Fig. 1
(a–c) Photographs and radiograph of a 3-year-old boy who sustained a traumatic amputation of his left thumb
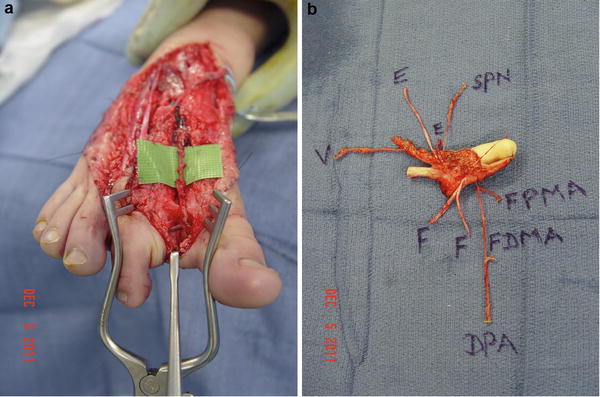
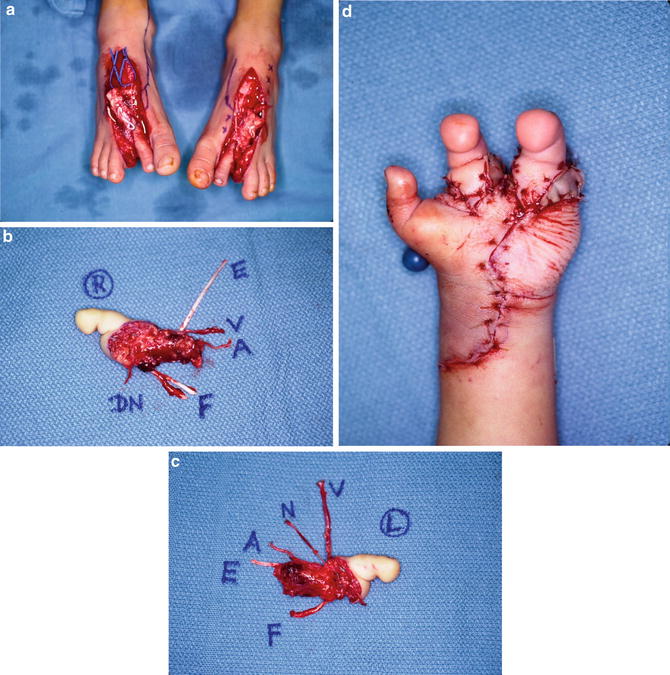
Fig. 2
(a) Dissection of the first dorsal metatarsal artery (FDMA) as the arterial supply to a right second toe transfer. (b) Second toe transfer
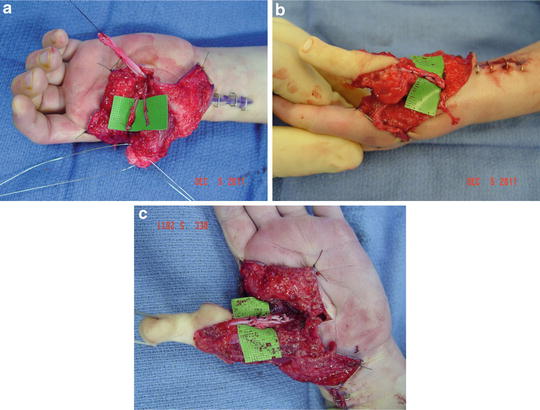
Fig. 3
(a) Dissection of the flexor pollicis longus tendon and radial and ulnar digital nerves to the thumb. (b) Repair of the extensor digitorum longus tendon to the extensor pollicis longus tendon. (c) Repair of the flexor digitorum longus tendon to the flexor pollicis longus tendon
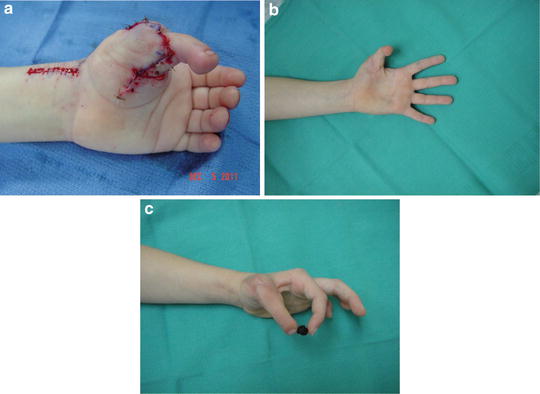
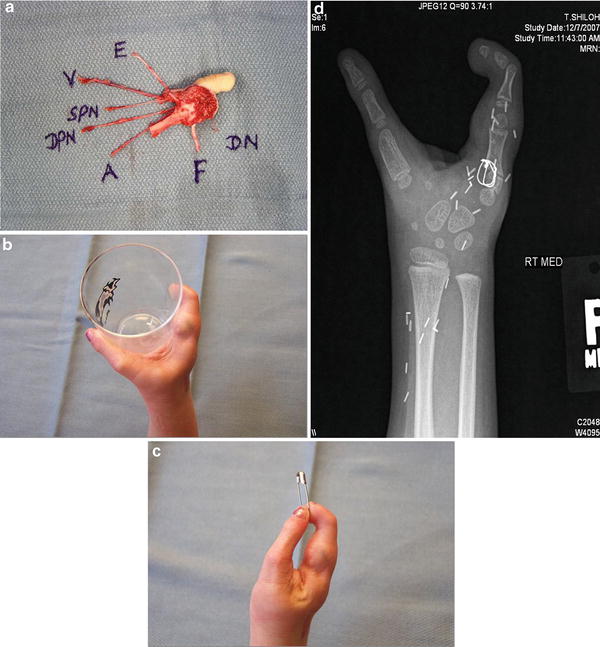
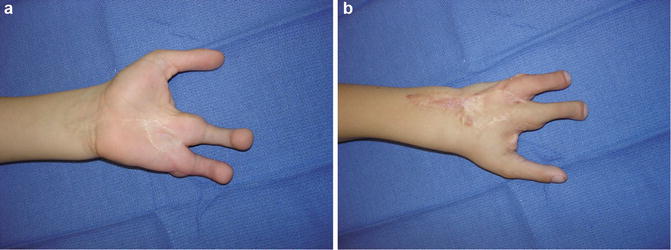
Fig. 4
(a) Immediate intraoperative photograph of the right second toe transfer to the left thumb. (b, c) One year after right second toe-to-left thumb transfer
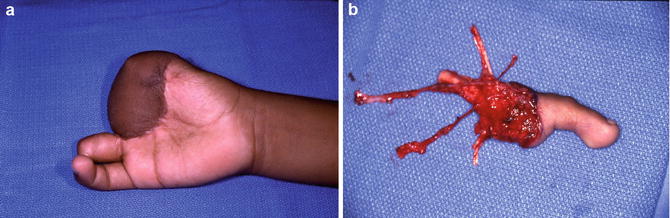
Fig. 5
(a) Eleven-year-old boy who sustained amputations of his right thumb, index, and middle fingers and the distal phalanx of the ring finger, initially covered with a groin flap. (b) Left second toe transfer
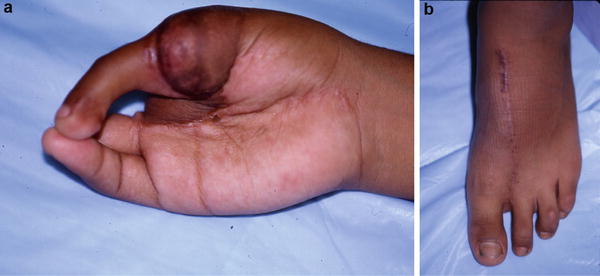
Fig. 6
(a) Left second toe to right thumb transfer. (b) The left foot donor site

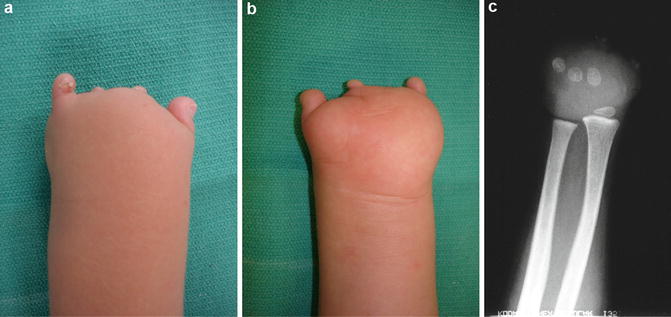
Fig. 7
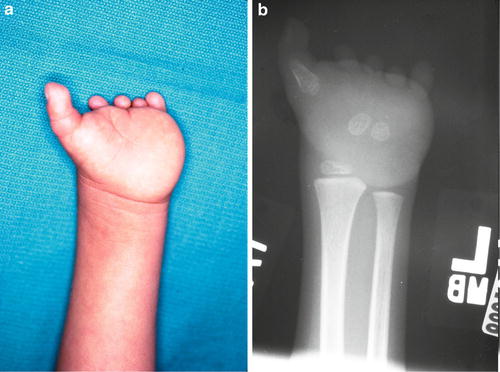
(a–c) Palmar and dorsal views and radiograph of an 8-year-old boy with burns of his left hand resulting in amputation of all five digits
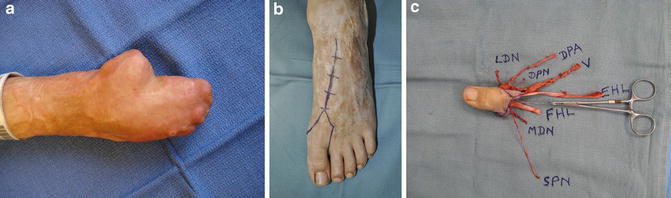
Fig. 8
(a) The thumb-index finger web space was released with full-thickness skin grafts, and the index finger metacarpal was resected to develop a mobile thumb metacarpal as a foundation for a great toe transfer. (b, c) Left great toe transfer
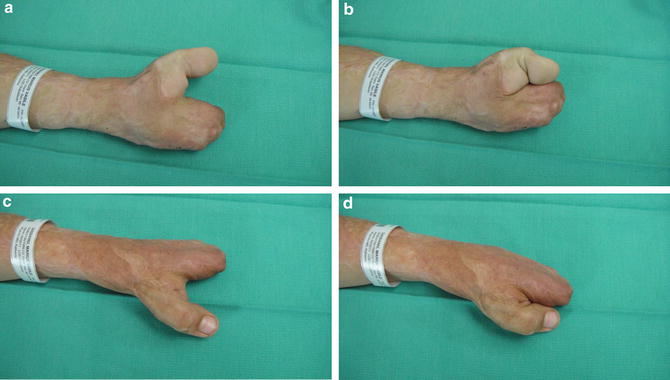
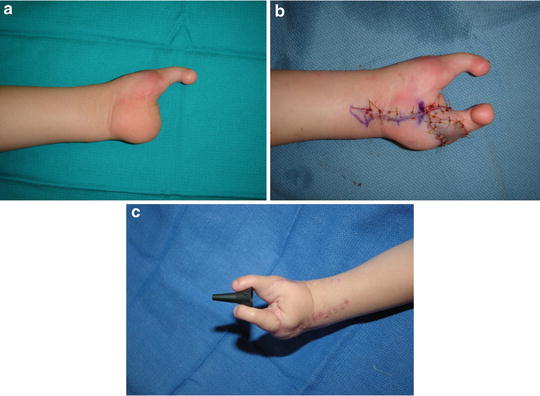
Fig. 9
(a–d) One year following the left great toe-to-left thumb transfer, the child already has pinch between the great toe transfer and the middle finger metacarpal. He subsequently underwent reconstruction of two fingers using a combined second-third toe transfer
The indications for toe transfers for finger reconstruction in children include:
Conventional Reconstruction of Congenital Hand Differences
Conventional non-microsurgical reconstruction of congenital absent digits usually involves pollicization of the index finger for children born with a hypoplastic or absent thumb (Buck-Gramcko 1971; Manske and McCarroll 1985) and nonvascularized toe phalangeal bone grafting (Entin 1959; Carroll and Green 1975; Goldberg and Watson 1982; Buck-Gramcko and Pereira 1990; Radocha et al. 1993; Cavallo et al. 2003; Jones 2004; Gohla et al. 2005; Unglaub et al. 2006) and distraction lengthening (Matev 1970; Kessler et al. 1977; Seitz and Froimson 1991; Ogino et al. 1994; Pensler et al. 1998; Hülsbergen-Krüger et al. 1998; Dhalla et al. 2001; Miyawaki et al. 2002; Matsuno et al. 2004; Seitz et al. 2010) of hypoplastic digits due to symbrachydactyly, cleft hand, or congenital constriction ring syndrome.
