Fig. 1
Anatomy of the brachial plexus, which is broadly divided into roots, trunks divisions, cords, and branches. LSS lower subscapular nerve, MABC medial antebrachial cutaneous nerve, MBC medial brachial cutaneous nerve, TD thoracodorsal nerve, USS upper subscapular nerve (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
Fig. 2
Injury to the brachial plexus can cause different injuries to each nerve root at preganglionic or postganglionic level. (a) Normal spinal cord and roots; (b) Avulsion injuries are preganglionic and cannot be repaired; (c) stretch injuries are postganglionic and have potential for spontaneous recovery; (d) rupture injuries can be repaired with surgery (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
The C5 and C6 nerve roots merge to form the upper trunk, C7 continues as the middle trunk, and C8 and T1 combine to form the lower trunk. The confluence of C5 and C6, termed Erb’s point, is also the spot where the suprascapular nerve arises. Each trunk then divides into an anterior and posterior division and passes deep to the clavicle. The three posterior divisions merge to form the posterior cord, while the anterior divisions of the upper and middle trunks combine to form the lateral cord. The anterior division from the lower trunk continues as the medial cord. The lateral cord divides into two terminal branches: the musculocutaneous nerve and the lateral cord contribution to the median nerve. The posterior cord continues as the axillary and radial nerves, and the medial cord contributes to the ulnar nerve and the median nerve. The portion of the brachial plexus formed by roots and trunks is located above the clavicle and termed the supraclavicular plexus; the portion formed by the divisions is found behind the clavicle and termed the retroclavicular plexus; the portion of the plexus formed by cords and terminal branches is termed the infraclavicular plexus.
A number of terminal branches emanate from the roots, trunks, and cords. The C5 root has a contribution to the phrenic nerve, dorsal scapular nerve (rhomboids), and long thoracic nerve (serratus anterior, also with contributions from C6 and C7). The suprascapular nerve (supraspinatus and infraspinatus) and nerve to subclavius muscle originate from the upper trunk. The lateral cord gives off the lateral pectoral nerve, while the medial cord gives off the medial pectoral nerve, medial brachial cutaneous nerve, and medial antebrachial cutaneous nerve. The posterior cord gives off the upper subscapular nerve (subscapularis), thoracodorsal nerve (latissimus dorsi), and lower subscapular nerve (subscapularis, teres major). Through careful and detailed testing of the function of muscles supplied by individual terminal nerve branches, the exact level of the injury to the brachial plexus can be determined. The sympathetic ganglion for T1 is located close to the T1 root and provides sympathetic innervation to the head and neck. Hence, a preganglionic injury at T1 level manifests clinically as Horner’s syndrome, characterized by ptosis, miosis, and anhidrosis on the affected side. In children, Horner’s syndrome can also lead to heterochromia (difference in eye color between both eyes). A lack of sympathetic stimulation in childhood can interfere with melanin pigmentation of the melanocytes in the superficial stroma of the iris.
Assessment
A complete history and physical examination, together with imaging and electrodiagnostic tools, allow localization of the level and severity of the injury to the brachial plexus. The aim of the preoperative workup is to determine the level of the injury – preganglionic (root level) or postganglionic (trunk, division, cord, or branches) – and also the severity of the lesion (partial or complete) for each component of the brachial plexus injured. This allows prognostication of recovery and a decision to be made for surgery. If no recovery is observed within the first 3–6 months, surgery is indicated. A preganglionic injury at one or more levels has little to no chance of recovery; hence, earlier intervention may be indicated.
Signs and Symptoms
A history of the mechanism of injury can be obtained from the patient or parents. High-energy injuries, for example, from motor vehicle accidents, have a lower chance of spontaneous recovery than low-energy injuries. Sharp injuries from lacerations should be explored acutely or subacutely. Gunshot wounds, in contrast, should be observed as many of these will exhibit spontaneous recovery over time.
