nephrons &/or collecting system
Renal volume may be normal or decreased initially but tends to decrease with age
Nephrons are poorly functioning or malfunctioning → salt wasting
Postinfectious Scarring
After pyelonephritis, renal abscess, sepsis
Patchy or global, affecting entire kidney
Xanthogranulomatous pyelonephritis
Chronic pyelonephritis with granulomatous abscess formation and severe kidney destruction
Controversy exists regarding
Increased scarring in infants and young children compared with older children
Increased scarring when antibiotic therapy is delayed
Prospective, randomized trials on subject are lacking
Imaging
Ultrasound: Cortical thinning, volume loss, increased echogenicity
DMSA: Absent radiotracer in areas of scar and fibrosis, often crescentic
CT & MR: Poorly enhancing, thinned cortex, lobulated contour
IVP: Seldom performed in children
Postinflammatory Scarring
May be seen after any “nephritis”
Glomerulonephritis
Radiation nephritis
Autoimmune
Henoch-Schönlein purpura
Hemolytic uremic syndrome
Scarring can affect 1 kidney asymmetrically, even when both kidneys have nephritis
Imaging shows smaller kidney, typically with global scarring
Obstructive Scarring
Scarring and nephron damage from any downstream obstruction
Ureteropelvic junction obstruction
Ureterovesical junction obstruction
Urinary calculi
Bladder outlet obstruction, posterior urethral valves
Neurogenic bladder and other voiding dysfunction
Pelvic mass or inflammation
Vesicoureteral Reflux (VUR) Scarring
Scarring has been shown with reflux, even in absence of infection
Higher grades of reflux are more likely to cause scarring
Higher grades of reflux are less likely to spontaneously resolve with age/somatic growth
Post-Traumatic
Underlying causes vary
Vascular insult, infarction, emboli, venous infarct
Obstruction to urine flow, superimposed infection
Perinephric hematoma with compressive injury
Multicystic Dysplastic Kidney (MCDK)
Severely dysplastic, nonfunctional tissue
Enlarged, normal size, or small in newborn
Over years, tissue involutes and atrophies
Recognizable only by location in teenagers
Helpful Clues for Less Common Diagnoses
Page Kidney
Hypertension and renal insufficiency caused by compression of kidney
Typically due to subcapsular hematoma, though other perinephric masses (tumor or urinoma) also possible
In 1939, Dr. Irvine H. Page (1901-89) demonstrated that wrapping cellophane tightly around animal kidneys can cause hypertension
Renal Vein Thrombosis, Chronic
Initially causes renal enlargement
Kidney atrophies over weeks to months
Seen in thrombotic conditions, premature infants with umbilical catheters, sepsis
Other Vascular Insult
Numerous other vasculitides can cause chronic scarring or atrophy of 1 kidney
Helpful Clues for Rare Diagnoses
Partial Resection
Nephron-sparing surgery continues to gain popularity
Any surgery done to remove segment of kidney results in remaining tissue being “small”
Consider partial resection when 1 renal pole appears flattened or truncated
Image Gallery
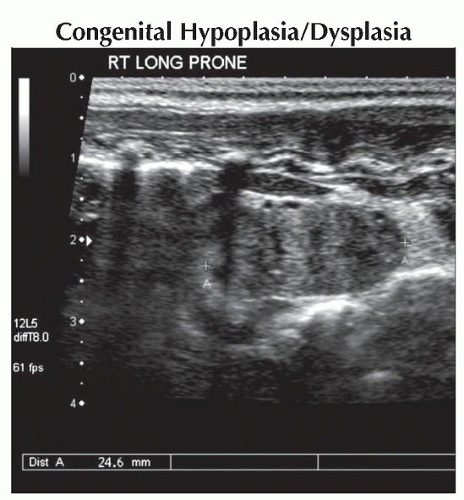 Longitudinal harmonic ultrasound shows a small, echogenic right kidney with poor corticomedullary differentiation in a newborn with a prenatal history of suspected right renal aplasia/hypoplasia. |
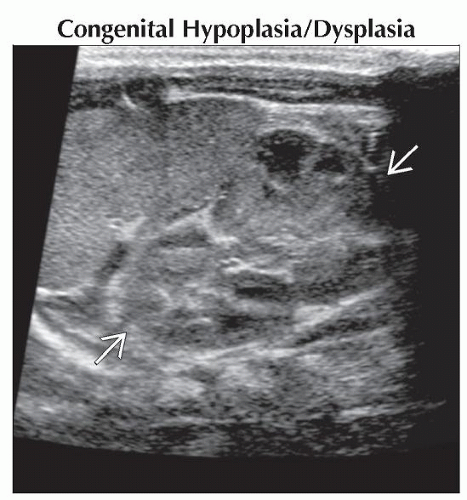 Longitudinal harmonic ultrasound shows a normal left kidney
 in the same infant. There is no compensatory hypertrophy of the left kidney at this point. in the same infant. There is no compensatory hypertrophy of the left kidney at this point.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|