Toe-to-Hand Transfers for Congenital Hand Differences
The first microsurgical toe transfer to reconstruct a congenital hand difference was performed by O’Brien et al. (1978) in 1977 who successfully transferred the great toe to reconstruct a hypoplastic thumb in two children. Yoshimura (Yoshimura 1980, 1984) performed 13 toe transfers in 12 children, 10 of whom had sustained traumatic amputations, but 2 had congenital differences – 1 child had an absent thumb, index, and middle fingers, and the second child had congenital constriction ring syndrome involving one finger. May et al. (1981) reported bilateral great toe-to-thumb transfers to reconstruct a 9-year-old boy with bilateral aplasia of his thumb, index, and middle fingers. After other case reports (Nyarady et al. 1983; Meals and Lesavoy 1983), several surgeons have reported larger series of microsurgical toe-to-hand transfers to reconstruct various congenital differences of the hand (Gilbert 1982, 1985; Lister 1988; Eaton and Lister 1991; Shvedovchenko 1993; Vilkki 1995; Kay and Wiberg 1996, Kay and McGuiness 1999; Kay et al. 1996; Van Holder et al. 1999; Foucher et al. 2001; Richardson et al. 2004; Jones et al. 2007; Jones and Kaplan 2013).
Indications for Toe-to-Hand Transfers for Congenital Hand Differences
Microsurgical toe-to-hand transfers for reconstruction of congenital hand differences have not evolved to a similar extent as toe transfers for reconstruction after trauma and remain controversial. Firstly, surgeons may be reluctant to risk the small but potential loss of a toe transfer in a child who is already missing one or more digits in their hands. Secondly, some pediatric hand surgeons still maintain that children with unilateral absence of one of more digits adapt to their impairment as they grow or can be helped with a static or functional prosthesis. Finally, parents may be reluctant to accept a very complicated reconstructive procedure that carries a small risk of ending up with a missing great or second toe as well as more scars on the hand to show for the failed endeavor.
Rather than just showing pre- and postoperative photographs or videos or fabricating moulages, the author’s practice is to arrange for prospective parents to meet the parents of a child with a similar congenital hand difference who has previously undergone a toe transfer, so that the parents can see for themselves the potential function and appearance of the reconstructed hand, as well as speak with the parents about their concerns (Jones 2013).