As other injuries may be associated with the injury to the brachial plexus, management of these takes precedence in the multitrauma patient. Management follows acute trauma life support (ATLS) principles, with attention to the airway, breathing and circulation taking priority, followed by treatment of other life- and limb-threatening injuries. A detailed examination of the various components of the brachial plexus should be performed when the patient is stable and able to cooperate with the examiner. The exam should be recorded in a manner that allows for comparison of dates (Fig. 3). Serial detailed examinations help determine the presence or absence of nerve recovery and prognosis for spontaneous improvement.
Fig. 3
The Mayo brachial plexus evaluation form. This allows complete assessment of the entire extent of the injury at a glance (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
In an older child, a detailed systematic examination of the brachial plexus may be possible, together with documentation of muscle strength following the modified grading system of the British Medical Research Council (BMRC) for adults (M0 to M5) (Mendel and Florence 1990; Table 1). Note that a patient cannot have grade 3 power unless there is full active motion against the existing passive range of motion.
Table 1
BMRC scale for muscle strength
0: No muscle contraction visible |
1: Muscle contraction is visible but there is no movement |
2: Active movement is possible with gravity eliminated |
3: Active movement against gravity |
4-: Active movement against gravity and slight resistance |
4: Active movement against gravity and moderate resistance |
4+: Active movement against gravity and strong resistance |
5: Normal power |
A preganglionic lesion can be diagnosed through the presence of Horner’s syndrome, which suggests a root avulsion at the T1 level. Additional muscles that are innervated close to the spinal cord provide further evidence of a preganglionic lesion. Paralysis of the serratus anterior muscle, manifest through winging of the scapula (may be very difficult to examine secondary to paralysis of other periscapular muscles), suggests a lesion proximal to the long thoracic nerve, formed by the C5, C6, and C7 nerve roots. Atrophy of the rhomboids and parascapular muscles also suggests a preganglionic lesion proximal to the origin of the dorsal scapular nerve. Examination of individual sensory dermatomes may sometimes be unreliable due to overlap from other nerves or anatomical variation.
Different patterns of injury may be predicted based on the mechanism of injury. Upper brachial plexus injuries (Fig. 4) occur in motorcyclists who fall with the shoulder forced downward and the head pushed to the other side. Lower brachial plexus or pan-plexus injuries (Fig. 5) may occur during fall from height through hyperabduction of the injured upper extremity.
Fig. 4
Patterns of brachial plexus injury are predictable. Upper brachial plexus injuries occur when the shoulder is forced downward and the head pushed to the opposite side, for example, following a motorcycle crash (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
Fig. 5
Patterns of brachial plexus injury are predictable. Avulsion of the lower nerve roots with stretch and rupture of the upper nerve roots occurs, in this case during a fall from a tree, through catching a branch with the injured upper extremity causing hyperabduction and injury to the plexus (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
Examination of donor nerves should also be performed if nerve transfer is contemplated as a treatment option, such as the spinal accessory nerve, nerve to triceps, and medial pectoral nerve. Presence of a Tinel’s sign and tenderness in the supraclavicular or infraclavicular area suggests a postganglionic lesion, while absence of these suggests a preganglionic lesion. An advancing Tinel’s sign is a prognosticator and suggests a recovering lesion. Minimal preservation of movement in tested muscle groups suggests a partial injury with a greater potential for recovery. Examination of stability, active, and passive range of motion of all joints should also be assessed. Concomitant spinal cord injury should be ruled out by performing a full neurological examination of the upper and lower extremity, testing for power, sensation, and reflexes. Finally, a vascular exam should be performed, as the subclavian or axillary artery can be ruptured or damaged in substantial injury to the brachial plexus.
In younger children and infants, evaluation of single muscles is not easy and the patient often not cooperative or able to tolerate a lengthy physical examination. The muscle grading system of Gilbert and Tassin (1984) has been proposed (M0 = complete paralysis; M1 = perceptible contraction; M2 = weak movements; M3 = normal muscle); however, it is our practice to attempt to use the BMRC grading as not to confuse muscle grading systems. The posture of the child can be used to evaluate the level of injury. Paralysis of the upper roots is suggested by the upper limb being held in internal rotation and pronation, with no abduction possible. Slight flexion of the elbow may suggest involvement of C5, C6, and C7, while full extension of the elbow suggests involvement of only C5 and C6. In complete involvement of the brachial plexus, the entire upper extremity is flail. Horner’s syndrome may also be observed in a preganglionic lesion involving the C8-T1 roots.
Assessment of sensation in younger children and infants is similarly difficult. Often, children will only respond to testing with painful stimuli. Tinel’s sign may be used to assess for the level of the lesion and presence of nerve regeneration. In addition, in children, deafferentation pain is absent; hence, unlike in adults, patients with preganglionic lesions will seldom exhibit pain. Disturbances of the sympathetic system may be observed in the immediate period following injury, such as anhidrosis, cyanosis, and edema.
Imaging and Electrodiagnostic Studies
Radiographs of the cervical spine, shoulder, and chest should be obtained as part of the workup. Transverse fractures of the cervical vertebrae suggest preganglionic injuries with root avulsion. Fractures of the clavicle or ribs (first or second) may be associated with injuries to the brachial plexus. Fractures of other ribs may preclude the use of intercostal nerves as a donor nerve for nerve transfer (Kovachevich et al. 2010). An elevated hemidiaphragm suggests damage to the phrenic nerve and a possible preganglionic injury.
Computed tomography (CT) myelography is very useful in determining the presence of preganglionic injury. This is usually performed at least 3–4 weeks after the injury. This delay allows blood clot in the area of the avulsed cervical root to resorb and for a pseudomeningocele to form. CT myelography has been shown to have a diagnostic accuracy ranging from 70 % to 95 % for detection of nerve root avulsion compared to plain myelography alone (Carvalho et al. 1997; Doi et al. 2002). Presence of a pseudomeningocele is associated with preganglionic injury in 98 % of cases (Nagano et al. 1989; Fig. 6).
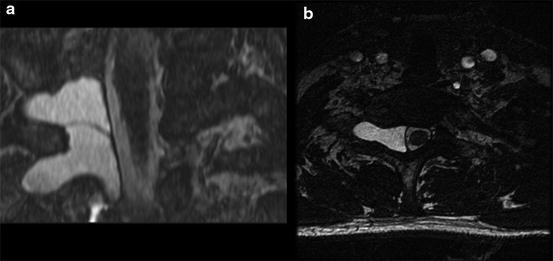
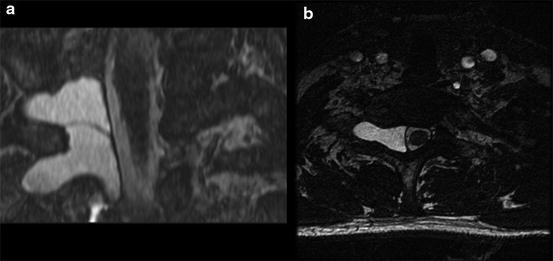
Fig. 6
CT myelogram of patient with root avulsion on right at C6 and C7 levels. (a) Large pseudomeningocele extending into the right neural foramen at C7-T1 level on coronal view; (b) the same pseudomeningocele seen on axial view (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
Magnetic resonance imaging (MRI) is also useful in evaluating patients with suspected root avulsion (Fig. 7) and allows better visualization of the entire brachial plexus. Large neuromas, abnormalities of the rootlets, inflammation and edema, as well as mass lesions can be visualized using MRI. While CT myelography should still be considered the first-line imaging modality in suspected nerve root avulsion, MRI using an overlapping coronal-oblique slice technique has been shown to be as reliable as CT myelography in detecting nerve root avulsion, with a diagnostic accuracy of 93 % (Doi et al. 2002).
