Trauma
Worldwide, motor vehicle crashes are the most frequent cause of death from unintentional injury. In the United States, there were more than 40,000 vehicular deaths in 1994, equivalent to approximately 20 deaths for each 100,000 persons. According to the National Highway Traffic Safety Administration (1998), vehicle deaths in females increased 6.7 percent from 1992 to 1994, as compared with an increase of only 2.4 percent in males for the same period. Car accidents are the leading cause of death in females ages 8–28.
The overall death rate for women due to unintentional injury is 24/100,000 population; motor vehicle crashes, suicide, and homicide account for more than 95 percent of these deaths. Overall, females are more likely than males to be involved in auto accidents, viz, 143 female drivers versus 95 male drivers per 10 million miles driven according to National Safety Council data. Considerable geographic variation exists in both death rates and cause of death as a result of trauma. Death from motor vehicle crashes is encountered at much higher rates in areas of low population density, for example, Manhattan, New York versus Esmarelda County, Nevada—2.5 versus 558 per 100,000, respectively. Conversely, firearm deaths and homicides are higher in the West and South, particularly in areas of low income and high population density (Baker and colleagues, 1988).
Fetal loss due to trauma is difficult to quantify as there are no compiled statistics, and the relationship of trauma to pregnancy loss is not always clear in individual cases. In a recent review of 80 injured pregnant women, Theodorou and colleagues reported a 17.5 percent incidence of fetal death. The two independent risk factors for fetal death were a non-viable pregnancy and an Injury Severity Score (ISS) of 9 or greater. There was a fivefold increase in fetal death if both risk factors were present. In another review of 61 pregnant women who experienced trauma, Baerga-Varela and colleagues (2000) reported a 15 percent fetal-neonatal death rate. However, the authors of this series were unable to detect a difference in ISS between viable and nonviable pregnancies. Over the past two decades, as other causes decreased, trauma has become the most common cause of maternal mortality (Dannenberg, 1995; Fildes, 1992; Jacob, 1998; and their colleagues; Harper and Parsons, 1997). Importantly, in many cases, trauma arises from domestic abuse or battering (Eisenstat and Bancroft, 1999).
The provision of modern trauma service relies on the cooperative effort of a variety of health care providers. It is of paramount importance to recognize that two patients are involved—mother and fetus (Maull, 2001). When the trauma victim is pregnant, the obstetrician becomes a vital member of the multidisciplinary trauma team. Often, particularly in cases of minor trauma, the obstetrician is the central figure in providing care. It is the obstetrician who has the special skills and knowledge relevant to pregnancy that best serve the interest of the woman and her fetus. All trauma centers should have a protocol for incorporating an obstetrician into the trauma team, and, likewise, obstetricians should be prepared to assist the trauma team when the victim is pregnant.
PHYSIOLOGIC CHANGES OF PREGNANCY
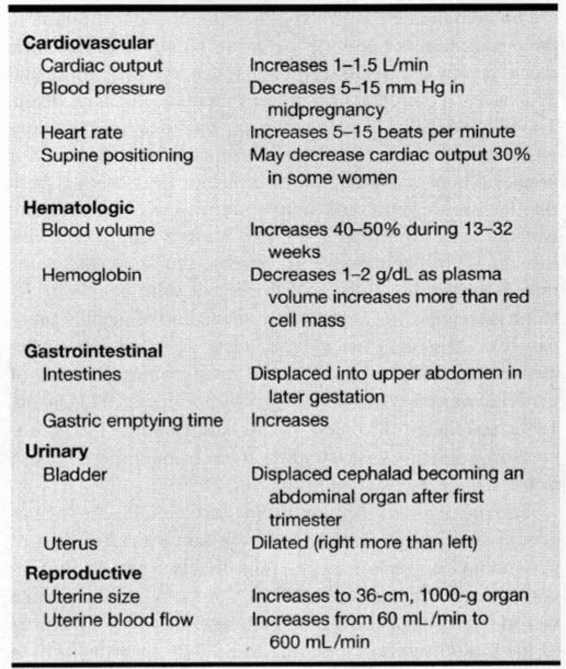
Crucial to resuscitation of the pregnant trauma victim is an understanding of both fetal and maternal physiology, particularly the physiologic response to stress and hypovolemia. Fundamental differences in the physiologic response to trauma occur as a result of pregnancy, and obstetric expertise is an invaluable asset to the trauma team. An overview of some of these changes during pregnancy is shown in Table 32-1.