Very little has been published on the specific indications for microsurgical reconstruction of congenital absent digits. Most pediatricians and even some hand surgeons do not understand which children should be considered for microsurgical reconstruction. Previous reports of toe transfers for congenital hand differences have all been based primarily on the specific embryological diagnoses, according to the classification of the International Federation of Societies for Surgery of the Hand (Swanson 1976). However, it is the authors’ contention that specific indications for toe transfers are more logically defined by the anatomy of the hand anomaly itself, a concept that is also much more easily understood by referring pediatricians and surgeons (Jones 2012). From an analysis of 235 hands in 204 children born with congenital absent digits over a 15-year period, Jones and Kaplan (Jones 2012) developed a simple documentation system, which allows hand surgeons to describe the morphological or radiographic appearance or the functional status of a child’s hand with congenital absent digits, based on which digits are missing and their level of absence. Each hand can be described by three letters R (radial), C (central), and U (ulnar) as well as five numbers. The first letter and number designate which rays are missing, and the second and third letters and numbers designate which rays are present. Consequently, an absent thumb would be designated as R1U4, a hand with a thumb but absent fingers would be designated as U4R1, and complete absence of all five digits would be designated as R5. The spectrum of radial deficiencies includes R1U4, R2U3, R3U2, and R4U1. There are 15 morphological phenotypes of congenital absent digits – the three most common phenotypes being U4R1 (thumb but absence of all four fingers corresponding to the monodactylous type III symbrachydactyly), R1U4 (absent thumb), and R5 (aplastic hand). Unlike most other classifications, this documentation system not only facilitates communication between hand surgeons but also incorporates all the previous subclassification systems that have attempted to describe congenital absent digits in radial, central, and ulnar deficiencies, symbrachydactyly, and congenital constriction ring syndrome. However, most importantly, it has allowed the development of an algorithm that predicts whether conventional or microsurgical reconstruction is indicated for each specific phenotype. Of the 15 phenotypes, only 7 phenotypes are potential indications for microsurgical reconstruction with toe-to-hand transfers: R1U4, R2U3, R3U2, R4U1, R5, U4R1, and occasionally C3R1U1. For a child missing a thumb but with four relatively normal fingers (R1U4), it is intuitive to reconstruct a thumb to oppose to these fingers, either by pollicization of the index finger or by a toe-to-thumb transfer. Similarly for a child missing all four fingers (U4R1), it is logical to reconstruct one or two fingers to allow pinch and grasp to the normal thumb, either by distraction lengthening or by toe-to-hand transfers.
