Name
Number
Description
Gene(s)
Hypermobility
Type 3
Type 3 presents with joint hypermobility and chronic musculoskeletal pain with associated frequent subluxations and dislocations
COL3A1 TNXB
Classical
Types 1 and 2
Type 1 typically presents with severe skin involvement, and type 2 presents with mild to moderate skin involvement. Patients with the classical type may experience similar joint symptoms as the hypermobility type but with more skin involvement
COL5A1, COL5A2, COL1A1, ADAMTS2
Vascular
Type 4
Type 4 typically is the most serious type because blood vessels and organs are fragile and prone to rupture
COL3A1
Kyphoscoliosis
Type 6
Type 6 is very rare characterized by progressive kyphoscoliosis, fragile eyes, and muscular weakness
PLOD1
Arthrochalasia
Types 7A and B
Types 7A and B are exceedingly rare and present with extreme joint hypermobility and bilateral hip dislocations
COL1A1, COL1A2
Dermatosparaxis
Type 7C
Type 7C is exceedingly rare and is characterized by extremely fragile, sagging skin
ADAMTS2
Ligamentous laxity syndromes have also been linked to additional musculoskeletal disorders (Mishra et al. 1996). Carpal tunnel syndrome has been noted to be more frequent in patients with hypermobility syndromes (Aktas et al. 2008), with the causative factor felt to be the increased wrist range of motion leading to higher compressive forces on the median nerve (March et al. 1988). Osteopenia and osteoporosis, defined by lower bone mineral density on dual-energy X-ray absorptiometry (DEXA) scans, were noted to be much more severe in perimenopausal women with signs of hypermobility than in a non-hypermobile control group (Gulbahar et al. 2006; Nijs et al. 2000). Fibromyalgia has been linked to hypermobility syndromes as well, although the chronic pain features inherent in the hypermobility type of EDS present similar findings and some overlap of these diagnoses is likely to be present (Acasuso-Díaz and Collantes-Estévez 1998).
Joint hypermobility may also offer a protective effect to bony structures by adding additional shock absorption via ligamentous structures to dissipate a force that may otherwise be sufficient to cause fracture. Accordingly, soft tissue trauma may be more severe than expected, and the patient’s clinical exam may be out of proportion to radiographic findings. Stanitski (1995) demonstrated that patients with hypermobility syndromes were 2.5 times more likely to sustain articular cartilage damage during patellar dislocations, findings that were only readily observed on magnetic resonance imaging studies. Rigorous activity also plays a role in regulating ligamentous laxity throughout the body (Crisco et al. 1997). Following repetitive exercises, wrist ligament stiffness was noted to decrease and gradually recover to baseline over 24 h, providing some protective effect to the wrist over that time period.
Although the connection between hypermobility syndromes and musculoskeletal disorders is well described, the biomechanical properties leading to the correlation have not been fully elucidated. High-level ruby players with hypermobility syndromes were three times more likely to sustain injuries to the shoulder, hip, knee, ankle, hand, or wrist throughout the course of a season (Stewart and Burden 2004). However, in a study of professional soccer players, those with joint hypermobility showed no difference in injury rates but did tend to require prolonged rehabilitation and missed more training days and games when compared to non-hypermobile controls (Collinge and Simmonds 2009).
In the elbow, Nork et al. (1999) demonstrated that increased elbow hyperextension, in association with generalized hypermobility, predisposed patients to sustain supracondylar humerus fractures at a higher rate than those without. The authors theorized that increased elbow hyperextension (10.5° vs. 4.4° in control group with both bone forearm fracture) during a fall on outstretched hand (FOOSH) placed increased torque along the supracondylar region, resulting in an increased likelihood of fracture through that region. They also noted that younger children tended to have increased joint mobility and a corresponding increased risk of supracondylar humerus fractures .
Assessment
The assessment of joint laxity was initially introduced to assist in the evaluation of infantile developmental hip dislocation. Carter and Wilkinson (1964) showed that ligamentous laxity of more than three joints (thumb touching the forearm in wrist flexion, finger MCP hyperextension parallel to forearm in wrist extension, elbow and knee hyperextension greater than 10°, and excess ankle dorsiflexion and eversion) was noted in 45 % (33/74) of patients with infantile hip dislocation, but only in 7 % of a control group of local schoolchildren. They also noted that joint hyperlaxity had a strong familial component and demonstrated that hip dislocation was noted in 64 % of patient with a first-degree relative with hip dislocation. Beighton and Horan (1969) expanded upon the Carter and Wilkinson assessment by substituting spine hypermobility (the ability to touch the palm to the floor while keeping the knees extended) for ankle hyperdorsiflexion and creating a hypermobility score of 0–5, utilizing an average score for the paired joints in the extremities. They described 100 patients with EDS, showing that most obtained a hypermobility score of at least 3, and many demonstrated considerable disability due to joint instability, arthritis, or skin ulceration. In 1973, Beighton et al. (1973) modified the hypermobility score to include each individual joint separately, giving the current maximum score of 9 (Fig. 1, Table 1). Using this scale, a score of ≥4 is indicative of hypermobility (Grahame et al. 2000), although some authors define moderate hypermobility as a score of 3–4 and severe hypermobility as a score of ≥5 (Mikkelsson et al. 1996; Beighton et al. 1998; Juul-Kristensen et al. 2007). Over the years, the Beighton score has gained international acceptance as a screening test for joint hypermobility and has been validated as both reproducible and indicative of pathologic joint instability.
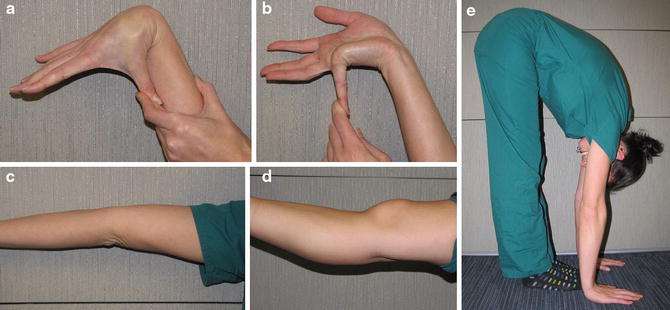
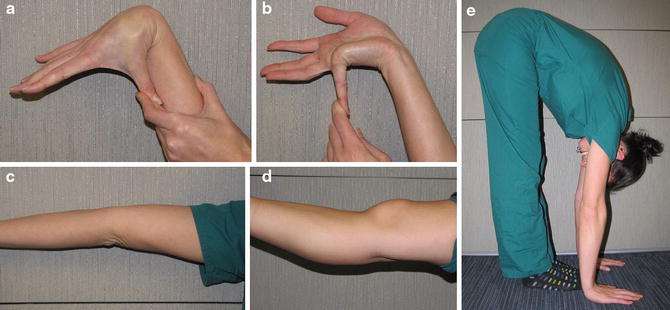
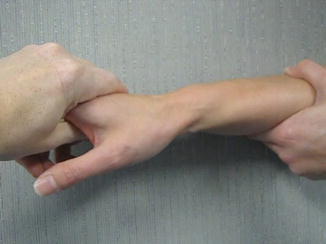
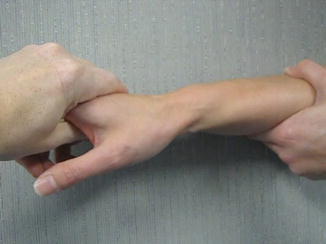
Fig. 1
Clinical photographs illustrating the criteria for Beighton score. (a) Thumb flexion to forearm. (b) Small finger MCP joint hyperextension to 90° (parallel to forearm). (c) Elbow hyperextension > 10°. (d) Knee hyperextension > 10°. (e) Truncal flexibility placing palms of hand flat on floor with knees fully extended (Photographs courtesy of Kevin J. Little, MD)
In the Rheumatology literature, the Brighton scale has gained more acceptance (Grahame et al. 2000) especially for the diagnosis of benign joint hypermobility syndrome (BJHS). The diagnosis of BJHS using the Brighton scale includes two major criteria and eight minor criteria. The major criteria are a Beighton score of ≥4 and arthralgias of ≥4 joints for greater than 3 months. The minor criteria include a Beighton score of 1–3, arthralgias of 1–3 joints for greater than 3 months, dislocation/subluxation of 1 joint, soft tissue rheumatism such as epicondylitis or tenosynovitis, marfanoid habitus, abnormal skin findings such as hypermobility or striae, ophthalmologic findings such as ptosis or myopia, and miscellaneous findings of hypermobility such as varicose veins, uterine/rectal prolapse, or hernia.