TABLE 32-1. Anatomic and Physiologic Changes of Pregnancy
FETAL PHYSIOLOGY
Several factors are important in determining the impact of a traumatic event on pregnancy outcome. These include gestational age, type and severity of trauma, and the extent of disruption of normal maternal and fetal physiology (Pearlman and associates, 1990a). In the first week of conception, the nonimplanted embryo is relatively resistant to noxious stimuli. Even during the first trimester, the uterus resides safely within the confines of the bony pelvis and is protected to a large degree from direct uterine trauma. At any gestational age after implantation, however, maternal hypovolemic shock may have a significant impact on the developing embryo/fetus. Uterine blood flow is not autoregulated; that is, it is maximal in the normal physiologic state. Maternal hypovolemia may result in vasoconstriction in many vascular beds, including those of the uterus. Even in the absence of uterine artery vasoconstriction, decreases in maternal blood pressure may result in decreased uterine blood flow. These facts underlie the importance of maintaining adequate maternal blood volume as a first step in fetal resuscitation. The third-trimester fetus can adapt to decreased uterine blood flow and oxygen delivery by diverting blood distribution to the heart, brain, and adrenal glands (Wilkening and Meschia, 1983). Furthermore, because fetal hemoglobin has a greater affinity for oxygen than adult hemoglobin, fetal oxygen consumption does not decrease until the oxygen delivery is reduced by 50 percent (Iwamoto, 1989).
Blunt or penetrating trauma may result in rupture of the membranes. In the second trimester, rupture without reaccumulation of fluid may result in pulmonary hypoplasia or orthopedic deformity. In addition, infection may develop with ruptured membranes at any gestational age. Injury to the placenta may result in separation or laceration leading to fetal anemia, hypoxemia, or hypovolemia (Dahmus, 1993; Goodwin, 1990; Pearlman, 1990b; Williams, 1990; and their associates).
MATERNAL ANATOMIC AND PHYSIOLOGIC CHANGES
Nearly every maternal organ system undergoes anatomic or physiologic changes during pregnancy. The description that follows emphasizes the importance of some of these changes in managing the pregnant trauma victim, particularly as these differences impact on the usual practice of trauma management.
A major concern for trauma victims is internal hemorrhage and hypovolemia. The sentinel findings are changes in vital signs—typically, hypotension and tachycardia. Consideration is given to the normal decrease in systemic vascular resistance resulting in a decrease in blood pressure of 10–15 mm Hg and an increased pulse rate of 5–15 beats per minute (bpm), particularly in the second trimester. These changes are accentuated if the woman is placed in the supine position; for example, strapped to a long board in order to secure the spine. The resultant potential decrease in venous return from the lower extremities can reduce central venous volume and result in a diminished cardiac output of up to 30 percent. Simple manual displacement of the uterus to the left, or placement of a rolled towel under the backboard while assuring the spine remains secure alleviates most of this effect.
Blood volume increases by a mean of 50 percent in the singleton gestation. This is usually maximal by 28–32 weeks. Red cell mass increases to a lesser degree than does plasma volume, resulting in a slightly decreased hemoglobin and hematocrit concentration. Iron-deficiency anemia is also common during pregnancy, and together with the normal dilution, hemoglobin concentration may be as low as 9–11 g/dL. These hematologic changes have two potential implications in the management of the trauma victim: (a) anemia may be confused with active bleeding and hypovolemia and (b) blood volume estimates should be modified upward during fluid resuscitation.
Several major pregnancy-induced changes in the gastrointestinal tract are important for trauma management. Compartmentalization of the bowel upward serves to protect it during lower abdominal trauma, but increases the risk of injury when there is penetrating trauma to the upper abdomen in later pregnancy. Complex injuries to the small bowel can be encountered with multiple entry and exit wounds as a result of its being crowded and compacted into the upper abdomen. Decreased gastric motility results in prolonged emptying time, thereby increasing the risk of aspiration. Rebound tenderness and guarding are less usually apparent in advanced gestation; thus, clinical diagnosis of hemoperitoneum is less reliable. This is likely due to stretching of the abdominal musculature and peritoneum.
The dramatic increase in uterine blood flow, up to 600 mL/min, may result in rapid exsanguination if there is avulsion of the uterine vessels or rupture of the uterus. Retroperitoneal hemorrhage from remarkably hypertrophied vasculature is a common complication of pelvic fracture. Enlargement of the uterus makes it susceptible to direct abdominal trauma. Injury to the uterus itself (uterine rupture), its contents (abruptio placentae or direct fetal injury), or adjacent organs (bladder rupture) are possible. While some of these are typically seen with direct and violent trauma, for example, uterine rupture, others may occur with minimal maternal trauma, for example, abruptio placentae.
BLUNT ABDOMINAL TRAUMA
With blunt trauma, head injury and hemorrhagic shock are equal contributors to over 85 percent of all maternal mortality (Crosby and Costiloe, 1971). As discussed, trauma is currently the most commonly cited cause of death during pregnancy. Most cases of trauma in pregnancy are caused by motor vehicle accidents, falls, and direct assault (Pak and colleagues, 1998).