There appear to be four indications for considering microsurgical reconstruction of an absent thumb (Jones 2013; Fig. 10):
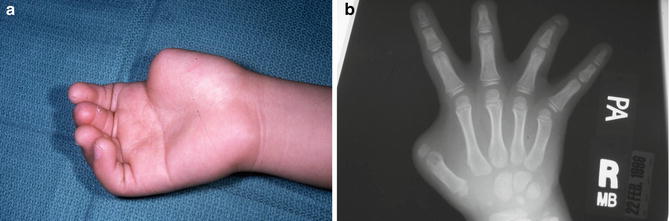
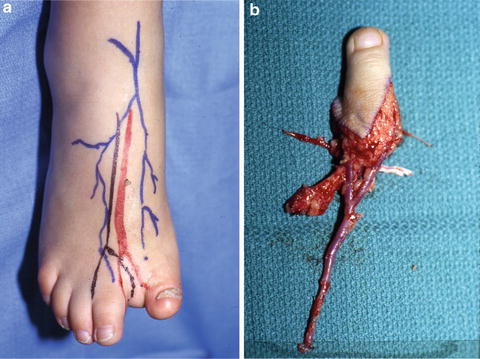

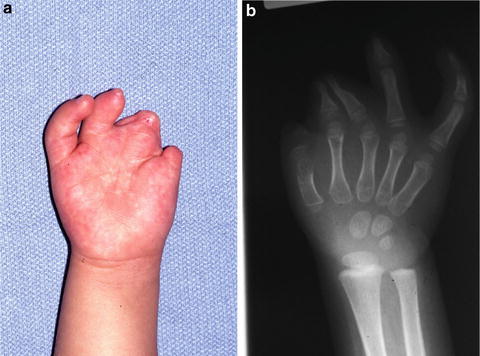
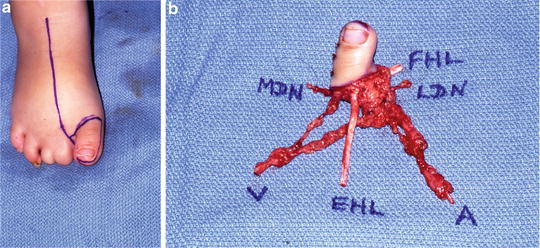

Fig. 10
Schematic representation of the indications for microsurgical toe-to-hand transfers for congenital differences of the hand
(i)
Isolated absence of the thumb with four normal or relatively normal fingers, in which the carpometacarpal joint and base of the thumb metacarpal and thenar muscles are preserved (R1U4). This is usually seen in congenital constriction ring syndrome or occasionally transverse failure (Figs. 11, 12, and 13). Reconstruction of these thumbs with a toe transfer is superior to index finger pollicization, distraction lengthening, or nonvascularized toe phalangeal bone grafting, because it provides greater length and the potential for growth and preserves the full complement of fingers. A second toe transfer in a 2–3-year-old child will provide almost 5 cm length of bone and soft tissue compared with only 13–17 mm length of a nonvascularized toe phalangeal bone graft or 3 cm that can be achieved by distraction lengthening, albeit with a secondary bone graft procedure. If the thenar muscles are poorly developed, an opposition tendon transfer using the flexor digitorum sublimis from the ring finger can be performed primarily at the same time as the toe transfer or at a secondary procedure.
However, if there is an isolated absence of the thumb and four relatively normal fingers, but the carpometacarpal joint is absent, pollicization of the index finger remains the gold standard of reconstruction.
(ii)
Absence of the thumb as well as the index and middle (and ring) fingers but with one or two fingers remaining on the ulnar side of the hand (R2U3, R3U2, and R4U1). This is usually seen with severe radial longitudinal deficiencies or the monodactylous type III atypical cleft hand form of symbrachydactyly (Blauth 1971; Fig. 14). A second toe can be transferred to reconstruct the absent thumb with minimal donor site morbidity, but the modified “wraparound” (Morrison et al. 1980) or trimmed great toe (Wei et al. 1988; Littler 1994) techniques can occasionally be considered in older children to provide both an excellent functional result and a “thumb” very similar in appearance to the contralateral normal thumb (Figs. 14, 15, and 16). If the carpometacarpal joint is absent in these severe radial deficiency phenotypes, the second toe metatarsal can be fixed to the scaphoid or spliced into the radial styloid as described by Vilkki (1989) and by Yu (Yu et al. 1999). Very rarely, a similar morphological deformity also occurs in one or both feet (cleft hand and cleft feet), and the abnormal great toe is sometimes amputated to facilitate the fitting of shoes. In these situations, the abnormal great toe can be transferred to reconstruct the absent thumb (Chang and Jones 2002a).