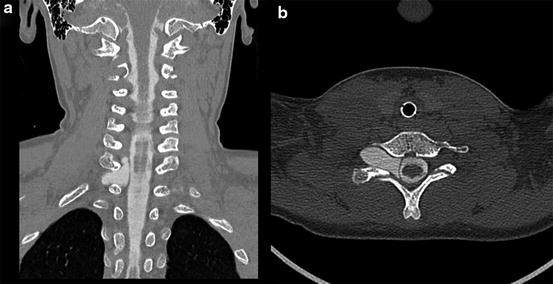
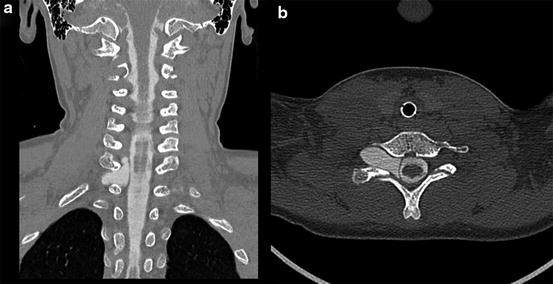
Fig. 7
MRI of patient with pseudomeningoceles at right C6, C7, and T1 levels. (a) Two right-sided cervical pseudomeningoceles are seen on coronal view; (b) axial view of one pseudomeningocele (By permission of Mayo Foundation for Medical Education and Research, All rights reserved)
Electrodiagnostic studies are pivotal in localizing and determining severity of injury in the brachial plexus. Baseline nerve conduction studies (NCS) and electromyography (EMG) should be performed 3–6 weeks after injury, after Wallerian degeneration has occurred. Serial follow-up studies can then be performed every 6–10 weeks to assess for recovery, complementing findings on physical examination for the purposes determining if there will be spontaneous recovery or if surgical reconstruction is necessary.
Nerve conduction studies include testing of motor and sensory nerves. Motor nerve testing is useful in detecting more distal injuries and conduction blocks in incomplete injuries. In traumatic brachial plexus injuries, amplitudes of compound muscle action potentials (CMAPs) are in general low. Sensory nerve testing is useful in determining whether a root injury is pre- or postganglionic. In a preganglionic injury, the dorsal root ganglion is spared injury even though it is detached from the spinal cord; hence, sensory nerve action potentials (SNAPs) are preserved. However, the patient is insensate in the associated sensory nerve distribution. There is excellent correlation between C6 (superficial radial nerve), C7 (median sensory to long digit), C8 (ulnar sensory nerve to small digit), and T1 (medial antebrachial cutaneous nerve) nerve root levels and individual peripheral sensory nerves in the upper extremity, aiding in localizing the level of the lesions in the brachial plexus. C5 and C6 innervate the lateral antebrachial cutaneous nerve, and this can be tested as part of sensory nerve evaluation for C5.
EMG provides the most reliable assay of motor nerve injury. Fibrillation potentials and positive sharp waves, indicative of denervation, can be seen in proximal muscles as early as 10–14 days and in distal muscles in 3–6 weeks. Motor unit analysis can determine the presence of injury in individual muscles. Polyphasic motor units occur in the presence of injury or pathology, while nascent potentials indicate axonal regeneration. Reduced recruitment of motor unit potentials can be demonstrated immediately after injury. Testing of individual muscles can help to distinguish preganglionic from postganglionic lesions. For example, denervation of the paraspinal muscles, rhomboids, and serratus anterior is a strong indicator of a preganglionic lesion as these muscles are innervated by branches from the cervical roots. Unfortunately, EMG recovery does not always equate with clinical recovery, and evidence of clinical recovery may not be detected through EMG in complete lesions, despite ongoing regeneration, when target end organs are more distal.
Intraoperative electrodiagnostic studies are useful prior to making a definitive surgical decision. These include the use of nerve action potentials (NAP), somatosensory and motor evoked potentials (SSEPs and MEPs) and CMAPs. The presence of a NAP distal to a lesion indicates preserved axons in an incomplete lesion or significant regeneration, with a correspondingly better prognosis (Kline and Happel 1993). Hence, neurolysis alone without additional treatment may be sufficient. The presence of an SSEP and MEP suggests continuity between the peripheral nervous system and the spinal cord via a dorsal root and ventral root, respectively. Hence, an SSEP and MEP is only present in postganglionic lesions. As lesions are not necessarily all or none, there may be situations where the SSEP is present and MEP absent or vice versa. In such cases, the viability of the root becomes difficult to ascertain, and correlation with EMG, clinical findings, and radiographic findings is necessary. CMAPs are useful in partial lesions where the magnitude of the lesion is proportional to the number of functioning axons.
Injuries Associated with Traumatic Brachial Plexus Injury
Brachial plexus injuries are often caused by high-energy trauma; hence, there are often substantial concomitant injuries. When a patient is evaluated in the emergency room, standard ATLS principles should be followed and the airway, breathing, and circulation stabilized prior to a search for other life- and limb-threatening injuries.
Injuries that should be evaluated include traumatic brain injuries and spinal cord injuries as well as vascular injuries, ipsilateral upper extremity musculoskeletal injuries, scapulothoracic dissociation, pneumothorax, hemothorax, and rib fractures. Treatment of these injuries takes precedence initially over the brachial plexus injury.
Classification
Brachial plexus injuries can be classified by the cervical/thoracic nerves involved, level of the injury, and severity of each nerve injury according to the Seddon (1975) and Sunderland (1978) classifications.
Determination of the cervical/thoracic nerves involved in the injury as well as level of the injury is based on clinical examination supplemented by imaging studies, as described previously. The level of the injury can be broadly divided into preganglionic root, supraclavicular plexus (roots and trunks), retroclavicular plexus (divisions), and infraclavicular plexus (cords and branches). Different authors have described various classifications for the level of injury, pursuant on their individual surgical strategies. Narakas (1981) describes dividing the level of injury into five levels (supraganglionic root, infraganglionic spinal nerve, infraganglionic trunk, and retroclavicular and terminal branches). Chuang (2010) alternatively divides brachial plexus injuries into four levels (Level 1, preganglionic root injury including spinal cord, rootlets, and root injuries; Level 2, postganglionic spinal nerve injury limiting the lesion to the interscalene space and proximal to the suprascapular nerve; Level 3, preclavicular and retroclavicular BPI including trunks and divisions; Level 4, infraclavicular BPI including cords and terminal branches proximal to the axillary fossa).
The severity of the injury to each nerve is classified according to the Seddon/Sunderland classification, with five levels of nerve injury. Seddon initially described three basic types of peripheral nerve injury, which was expanded to five types by Sunderland. In neurapraxia (first-degree injury), a focal physiologic conduction block exists at the site of nerve injury, with the endoneurium, perineurium, and epineurium remaining intact. This typically recovers spontaneously within days to weeks and does not require surgical intervention. In axonotmesis (second- to fourth-degree injury), the connective tissue framework of the nerve is preserved, but the axon is disrupted to varying extents, resulting in Wallerian degeneration distal to the site of nerve injury with a disruption of nerve conduction. In a second-degree injury, the axon is disrupted, but the endoneurium, perineurium, and epineurium are preserved. Nerve regeneration and recovery of motor and sensory function are expected but may take months to years. In third-degree injury, the axon and endoneurium are disrupted, but the perineurium and epineurium are intact. In a fourth-degree injury, the axon, endoneurium, and perineurium are disrupted, while the epineurium remains intact. In third- and fourth-degree injuries, regeneration occurs variably or may not occur at all; hence, these lesions often require surgical intervention. In neurotmesis (fifth-degree injury), the nerve is completely disrupted; hence, surgical intervention is necessary. Fifth-degree injuries include preganglionic avulsions and postganglionic ruptures of the brachial plexus.
Outcome Tools
There is no clear consensus on the best instrument to measure outcomes after brachial plexus reconstruction in either the adult or pediatric patient. The BMRC muscle strength scale is the most common tool used, on a scale from M0 to M5. However, this tool has a number of limitations including its lack of precision and inter-rater reliability as well as a wide range of strength covered by grade of M4 (MacAvoy and Green 2007; Shahgholi et al. 2012). The Disabilities of the Arm, Shoulder and Hand (DASH) score is the most validated measure of upper extremity function (Dowrick et al. 2005) and has been useful as an outcome tool following brachial plexus reconstruction; however, it is not validated for the pediatric population.