Motor vehicle crashes are the most common cause of blunt abdominal trauma during pregnancy. These are followed by falls, direct assaults to the abdomen, and miscellaneous causes (Pearlman and associates, 1990b). While some investigations imply that changes in the center of gravity due to pregnancy result in increased clumsiness and propensity to injury, there is no evidence that the frequency or severity of trauma is greater during pregnancy (Buchsbaum, 1968; Crosby, 1983, 1986; Pearlman and colleagues, 1990a). Due to anatomic and physiologic changes discussed earlier, however, certain patterns of injury are encountered. For example, an increased incidence of spleen rupture and retroperitoneal hemorrhage is reported during pregnancy, whereas bowel injuries may occur less frequently (Buchsbaum, 1967; Pepperell and associates, 1977; Rothenberger and coworkers, 1978).
Battering is probably underestimated as a cause of trauma during pregnancy, and around 10 percent of otherwise healthy women are physically abused during pregnancy (Berenson, 1991; Cokkinides, 1999; Curry, 1998; Poole, 1996; and all their associates). An additional 20 percent of women in these studies reported abuse prior to the pregnancy or were threatened with abuse during the pregnancy (Helton and colleagues, 1987). In a recent prospective cohort study, Covington (2001) reported that 16 percent of teens reported prenatal violence and 9.4 percent reported severe violence. Approximately 12 percent of adults reported violence and approximately 5 percent reported severe violence (“hitting, kicking, stabbing”). Teens experienced abdominal trauma more often than adults.
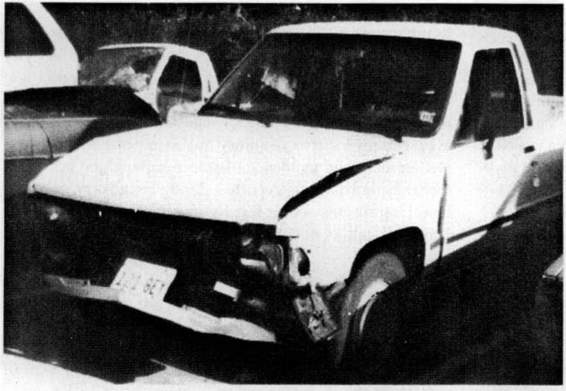
Fetal well being is a major concern whenever a pregnant woman is injured. The fetus can be harmed by a variety of mechanisms that include direct fetal injury, abruptio placentae, or massive fetomaternal hemorrhage. While fetal injuries are more frequent following severe trauma, minor trauma, such as shown in Figure 32-1, is much more frequent, and thus, fetal losses follow relatively minor accidents (Dahmus, 1993; Goodwin, 1990; Pearlman, 1990b; Williams, 1990; and their colleagues). According to Crosby and Costiloe (1971), the most frequent cause of fetal death was maternal death. This was certainly true with severe motor vehicle accidents from the 1960s when only two-point driver and passenger restraints were available, and when seat belts were infrequently used. Since then, numerous series demonstrate that most fetal deaths occur in association with relatively minor maternal injuries (Fries and Hankins, 1989; Stafford and colleagues, 1988). It is again emphasized that this is the result of the high ratio of minor to life-threatening injuries, although it is clear on a case-by-case analysis that severe injury more commonly results in fetal loss (Pearlman and colleagues, 1990b; Rothenberger and colleagues, 1978).
FIGURE 32-1. Motor vehicle accident with relatively minor damage to the vehicle and no evidence of maternal trauma, yet death of the fetus occurred as a result of intracranial and intrahepatic hemorrhage.
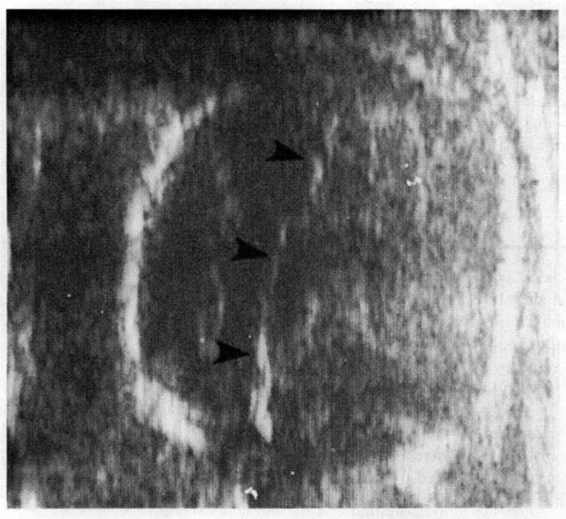
In four reports of 57 fetal and neonatal deaths due to trauma, only six were associated with maternal deaths (Agran, 1987; Hoff, 1991; Lane, 1989; Pepperell, 1977; and their colleagues). Of the other 51 deaths, more than half were associated with minor maternal injury—often considered trivial. More than two-thirds of the fetal deaths were due to abruptio placentae, and there was direct fetal injury in 25 percent (Fig. 32-2). There was a disproportionate number—over 90 percent—of fetal losses due to abruptio placentae in the minor injury group, suggesting that even minor degrees of uterine deformation may result in abruptio placentae.