(iii)
Unilateral (or, extremely rarely, bilateral) absence of the thumb and all four fingers (R5). This is usually seen with the adactylic type IV symbrachydactyly (Blauth and Gekeler 1971) or with transverse failure of formation.
(iv)
Very rare cases in which the thumb or radial side of the hand becomes totally enveloped by a rapidly growing vascular malformation which is unresponsive to embolization or sclerotherapy or by progressive macrodactyly. This situation can potentially be salvaged by radical resection of the thumb but preserving the carpometacarpal joint and base of the thumb metacarpal and thenar muscles, followed immediately by a second toe transfer (Foucher et al. 2001; Carlsen and Jones 2007).
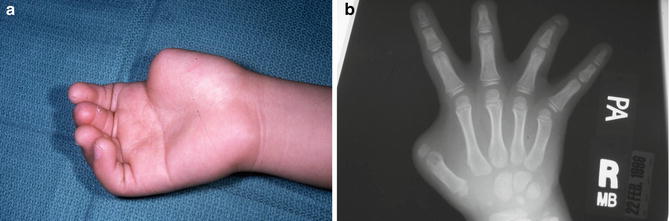
Fig. 11
(a, b) Photograph and radiograph of a 2-year-old girl with congenital constriction ring syndrome affecting her right thumb. The thumb is missing from just distal to the metacarpophalangeal joint, but the thenar muscles are preserved, classified as an R1U4 hand [59]
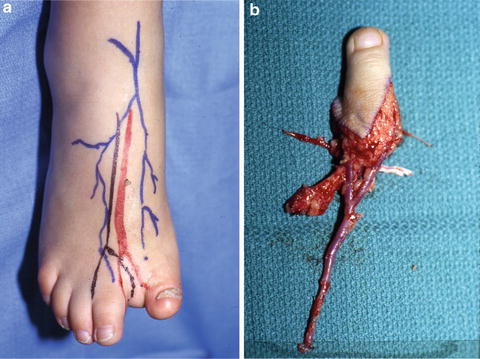
Fig. 12
(a, b) The congenital constriction ring syndrome also caused an above knee amputation of the left lower extremity and an abnormality of the right great toe, so only the right second toe was available for transfer

Fig. 13
Three years postoperatively, the right second toe-to-right thumb transfer has comparable appearance to the normal left thumb and excellent opposition to the small finger
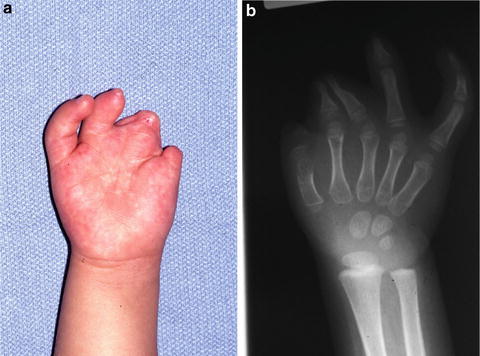
Fig. 14
(a, b) Photograph and radiograph of a 3-year-old girl with severe congenital constriction ring syndrome affecting her right thumb, index, middle, and ring fingers. The thumb is missing from just distal to the metacarpophalangeal joint, but the thenar muscles are preserved and the ring and small fingers remain relatively functional
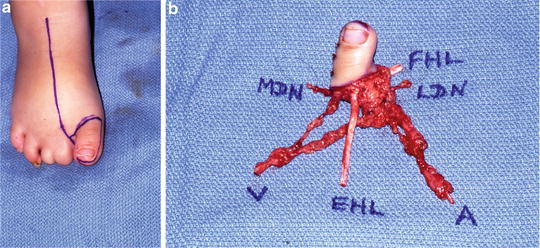
Fig. 15
(a, b) Because the second and third toes in both feet were affected by the congenital constriction ring syndrome, a right “trimmed” great toe transfer was designed for reconstruction of the thumb

Fig. 16
Two years postoperatively, the right “trimmed” great toe-to-right thumb transfer has comparable appearance to the normal left thumb and excellent opposition to the only normal small finger
There appear to be two indications for considering toe transfers to reconstruct absent fingers (Jones and Kaplan 2013; Fig. 10):

(i)
Absence of all four fingers (from the carpus out to the base of the middle phalanges) but with a normal thumb (U4R1). This is usually seen with the monodactylous type III symbrachydactyly, transverse failure of formation, congenital constriction ring syndrome , or severe ulnar longitudinal deficiency (Figs. 17 and 18). The location into which the toe is transferred depends on the anatomy. Microsurgical reconstruction of a finger can be accomplished by a single second toe transfer into the middle, ring, or small finger position. Placement of the toe transfer on the ulnar side of the hand allows both grasp of large objects as well as tip-to-tip pinch (Fig. 18b, c). An alternative option if the parents are agreeable is to transfer two second toes, either simultaneously or sequentially, into the middle and small finger positions to allow three-point pinch (Figs. 19, 20, and 21). Occasionally, if the parents are willing to accept the appearance of the donor foot, combined second and third toes can be transferred into the middle-ring or ring-small finger positions. The range of motion of a toe transfer used for reconstruction of a finger depends on whether there is an existing metacarpophalangeal joint in the hand. If the proximal phalanx of a toe transfer can be fixed to a remnant of the proximal phalanx of a finger, excellent motion can be expected at the existing metacarpophalangeal joint, whereas if the metatarsal of a toe transfer has to be fixed to a metacarpal in the hand, the motion achieved at the metatarsophalangeal and proximal interphalangeal joints is considerably less.
(ii)
Complete absence of all five digits (R5). This is usually seen in the adactylic type IV symbrachydactyly (Blauth 1971) or transverse failure of formation (Fig. 22). Reconstruction may be accomplished using two second toe transfers into the thumb and ring or small finger positions to provide grasp and tip-to-tip pinch. This can be performed simultaneously but is probably better performed sequentially, so that positioning of the second transfer into a finger position can be adjusted to the position and mobility of the first transfer into the thumb position (Figs. 23 and 24).
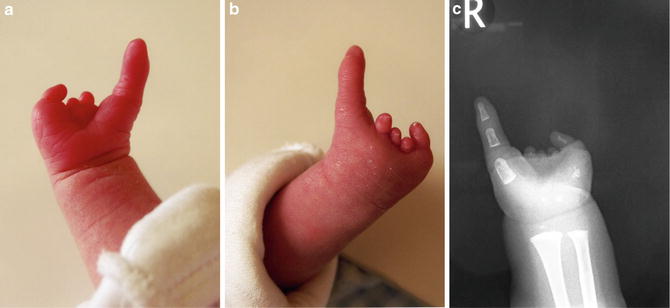
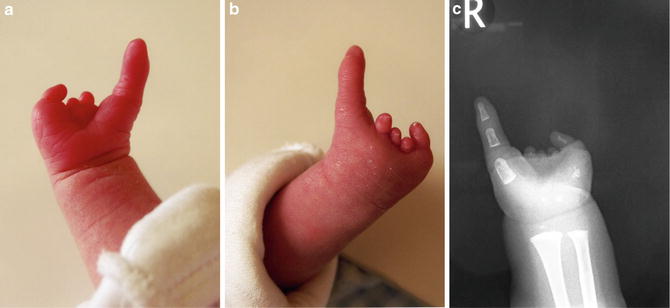
Fig. 17
(a–c) Palmar and dorsal photographs and radiograph of a 6-month-old baby girl with symbrachydactyly of her right hand, with a normal thumb but absence of all four fingers which are just represented by nubbins, classified as a U4R1 hand [59]
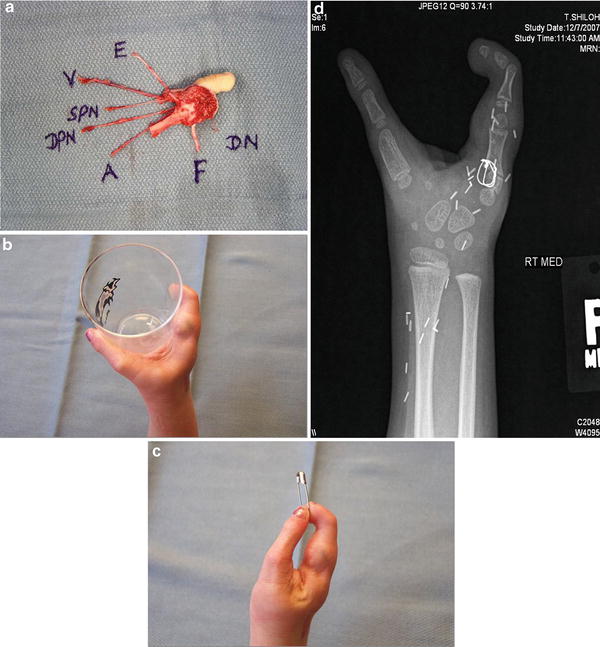
Fig. 18
(a) Second toe transfer performed at 2 years of age. (b, c) Five years after a second toe-to-small finger transfer, the child has excellent grasp and very precise pinch between the thumb and second toe transfer. (d) The postoperative radiograph shows 90-90 interosseous wire fixation of the second toe metatarsal to the base of the small finger metacarpal
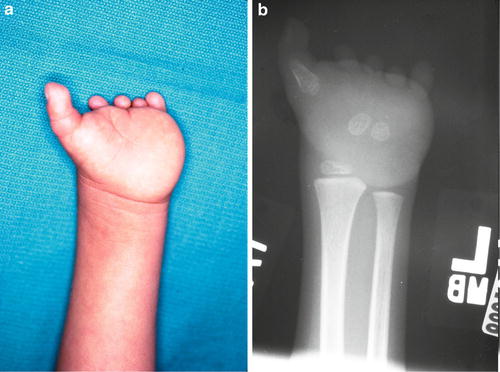
Fig. 19
(a, b) Photograph and radiograph of a 2-year-old boy with symbrachydactyly of his left hand. The thumb is present, but all four fingers are absent and just represented by nubbins, classified as a U4R1 hand [59]
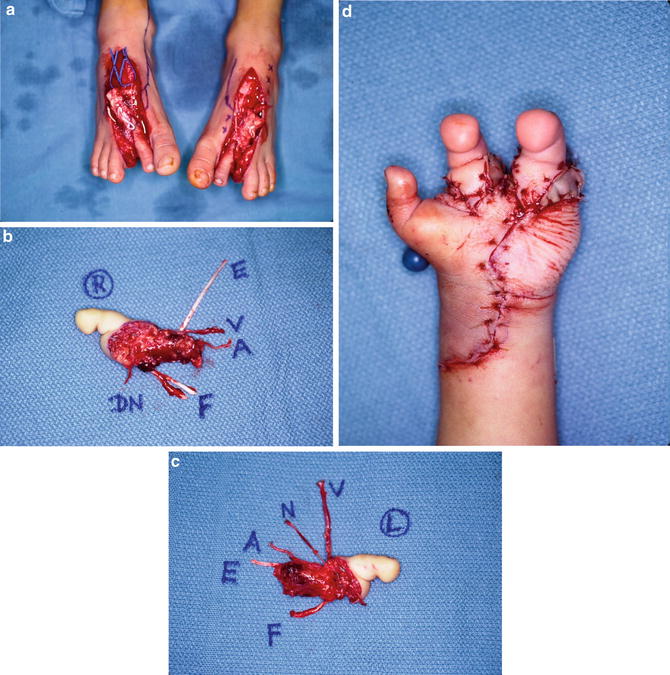
Fig. 20
(a–d) Simultaneous bilateral second toes were transferred into the middle and small finger positions
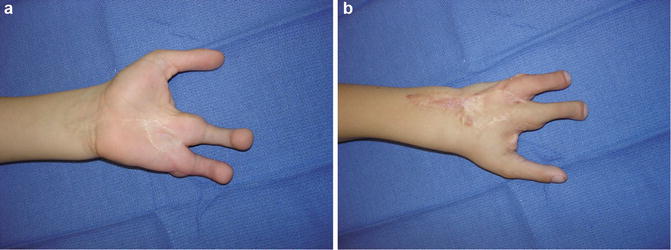
Fig. 21
(a, b) Seven years postoperatively, both “fingers” have normal sensation and continue to grow and provide three-point pinch with the mobile thumb
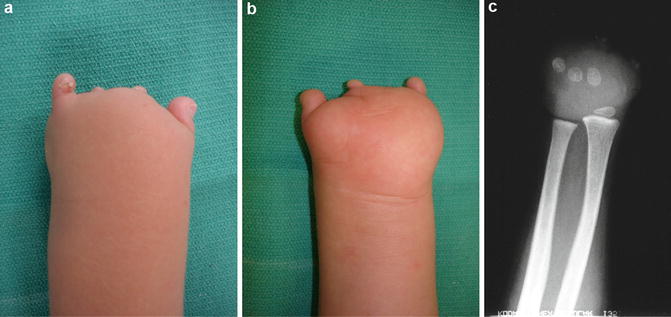
Fig. 22
(a–c) Dorsal-palmar photographs and radiograph of a 2-year-old boy with symbrachydactyly affecting all five digits of his left hand. The digits are missing from the level of the metacarpal bases; classified as an R5 hand (Jones and Kaplan 2012)
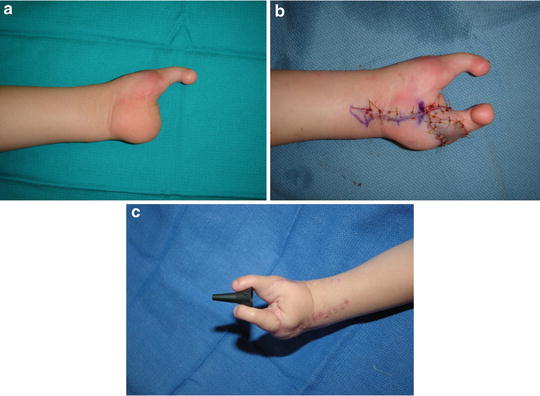
Fig. 23
(a–c) The child underwent staged second toe transfers, firstly into the thumb position (a) and 6 months later into the small finger position (b). Six weeks postoperatively (c), demonstrated by the presence of remaining skin sutures and before the child has regained any sensation in the second toe transfer, he is already able to pinch between the two toe transfers just by visualizing his hand

Fig. 24
(a, b) Six years postoperatively, the child demonstrates excellent ability to pick up small objects by side-to-side pinch between the two second toe transfers and strong grasp to lift up a heavy bottle
Timing of Toe Transfers for Congenital Hand Differences
The optimal age for performing a toe transfer to reconstruct a congenital hand difference has not been defined. Generally, the earlier that a toe transfer is performed, the better the chance of cortical integration. Children with a unilateral congenital hand anomaly should probably be reconstructed at an earlier age, before the use of the contralateral normal hand dominates. However, the real limiting factor in pediatric toe transfers is the size of the donor and recipient vessels, which must be of adequate size to facilitate the microsurgical anastomoses. Gilbert (1982, 1985) and Lister (Lister 1988) have performed toe transfers in children as young as 6–12 months of age, but toe transfers have also been successful in older children between 11 and 17 years of age (Spokevicius 1997). The senior author usually performs toe transfers between 2 and 3 years of age.
Preoperative Assessment of a Child for a Toe-to-Hand Transfer
After a traumatic injury to a child’s hand, there is always some blame, either attached to or accepted by one of the parents. The parental response to a child born with a congenital hand difference resembles the bereavement response. Each parent must deal with their own sense of loss, as well as the obligation to direct the treatment of their child. Listening to the child’s parents and allowing them to express their understanding of their child’s condition and their hopes and expectations for reconstruction are vitally important. Some surgeons have recommended that the parents and child meet with a clinical psychologist prior to considering a toe-to-hand transfer, and it has been documented that psychological counseling may play an integral role in decision-making in pediatric hand surgery (Bradbury et al. 1994). The parents should be prepared psychologically for the substantial amount of time and energy that will be required during the pre- and postoperative period. In addition, they must understand and accept the fact that a toe transfer can fail, leaving the child with the same deficit in the hand but also now missing a toe in the foot. If the parents and/or child cannot accept the time commitment and the potential risk of failure, this surgery should not be considered.
