Twin Related Anomalies
Anne Kennedy, MD
DIFFERENTIAL DIAGNOSIS
Common
Fetal Demise
Twin-Twin Transfusion Syndrome
Conjoined Twins
Twin Reversed Arterial Perfusion
Rare but Important
Fetus-in-Fetu
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Most important step in evaluation of multiple gestation is determination of chorionicity
Certain problems only occur in monochorionic gestation
Twin-twin transfusion syndrome (TTTS)
Twin reversed arterial perfusion (TRAP)
Conjoined twins
Assess fluid distribution
Show fluid on either side of inter-twin membrane
Measure maximum vertical pocket for each twin
If fluid is asymmetric, determine which side is abnormal
Decreased in one twin: Oligohydramnios differential
Increased in one twin: Polyhydramnios differential
Increased in one twin & decreased in the other: TTTS most likely diagnosis
Helpful Clues for Common Diagnoses
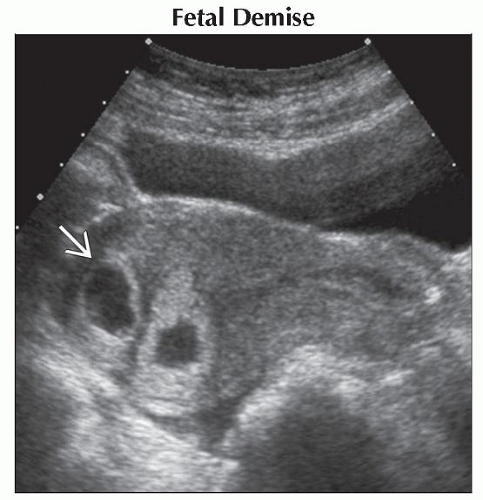
Fetal Demise
Not uncommon in early pregnancy
Cardiac activity should always be seen in an embryo > 5 mm in crown rump length
If early, sac may completely resorb → “disappearing twin”
If later in monochorionic gestation, TRAP sequence may develop
Cord entanglement is a specific cause of demise in monoamniotic twins
Twin-Twin Transfusion Syndrome
Monochorionic gestation
Asymmetric or discordant growth
Abnormal fluid distribution: One twin with oligohydramnios, one with polyhydramnios
Look for “stuck” twin with shrink-wrapped membrane in severe cases
TTTS staging
Stage 1: Donor bladder visible, normal Doppler
Stage 2: Donor bladder empty, normal Doppler
Stage 3: Donor bladder empty, abnormal Doppler
Stage 4: Hydrops in recipient
Stage 5: Demise of one or both
Conjoined Twins
Monoamniotic gestation = no inter-twin membrane
Must have contiguous skin covering between fetuses
Nomenclature
Site of attachment & “pagus” (e.g., cephalopagus)
“Di” & site of duplication (e.g., dicephalus)
Twin Reversed Arterial Perfusion
Monochorionic gestation with one normal “pump” twin and one anomalous twin
Anomalous twin
Absent cardiac activity or rudimentary heart
Often well-developed torso/lower extremities
Upper extremities/cranium poorly developed or absent
Marked skin edema ± effusions/ascites
Hallmark of this condition is umbilical artery flow toward the abnormal fetus rather than toward the placenta
Helpful Clues for Rare Diagnoses
Fetus-in-Fetu
Apparent singleton: “Twin” is incorporated into the “singleton” as a mass
Always think about this with an unusual fetal mass
Other Essential Information
Anomaly rate higher in twin than singleton pregnancies
Any anomaly/aneuploidy can occur regardless of chorionicity
Specific entities arise from vascular connections in monochorionic placentas
TTTS arises secondary to artery to vein shunt within monochorionic placenta
Donor twin shunts arterial blood into recipient twin’s venous circulation → donor oligemia → effective “hypotension”
↓ Renal perfusion → ↓ urine output → oligohydramnios
↓ Blood to placenta → ↓ return of oxygenated blood → chronic hypoxia → poor growth
Recipient twin receives all its own return from placenta & portion of co-twins → plethora/fluid overload
↑ Volume status → ↑ cardiac output → eventual development of hydrops
TRAP sequence arises secondary to artery to artery shunt within monochorionic placenta
Pump twin deoxygenated blood → co-twin umbilical arteries → preferential perfusion of lower extremities → lack of upper body/cranial development
Blood enters fetus via UA not UV → lack of normal circulation through heart → abnormal cardiac development
Alternative Differential Approaches
Twin with hydrops
Anomalous twin in TRAP sequence: Massive skin edema/effusions common
Pump twin in TRAP sequence at risk for hydrops from cardiac compromise
Both twins in TTTS at risk for hydrops (greater in recipient due to volume overload)
May have hydrops from other causes unrelated to placental sharing
All cases need careful anatomic survey, infection work up ± chromosome evaluation
Perform formal fetal echocardiography for structure, function, rate and rhythm
Twin with encephalomalacia
Any destructive process may end in encephalomalacia regardless of chorionicity
May occur secondary to chronic hypoxia in donor twin in TTTS
Monochorionic twin demise places surviving twin at risk for ischemic injury described as “twin embolization syndrome”
Shared placental circulation → vascular communications between fetuses
Death of one twin → sudden drop in peripheral resistance for survivor → effectively severe hypotensive episode
Ischemic injury seen in brain/myocardium/kidneys
Sonographic findings
↑ Echogenicity in periventricular white matter, loss of grey-white matter differentiation
Eventual cystic encephalomalacia, porencephaly, microcephaly
Image Gallery
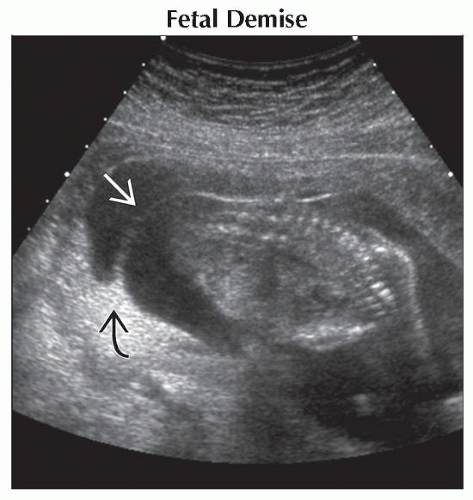 Ultrasound shows an inter-twin membrane
 and a twin peak sign and a twin peak sign  . Fluid volume in the smaller sac is low due to twin demise. The dead twin and sac shrank over serial follow-up scans. . Fluid volume in the smaller sac is low due to twin demise. The dead twin and sac shrank over serial follow-up scans.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|