FIGURE 32-2. Ultrasound of the head of the fetus involved in the accident shown in Figure 32-1 demonstrating a midline shift (arrows point to falx) and large intracranial hemorrhage. The fetus also demonstrated repetitive variable decelerations on electronic heart-rate monitoring.
COMPLICATIONS
ABRUPTIO PLACENTAE. Premature placental separation is the most common cause of fetal or neonatal death resulting from trauma. The mechanism of this injury has been well described by Crosby and colleagues (1968) in their study of seat belts in pregnant baboons. Using high-speed cameras and intrauterine pressure catheters, they demonstrated that there are two times during an accident when the intrauterine environment is at risk for injury (Fig. 32-3). In a front-facing decelerative event—for example, a restrained woman in a car hitting a tree at 25 mph—the body is thrown suddenly forward. During the initial phase of deceleration (0-0.06 seconds), there is an increase in intrauterine pressure to about 500 mm Hg. This corresponds to a time period when the body is compressed downward into the seat. It may also result from the uterus being thrown forward against the anterior abdominal wall. There is a second increase in intrauterine pressure with a two-point restraint, whereby the uterus is compressed by the hyperflexed torso (Fig. 32-3). With a three-point restraint, there were similar increases in intrauterine pressure at the time in which the body was compressed against the shoulder harness.
FIGURE 32-3. Impact sequence. Relationship between body motion, uterine pressure, and belt tension. (Modified from Crosby and associates, 1968, with permission.)
The effect of air bags, which have become standard on many vehicles sold in the United States, has not been tested during pregnancy. A few case reports are encouraging (Sims and associates, 1996); however, placental abruption with stillbirth has been described despite their use (Schultze and colleagues, 1998). Current studies on the effects of various restraint systems during pregnancy are being conducted jointly by the University of Michigan and General Motors Corporation.
Abruptio placentae complicates 1–5 percent of minor trauma cases as compared with 20–50 percent following major injuries (Pearlman and Tintinalli, 1991). The physical characteristics of the uterine and placental tissues appear to play an important role in the pathogenesis of abruptio placentae. Deformation of the relatively elastic myometrium can result in a shearing effect of the inelastic placenta away from the decidua basalis (Fig. 32-4). The placenta does not have to be implanted anteriorly, as the original impact sets up a wave within the uterus, causing initial elongation and narrowing of the uterus, followed by shortening and widening. As these deforming forces affect the entire uterus, any placental location is at risk for separation following impact. In some circumstances, abruptio placentae develops without direct uterine impact. For example, we have managed two cases of abruptio placentae that developed following hard falls directly on the buttocks. Presumably, the fall resulted in transmission of this energy to setting up a waveform within the uterus.
FIGURE 32-4. Illustration of woman striking a steering wheel with deformation of the uterus and separation of the placenta from the decidual basalis.
UTERINE RUPTURE. Trauma is an uncommon cause of uterine rupture and has been reported in about 0.6 percent of all uterine ruptures during pregnancy (Pearlman and colleagues, 1990a). Unlike abruptio placentae, uterine rupture is associated with direct and intense uterine impact (Buchsbaum, 1968; Handel, 1978; Weinstein and Pallais, 1968). Factors that predispose to uterine rupture during labor—for example, prior uterine scar, multiple gestation, and hydramnios—also predispose to traumatic rupture. Importantly, traumatic rupture is also encountered in the absence of any predisposing factors. Even with a prior cesarean delivery, traumatic rupture has been described remote from the uterine scar (Weinstein and Pallais, 1968).
During early pregnancy, the uterus is relatively resistant to direct injury. This is so with intense, direct abdominal injury unless the pelvic ring collapses as a result of fracture (Crosby and Costiloe, 1971). After the first trimester, the uterus becomes an abdominal organ and is susceptible to direct trauma. Direct uterine trauma may result in (a) complete disruption of the myometrial wall with or without extrusion of the fetus, placenta, or umbilical cord into the abdominal cavity; (b) avulsion of the uterine vasculature with intraperitoneal or retroperitoneal hemorrhage; (c) less than full thickness injury to the myometrial wall, for example, serosal hemorrhage or abrasions; or (d) complete uterine avulsion, which has been described as a result of an improperly placed lap belt (McCormick, 1968). Figure 32-5 shows an example of how a directed force can “burst” the uterus.
FIGURE 32-5. A.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree