Fig. 1
A 14-year-old female with pain and right thoracic outlet syndrome attributed to cervical rib. The patient has decreased right arm abduction secondary to pain (Courtesy of Shriners Hospital for Children, Philadelphia)
Symptoms of venous TOS typically arise in patients who repeatedly exert their upper extremity with the arms above shoulder level. Fatigue of the affected forearm may occur within minutes of use. Swelling accompanied by pain and/or cyanosis is a common manifestation of venous TOS and may lead to paresthesias in the digits (Fig. 2a). Collateral veins that are visible in the skin around the affected shoulder, neck, and chest wall may develop due to venous compression (Marine et al. 2013; Fig. 2b). Additionally, due to the diameter of the veins being decreased and flow being interrupted (stasis), spontaneous upper extremity venous thrombosis (Paget-Schroetter syndrome) may develop (Urschel and Razzuk 1991).


Fig. 2
An 18-year-old male who presented with complaints of pain in the right arm after working as short-order cook. (a) Swollen right arm with venous congestion present due to venous thoracic outlet syndrome. (b) Presence of distended veins (Courtesy of Shriners Hospital for Children, Philadelphia)
Compression of the arteries within the thoracic outlet is virtually always associated with a cervical or anomalous rib. Arterial TOS is extremely rare, and symptoms develop spontaneously, commonly in young patients with little or no risk factors for atherosclerosis. Clinical manifestations of arterial TOS are typically caused by arterial thromboembolism and include symptoms of hand and finger ischemia, including pain, pallor, paresthesias, and coldness. Arterial thromboembolisms most often develop from mural thrombus of the subclavian artery. Rarely, a thrombus from the subclavian artery can embolize in a retrograde fashion causing a stroke (Desai and Robbs 1995; Lee and Hines 2007).
Distal nerve compression in association with TOS has been suggested as a cause of double-crush syndrome. Carpal tunnel syndrome has been reported in 21–45 % of patients with TOS, and cubital tunnel syndrome has been seen in up to 10 % of cases (Leffert 1992; Lishman and Russell 1961; MacKinnon 1992; Putters et al. 1992). The double-crush theory remains controversial. Opponents of the double-crush theory propose that the wide range of variable symptoms is due to nerve compression at a single site, based on symptom relief achieved following surgery at one location (Carroll and Hurst 1982).
Due to the chronic, unremitting nature and clouded differential diagnosis of TOS, patients may experience continued psychological stress. Numerous tests and physical examinations may be performed, furthering the psychological strain on patients. Depression, anxiety, anger, and frustration can become more visible as symptoms persist without a definitive diagnosis (Jamieson and Merskey 1985; Luoma and Nelems 1991). Therefore, psychological evaluation and treatment should be available for any patient who exhibits signs of psychological stress.
Physical Examination
Although the history of patients with TOS is often nonspecific, physical examination is diagnostic in up to 97 % of patients (Rayan 1998). Physical examination should begin with observation of the patient’s habitus and assessment of any visible asymmetry. Slouching, shoulder droop, and scapular asymmetry are clues that may lead to a diagnosis of TOS but could also represent alternative pathologies. The skin over the chest wall, neck, and shoulder girdle should be examined for the presence of venous engorgement or collateral sprouting. Muscle tone and bulk should be evaluated via palpation with and without resistance, especially in the neck, upper back, shoulder, arm, forearm, and hand. A sensory examination should be performed utilizing two-point discrimination and Semmes-Weinstein monofilaments, as well grip and pinch measurements. Blood pressure measurements in both arms, as well as auscultation of the subclavian arteries, should be performed to assess for thromboembolism or aneurysm. In a study by Braun and colleagues, pulse oximetry measurements in patients with symptomatic TOS were compared with measurements taken in a control group prior to and after a provocative maneuver. Oxygen saturation dropped to 86 % in the symptomatic TOS group while only dropping to 94 % in the control group. Therefore, it was concluded that pulse oximetry may be a quick and inexpensive tool to aide in the diagnosis of thoracic outlet syndrome (Braun et al. 2012).
The hallmark of the physical examination for thoracic outlet syndrome is the performance of provocative tests. Positive results are documented if a maneuver either reproduces the patient’s symptoms or diminishes/obliterates the radial pulse. Several historically utilized maneuvers such as Adson’s, Wright’s, and Halstead’s tests are less commonly performed due to their lack of sensitivity and specificity for TOS (Gillard et al. 2001).
The Roos’ test (90° abduction external rotation test, stickup test, elevated arm stress test [EAST]) involves the patient holding the affected arm in an abducted and externally rotated position while repeatedly pumping the hand open and closed for 3 min. Symptoms and rapid fatigue are indicative of a positive test. The test may be poorly tolerated in patients with positional nerve compression. This maneuver is often considered the most sensitive test for thoracic outlet syndrome (Roos 1990).
The upper limb tension test involves the patient elevating both arms out to the sides with elbows straight and head facing forward. The patient’s wrists are then extended, and the head is tilted away from the affected side. When this test is positive, the patient reports increasing discomfort or paresthesias due to the increasing tension on the brachial plexus (Sanders et al. 2007).
Imaging and Other Diagnostic Studies
Several imaging modalities may be utilized in the workup of thoracic outlet syndrome. Initial radiographs of the cervical spine and chest should be obtained at the time of first evaluation to assess for the presence of an elongated C7 transverse process or cervical rib on the affected side (Wilbourn 1999; Fig. 3). Fibrous bands associated with abnormal cervical ribs are radiolucent and therefore are better visualized on MRI (Panegyres et al. 1993).
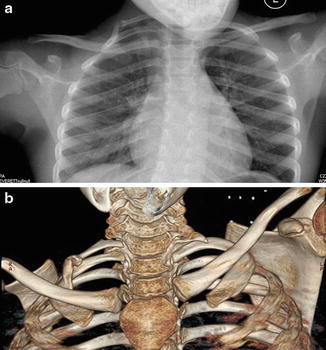
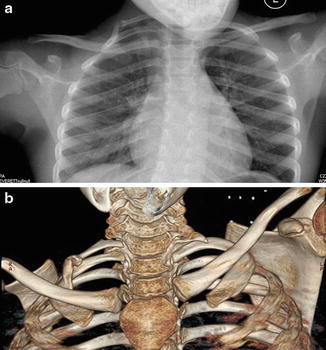
Fig. 3
(a) Chest radiograph demonstrates cervical rib on the right side with intervening synchondrosis. (b) CT scan better delineates the cervical rib and synchondrosis (Courtesy of Shriners Hospital for Children, Philadelphia)
Ultrasonography is often utilized in patients with vascular pathology due to its low cost and ease of use. Color duplex ultrasonography is highly sensitive and specific when diagnosing stenosis, occlusion, and/or flow abnormalities (Demondion et al. 2006; Wadhwani et al. 2001). Pulse volume recordings can be used to evaluate arterial compression and can be followed up by MR angiography or arteriography (Kleinert and Gupta 1993).
Angiography provides the best visualization of the arterial anatomy and is considered the gold standard for the diagnosis of arterial TOS. MR angiography is noninvasive, but conventional angiography allows for simultaneous therapeutic thrombolysis in an acute scenario (Ohkawa et al. 1992; Sharafuddin et al. 2002). The bony anatomy should be carefully assessed, as bone anomalies are the most common cause of arterial compression.
In cases of suspected venous TOS, venography is the gold standard. The patient may be asked to perform a provocative maneuver while imaging takes place, as this may be diagnostic for venous compression from TOS. As with angiography, thrombolysis can also be achieved during venography if necessary. Additionally, collateral vein sprouting may be visible on venography (Sharafuddin et al. 2002).
Electrodiagnostic evaluation is recommended in patients with suspected neurogenic TOS as part of the initial workup. In patients with symptomatic neurogenic TOS, electromyographic (EMG) changes showing chronic denervation of the intrinsic hand muscles are the initial abnormalities observed, while nerve conduction velocity changes are not seen until late in the disease (Marcaud and Métral 2000; Passero et al. 1994).
Classification Scheme
A scheme was introduced by Roos that classified TOS based on the affected segment(s) of the brachial plexus. These categories include upper trunk compression, lower trunk compression, and combined compression. Eighty-five to ninety percent of his patients exhibited symptoms of lower trunk and/or combined compression (Roos 1982).
Wilbourn categorized thoracic outlet syndrome into two basic types, each with two subtypes (Wilbourn 1999). Vascular TOS is subdivided into arterial and venous, while neurogenic TOS is subdivided into true, or electrically positive, and disputed, or electrically negative.
Outcome Tools
There are no validated outcome measures to specifically assess thoracic outlet syndrome outcomes. Several quality of life scores, including the Cervical Brachial Symptom Questionnaire (CBSQ), the Brief Pain Inventory (BPI), and the Short-Form 12 (SF-12), have been utilized to evaluate long-term TOS outcomes following operative intervention. Additionally, functional outcomes following surgical repair of TOS have been measured utilizing the Disability of Arm, Shoulder, and Hand (DASH) score (Rochlin et al. 2012, 2013).
Nonoperative Treatment
Nonoperative management is universally agreed upon as the first-line treatment of thoracic outlet syndrome. The goal is to alleviate the compression of the thoracic outlet as well as avoidance of exacerbating factors (Leffert 1992; Novak et al. 1993; Table 1).
Table 1
Thoracic outlet syndrome | |
|---|---|
Nonoperative management | |
Indications | Contraindications |
All suspected cases of TOS | The presence of a mass |
Acute arterial or venous thrombosis | |
Techniques
Supervised postural training and exercises directed at strengthening the parascapular muscles and widening of the thoracic outlet are the strategy for patients with poor posture. Additional exercises aimed at strengthening the muscles of the shoulder girdle, stretching the scalene muscles, and relaxing the first rib can be performed. These exercises should attempt to expand the thoracic outlet so that the brachial plexus can pass unobstructed (Atasoy 1996; Pratt 1986).
For women with macromastia, better breast support may improve symptoms. Reduction mammoplasty may be warranted in severe cases, although this treatment remains controversial (Iwuagwu et al. 2005; Kaye 1972; Leffert 1992). Decreasing overhead activity and reducing downward force on the shoulder girdle through ergonomic modification can also be helpful. Symptomatic improvement is achieved in the majority of TOS patients treated without surgery. Only 10–30 % of TOS patients will progress to becoming surgical candidates (Oates and Daley 1996; Sanders et al. 1979; Selke and Kelly 1988; Thompson and Petrinec 1997; Thompson et al. 1997).
Operative Treatment
Indications/Contraindications
Indications for surgical treatment include intractable pain, neurologic deficits, vascular compromise, the presence of a mass or abnormal anatomy, or failure of nonoperative treatment (Oates and Daley 1996; Sanders et al. 1979; Selke and Kelly 1988; Thompson and Petrinec 1997; Thompson et al. 1997).
Surgical Objective
The goal of operative management is decompression of the neurovascular structures within the thoracic outlet. A variety of procedures and approaches have been proposed, and there is no consensus on which procedure is the gold standard. Procedures include the following in isolation or combination: cervical rib resection, first rib resection, scalenotomy, scalenectomy, anomalous fascial band excision, claviculectomy, and pectoralis minor release.
Preoperative Planning
See Table 2.
Table 2
Thoracic outlet syndrome |
|---|
Preoperative planning |
OR table: standard OR table |
Position/positioning aids: variable depending upon the approach |
Fluoroscopy location: unnecessary |
Equipment: Spurling Kerrison rongeur, chest tube |
Tourniquet (sterile/nonsterile): none |
Draping: entire arm and hemithorax to contralateral sternoclavicular joint |
Positioning
The position of the patient will vary according to the surgical approach. The patient may be supine, lateral decubitus, or in the beach chair position. The arm is prepped and draped within the sterile field. All bony prominences are meticulously padded.
Surgical Approach
There is currently no universally accepted approach for operative treatment of thoracic outlet syndrome (Oates and Daley 1996). Several approaches have been described including a supraclavicular, transclavicular, subclavicular, transaxillary, posterior, and a combined approach.
First rib resection , with or without anterior scalenectomy, is most commonly performed for TOS (Leffert 1992; Oates and Daley 1996; Roos and Owens 1966, 1982). The rare upper plexus TOS can be managed via isolated scalenectomy, where 80–90 % of the anterior scalene muscle and 40–50 % of the middle scalene muscle are excised (Alnot 1995; Sanders et al. 1979; Thompson and Petrinec 1997). The supraclavicular approach is commonly utilized for scalenectomy and upper plexus exploration but may limit the exposure of the first rib (Thompson et al. 1997).
Removal of the first thoracic rib can alleviate several potential sites of compression as the first rib acts as a fulcrum for T1, a site of attachment for the scalene muscles, and also borders the costoclavicular space. The transaxillary approach provides the greatest access to the first rib and is cosmetically more appealing but sacrifices the possibility of scalenectomy and upper plexus exploration (Alnot 1995; Karamustafaoglu et al. 2011; Thompson and Petrinec 1997). The transaxillary approach can be utilized for removal of cervical ribs, and the pectoralis minor tendon can be divided if subcoracoid compression is suspected. A supraclavicular and transaxillary combined approach may be useful in recurrent or complicated cases (Qvarfordt et al. 1984).
Technique
First rib resection utilizing the supraclavicular approach is performed via a transverse incision just above the clavicle. The incision extends from the sternocleidomastoid to the anterior edge of the trapezius. Cutaneous nerves are mobilized and the platysma incised. The external jugular vein is ligated and the underlying omohyoid identified and retracted. The omohyoid is the “door” to the supraclavicular plexus. The fat pad is mobilized to reveal the underlying plexus. The anterior and middle scalene muscles are identified. The phrenic nerve is visualized lying on the anterior surface of the anterior scalene.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