Usually with congenital hand differences, the child will have been examined by a pediatrician for other congenital anomalies and possibly even by a geneticist to exclude any syndrome. A detailed examination of the involved upper extremity should be performed or if the child is very young, observed while playing. More proximal shoulder or elbow abnormalities should be excluded such as Poland’s syndrome or radial-ulnar synostosis. The presence or absence of a radiocarpal joint as well as the number and length of any metacarpal bones should be determined. The presence or absence of a thumb and whether there is a thumb carpometacarpal joint are important if a toe-to-thumb transfer is being considered. Dimpling of the skin in symbrachydactyly may indicate the presence of flexor tendons in the vicinity of the nubbins.
One or other of the child’s feet may be positioned close enough to the affected hand, so that the parents and/or child can visualize what the transferred toe might look like. Occasionally, congenital anomalies of the lower extremities may coexist with upper extremity anomalies and especially with bilateral congenital hand differences; the availability of donor toes may be limited because of associated foot anomalies.
Plain radiographs of both hands and both feet should be obtained to determine the presence of metacarpals and whether a carpometacarpal joint of the thumb is present or absent. In children where the carpal or metacarpal bones have not yet ossified, an MRI scan may be considered.
The necessity for preoperative angiography of either the upper or lower extremity remains controversial. Greenberg and May (1988) found a preoperative lateral angiogram of the foot to be helpful in identifying the location and size of the first dorsal metatarsal (FDMA) and first plantar metatarsal arteries (FPMA). The author no longer obtains angiograms but listens to the dorsalis pedis and first dorsal metatarsal artery in both feet with a handheld Doppler probe. The dorsalis pedis artery can be traced distally into the first dorsal metatarsal artery lying between the great toe and second toe metatarsals using an 8 MHz pencil Doppler ultrasound probe. The dominance of the FDMA can be assessed from the presence or absence of a Doppler signal and the potential depth of the FDMA from the intensity of the signal (superficial, within, or deep to the interosseous muscles).
A final preoperative evaluation should always be performed by the child’s pediatrician a few days prior to any toe-to-hand transfer to exclude any viral infection, which might compromise postoperative respiratory function after a multi-hour operation.
Anatomy of the Great Toe and Second Toe
The arterial anatomy of both the great toe and the second toe is based on either the first dorsal metatarsal artery (FDMA), a continuation of the dorsalis pedis artery, or the first plantar metatarsal artery (FPMA) (Villen and Julve 2002). Superficial veins drain to the medial side of the dorsum of the foot and then into the greater saphenous vein. Sensibility to the plantar surface of the great toe or second toe is provided by the tibial (medial) and fibular (lateral) digital nerves and to the dorsal surface by the deep peroneal nerve.
Surgical Technique
The child is positioned supine with the arm and hand on a hand table and the donor foot at the end of the operating table. General anesthesia is occasionally supplemented with an axillary block or continuous brachial plexus infusion. A Foley catheter is used to monitor urine output and fluid status, but central venous catheters are not used routinely. A regular tourniquet is applied to the upper arm, and a sterile tourniquet is applied to the thigh, since a skin graft may need to be harvested later from the thigh or groin.
Toe-to-hand transfer |
|---|
Preoperative planning for all procedures |
OR table: any table for supine position |
Positioning/positioning aids: supine with the arm and hand on a hand table and the donor foot at the end of the operating table |
Equipment: basic and microsurgical instruments, microscope, tourniquets |
Toe-to-hand transfer |
|---|
Surgical steps – donor foot |
8 MHz Doppler ultrasound probe is used to mark the location of the dorsalis pedis artery and/or the posterior tibial artery |
Location of suitable dorsal veins may be marked by inflating the thigh tourniquet to 100 mmHg after the draping |
Leg elevated but not exsanguinated and the tourniquet elevated to 300 mmHg |
Racquet-shaped incision is used to harvest the great toe, or a V-shaped incision is used to harvest the second toe |
Dorsal incision is extended to the level of the extensor retinaculum |
Draining veins are dissected in a distal-to-proximal direction to a dominant dorsal vein |
The extensor hallucis longus (EHL) tendon to the great toe or the extensor digitorum communis tendon (EDC) to the second toe is dissected in a distal-to-proximal direction and transected at the level of the extensor retinaculum |
Deep peroneal nerve is identified proximally by dividing the extensor hallucis brevis tendon and traced in a proximal-to-distal direction isolating the fascicles supplying either the great toe or the second toe, which are divided from the main deep peroneal nerve |
Find the first dorsal metatarsal artery (FDMA) distally in the web space between the great toe and second toe. The FDMA may lie in a superficial dorsal, intramuscular, or plantar position in relation to the interosseous muscles |
A communicating branch between the FDMA and the first plantar metatarsal artery (FPMA) may be visualized passing over and distal to the intermetatarsal ligament. The ligament is divided, and the FPMA is dissected further proximally through the plantar incision |
If the second toe is being transferred, the fibular digital artery to the great toe is ligated and divided. If the great toe is being transferred, the tibial digital artery to the second toe is ligated and divided |
Select the dorsal or plantar arterial system depending upon which is dominant |
The flexor hallucis longus tendon to the great toe or the flexor digitorum longus and flexor digitorum brevis tendons to the second toe are identified through the plantar incision and are divided as far proximally as possible |
The tibial and fibular plantar digital nerves are traced proximally to their bifurcation from the common digital nerves. The common digital nerves to the great toe-second toe web space and the second-third toe web space are split more proximally using micro-forceps and micro-scissors before transecting the tibial and fibular digital nerves to either the great toe or second toe
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|