Fig. 43.1
A midline neck mass illustrating the typical presentation and position for a thyroglossal duct cyst
A TGDC can enlarge several centimeters in size but on presentation they are typically pea size to 2 cm. They are commonly firm but not solid or soft on palpation. They may be freely mobile under the skin and classically elevate on swallowing. TGDC can develop a variety of secondary features. The thyroid’s embryological relationship with the tongue makes a cyst susceptible to infection from microbes that enter the tract from the oral cavity. Infection has been reported in up to 50 % of cases [13]. Infected cysts may present as an abscess with inflammation and tenderness. TGDC do not typically communicate with the skin, but infection can lead to the development of a draining fistula [14].
Differential Diagnosis
The majority of neck masses in the pediatric population have a congenital or infectious etiology. Despite being a common cause for a midline neck mass in the child, TGDC have a broad differential diagnosis. Even after proper clinical evaluation, other masses such as lymph nodes and thyroglossal carcinomas have been misdiagnosed as TGDC [9, 15]. The wary physician must always consider the full range of diagnostic possibilities when accessing any neck mass in a child. The most important lesion to distinguish from a TGDC is a median ectopic thyroid gland. Most patients with an ectopic thyroid gland will have their entire functioning tissue located in an aberrant midline location [4]. Removal will result in lifelong hypothyroidism so care must be taken during the evaluation to rule out this possibility.
Dermoid cysts can also be readily mistaken for TGDC [5, 9]. They can present midline in the same locations as a TGDC and may also have the same consistency on palpation. Unlike TGDC, dermoid cysts do not move with swallowing. Other midline considerations include lymph nodes, branchial anomalies, lipomas, lymphatic malformations, and ranulas [5, 9, 16].
Diagnosis and Evaluation
Physical Examination
The classical TGDC is not soft or hard, but is firm and usually midline (Fig. 43.2). A complete head and neck examination should be performed on all patients. The clinician should inspect the base of the tongue and floor of mouth with visual and bimanual palpation. Ranulas and lingual thyroids can often be ruled out in this manner. Next the neck should be palpated on both sides. This is classically done from the rear of the patient using a hand on each side of the neck and systematically checking each neck level, including the midline. In a very young patient, the behind the neck approach may not be feasible. Care should be taken to check for masses in the submandibular spaces and along the jugular digastric chain. Midline masses should be palpated with both hands and the patient should be asked to swallow to see if the mass elevates and descends with deglutition. This finding may be difficult to observe in some pediatric patients. Although not always possible, it is advisable to try and palpate the thyroid gland to determine if it is in its normal location. If the mass is small or changing in size, it may be difficult to locate on the first evaluation. If the mass cannot be located, it is important to have the patient or their guardian/parent show the physician where the area of concern is after the examination is complete. TGDC do not commonly reduce in size or disappear. If this occurs with a suspected TGDC, the diagnosis should be in question. Unless the cyst has been infected and drained spontaneously, there is usually not a fistulous opening to the skin.
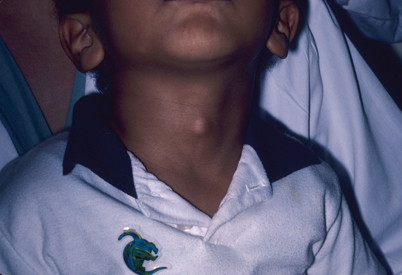
Fig. 43.2
Any midline neck mass should raise suspicion for a thyroglossal duct cyst
Laboratory Data
Most midline neck masses, including TGDC, do not require any laboratory data prior to removal. Most patients will be euthyroid and rarely will the TSH or other thyroid function tests (TFT) show any abnormalities. TFT should be ordered in cases where the presumed TGDC is an ectopic thyroid gland or if the patient appears clinically hypothyroid [9, 16]. In the healthy child without other comorbidities, other laboratory testing will typically be normal and not necessary prior to treatment.
Imaging Evaluation
The presence of a TGDC implies that normal thyroid decent has occurred. The main goal and advantage of any imaging is to document that the thyroid gland is indeed located in its usual location and not ectopic. While many ectopic thyroid glands will eventually require removal, it serves the surgeon well to advise the patient or their guardians of this possibility prior to surgery [14].
In the past many practitioners relied on thyroid scans to document the actual location of the thyroid gland and any ectopic functioning thyroid tissue [17]. Thyroid scans are accurate, but require intravenous access, time, and patience on the part of the patient. They may involve separate evaluations and appointments. Sedation may also be necessary in young children. In recent years, ultrasound (U/S) has replaced thyroid scans in many institutions [8, 14, 18]. U/S has the benefit of documenting the presence of a normal thyroid gland as well as locating the TGDC (Figs. 43.3, 43.4). It is not time consuming and does not expose the patient to radiation. It usually can be scheduled quickly, sometimes on the day of the primary evaluation. Although other midline anomalies can be discerned with U/S, at times it can be misleading. For example, in young infants a large thymus gland can protrude up into the neck and masquerade as a normal thyroid gland on U/S. The senior author has had this occur twice in 25 years of practice.
Fig. 43.3
U/S imaging documenting the location of the thyroid gland (arrows)
Fig. 43.4
U/S showing the typical location of a thyroglossal duct cyst (arrow)
Some have used computed tomography (CT) scanning with contrast to evaluate a TGDC (Fig. 43.5a, b). This is typically not necessary unless the physician senses some other pathological process that U/S could not properly evaluate. CT scanning with contrast may be of help when accessing a reoccurring TGDC [18]. Extra tracts or other diagnostic possibilities can at times be better delineated on CT scans. Like thyroid scans, sedation or general anesthesia might be necessary in select patients.
Fig. 43.5
a, b CT scan with arrows indicating the location of a thyroglossal duct cyst
Pathology
The pathology of a TGDC is straightforward. The cystic tract is lined by either squamous or pseudostratified ciliated columnar epithelium (Fig. 43.6) [19]. Inflammatory cells and thyroid follicles may also be present [20]. Confirmation of the correct diagnosis is mandatory to avoid postoperative complications. If there is any question of a possible ectopic thyroid gland during surgery, an intraoperative frozen section should be obtained. If the frozen section reveals thyroid glandular tissue or colloid follicles without any cystic components, it is imperative to obtain a thyroid scan in the postoperative period to document that an actual functioning thyroid gland exists. The surgeon may also opt to explore the area where the thyroid gland should be located to see if a gland is present.
Fig. 43.6




Thyroglossal duct cyst, midline neck. a Large soft tissue cyst lined by well-formed respiratory ciliated epithelium (arrowheads) containing sloughed surface epithelial cells, cellular debris, inflammatory cells, and mucus. b Higher magnification of ciliated respiratory epithelium (detail from area indicated by arrowheads in a). c Ectopic islands of thyroid tissue with well-formed follicles (between arrows). d Thyroglossal duct remnant (between arrows) adjacent to hyoid bone
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