A number of outcome tools are used to assess outcomes following obstetric brachial plexus injury and reconstruction, and there may be a role to adopting them to infants or young children following traumatic brachial plexus injury. The most widely used tool is the Mallet classification (Abzug and Kozin 2010), which measures integrity of muscles innervated by the upper brachial plexus. The arm is tested in five different movements: abduction, external rotation, hand behind head, hand to back, and hand to mouth. Each movement is classified from grade 0 to V. A recent modification was proposed, the addition of a hand to belly button category, which tests the child’s ability to reach to midline. Other tools used include the Toronto Test Score (Bae et al. 2003), Active Movement Scale, and Gilbert shoulder classification.
Differences Between Adult and Pediatric Injuries
In pediatric patients, surgical reconstruction options are affected by the presence of open growth plates and potential growth that may affect the long-term results of certain procedures. The most active physes in the upper extremity include the proximal humerus, which accounts for 80 % of longitudinal growth (Pritchett 1991) and the distal radius. The length of the humerus grows approximately 1.3 cm in boys and 1.2 cm in girls from age seven until skeletal maturity, while the length of the radius grows approximately 1.0 in boys and 0.9 cm in girls from age seven until skeletal maturity (Pritchett 1988). Boys usually reach skeletal maturity between 16 and 17 years old, while girls reach skeletal maturity between 14 and 15 years old.
Therefore, in the pediatric population, the use of functional free muscle transfer should be done so with care as the transferred muscle may not grow in proportion with the rest of the upper extremity and lead to joint contractures. Additionally, secondary procedures that cross joints, such as tendon transfers, tenodesis, and joint fusions, may lead to joint contractures and limitation of function of the affected limb.
Treatment Options
Surgery has been shown to be beneficial for patients in traumatic brachial plexus injuries with no hope for spontaneous recovery or in the absence of clinical or electrodiagnostic evidence of recovery. The mechanism of injury provides a vital clue to decide the possibility for spontaneous recovery. In sharp or blunt injuries causing lacerations, all patients should undergo surgical exploration as the possibility of spontaneous recovery is low. In gunshot wounds, many patients will recover spontaneously as the majority of injuries are neuropraxic and caused by the shock wave from the passage of the projectile. Hence, nonoperative management is preferred initially. In traction injuries, the indication and timing for surgery are more controversial and would depend on the type and exact mechanism of injury. Early exploration of the brachial plexus between 3 and 6 weeks should be performed if there is a high suspicion of root avulsion. In general, surgical exploration of the brachial plexus should be performed by 6 months of injury and is not performed more than 12 months after the injury as results are poor, as the time for nerve regeneration to the target muscle is greater than the time of survival of the denervated motor end plate.
Nonoperative Management
Indications/Contraindications
In patients waiting for surgery or those treated conservatively, physical therapy is essential to strengthen functioning muscles, maintain range of motion, and prevent stiffness and joint contractures. Occupational therapy may be useful in modification of the patient’s workplace setting and home environment to improve the patient’s functional ability and also in use of orthoses and adaptations (Booney 1998). Specific indications and contraindications for pure nonoperative management of traumatic brachial plexus injuries are listed below (Table 2). However, rehabilitation has a role to play in all surgical patients as well, both preoperatively and postoperatively.
Table 2
Traumatic brachial plexus injuries: nonoperative management
Indications | Contraindications |
|---|---|
Mechanism of injury: gunshot wounds, certain traction injuries | Mechanism of injury: sharp lacerations, root avulsions |
Patient expectations: unrealistic goals, unwillingness to undergo surgery | Patient expectations: agreeable with surgical reconstruction |
Spontaneous ongoing recovery in involved elements | Lack of improvement on clinical and electrophysiologic testing |
Techniques
Physical/Occupational Therapy Recommendations
The main goals in treatment of traumatic brachial plexus injury patients are prevention of secondary deformities, maintenance of passive range of motion, pain suppression, sensory rehabilitation for recovery of somatosensory deficits, treatment of developmental disregard, and postoperative care (Smania et al. 2012).
Due to the long time needed for reinnervation of muscles following BPI, muscle atrophy will lead to muscle imbalance, and subsequent secondary deformities of the upper extremity are commonplace. Hence, an important component of rehabilitation consists of the prevention of joint contractures.
Passive movements of the injured upper extremity can be combined with an orthoses, such as elbow and hand splints, to avoid joint stiffness and to maintain range of motion. Biofeedback can be used to lessen cocontraction. Botulinum toxin injections can be used for the treatment of imbalanced muscles. It is particularly important to avoid deformities such as internal rotation of the shoulder, which markedly reduces function and ability to care for one’s self and may also lead to glenohumeral dysplasia.
While neuropathic pain after BPI is a major concern in adult patients, in the pediatric population, deafferentation pain is often absent, despite having a greater chance of preganglionic injury. However, if this becomes an issue in older pediatric patients, multidisciplinary management is mandatory for optimal patient care. Different modalities of treatment are used, such as pharmacotherapy, physical therapy, transcutaneous electrical nerve stimulation (TENS), and psychosocial intervention, all playing important roles in pain management.
Following a peripheral nerve injury, patients develop altered profiles of neural impulses. Hence, sensory reeducation is useful to reprogram the brain through the use of cognitive learning techniques and graded tactile stimuli to improve tactile gnosis (Jerosch-Herold 2011). Exercises including perception of different shapes and textures as well as localization of stimuli help retrain the brain to recognize sensory stimuli through cortical plasticity. Developmental disregard, or behavioral suppression of motor activity in the impaired limb, has been treated through a targeted technique, the constraint-induced movement therapy (CIMT) (Fritz et al. 2012). This aims to increase use of the impaired limb by limiting use of the non-affected upper extremity. CIMT has been proposed to work through changes in behavioral approach by the patient with subsequent cortical reorganization in the brain (Hoare et al. 2007).
Postoperative rehabilitation is key to achieving good functional results. An example is passive stretching of muscles to prevent secondary deformities such as maintaining external rotation of the shoulder to minimize glenohumeral joint deformity. Following nerve transfers, induction exercises are also used by patients (Terzis and Kostopoulos 2007) to help the donor nerve to fire and reactivate the reinnervated muscle.
Outcomes
The literature is scarce on objective outcomes of rehabilitation through physical and occupational therapy. However, it is the experience of most other brachial plexus surgeons that physical and occupational therapies, both in the preoperative and postoperative periods, are essential to optimize outcomes following surgical reconstruction of the brachial plexus.
Operative Management
Indications/Contraindications
Surgical management is indicated when spontaneous recovery is impossible, for example, in root avulsions or in the absence of clinical and electrodiagnostic evidence of recovery by 6 months after injury. There are few absolute contraindications to surgical reconstruction of the brachial plexus. These include the unwillingness of the patient to undergo the surgical procedure with subsequent prolonged rehabilitation or unrealistic goals of the patient. Other contraindications include patients who exhibit spontaneous ongoing recovery and those with life-threatening conditions precluding surgery. Patients presenting late (more than 12 months after injury) are not candidates for primary plexus reconstruction but may be candidates for free functioning muscle transfer.
Timing of Surgery
Immediate exploration and repair is performed in patients with a sharp open injury of the brachial plexus. Surgery allows direct visualization and repair of injured elements. For patients with blunt injuries to the brachial plexus without chances of recovery, surgery is performed about 3–4 weeks after the injury to allow the zone of nerve injury to delineate. In patients with a high suspicion of root avulsion, surgery can be performed even earlier.
Delayed surgery is performed in patients with a chance for spontaneous recovery. Exploration may be delayed up to 6 months after the inciting injury, particularly for patients where the mechanism of injury suggests that spontaneous recovery is possible, such as low velocity gunshot wounds or closed traction injuries. Lack of progressive recovery on clinical examination and electrophysiologic studies is an indication for surgery.
Finally, secondary reconstruction through procedures such as free functioning muscle transfer (FFMT), tendon transfers, and adjunctive procedures are performed for patients who present late (more than 12 months after injury). In these patients, primary plexus reconstruction is associated with poor results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