Injury assessment in individuals with ligamentous laxity proceeds, as in all patients, with a thorough history and physical examination. Patients may present many months after an initial, minor trauma with complaints of pain and disability far beyond what was initially present immediately following the injury. The history of present illness should incorporate all treatment modalities attempted since the dysfunction began, with special care noted as to any previous physiotherapy and which exercises were performed. Additionally, detailed information about previous injuries throughout the body should be obtained. The examiner should have a low index of suspicion and carefully evaluate for hypermobility syndromes, especially in patients where complaints appear out of proportion to physical exam or radiographic findings.
The physical examination should incorporate the Beighton score as a measure of generalized joint laxity as well as a more thorough examination of the affected joint. The affected area should be inspected for edema, ecchymosis, skin tears, or striae and palpated for the area of maximal tenderness. The active and passive ROM of the affected joint should be documented before specialized tests of joint hypermobility are performed. In the shoulder, a sulcus sign (Fig. 2) can be demonstrated with the patient seated or standing, by pulling inferiorly on the adducted shoulder, noting that greater than 2 cm of inferior translation is indicative of shoulder instability. The anterior apprehension sign is elicited with the shoulder abducted to 90°, placing anteriorly directed force combined with external rotation at the shoulder joint, followed by the Relocation test that is done by then placing a posteriorly directed force on the shoulder to assess for relief from shoulder apprehension. Similarly, the posterior apprehension sign is elicited with the shoulder forward flexed to 90° and internally rotated, placing a posteriorly directed force at the shoulder joint. Additionally the Jerk test can be performed in a similar arm position with a rapid posteriorly directed force placed upon the shoulder which can produce painful and palpable posterior subluxation, which is then relieved, often with a palpable clunk, with gradual extension of the arm (Ho et al. 2007). The diagnosis of multidirectional instability occurs when a patient exhibits signs of pathologic instability in more than one anatomical direction, either anteriorly, posteriorly, or inferiorly. Unidirectional or multidirectional instability may occur in the setting of underlying ligamentous laxity, and a careful assessment of both affected and unaffected joints is crucial towards understanding the nature of the patient’s complaints (Cameron et al. 2010).

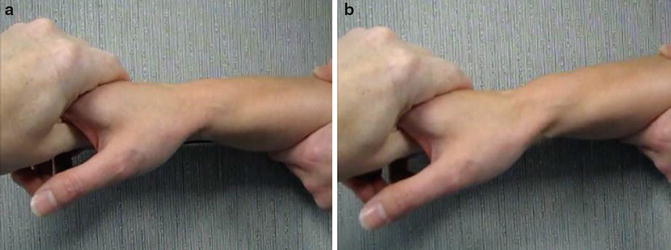

Fig. 2
Clinical photograph illustrating a positive sulcus sign in the shoulder (Photograph courtesy of Kevin J. Little, MD)
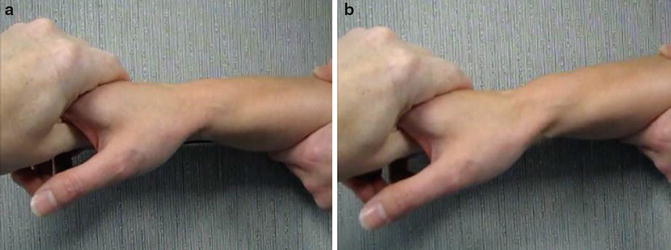
Fig. 3
Clinical photograph illustrating a patient with midcarpal instability. (a) In neutral position and (b) demonstration of midcarpal instability elicited by pronation and volar pressure on the stabilized wrist (Photograph courtesy of Kevin J. Little, MD)
Examination of the elbow includes an assessment of ROM and hyperextension of the joint. Further instability of the elbow is typically pathologic indicative of laxity or tearing of the medial or lateral ulnar collateral ligament injury, which is assessed by placing valgus and varus stress, respectively, on the joint. Additionally, the lateral pivot-shift test is utilized to assess for posterolateral instability by placing an axial and valgus compressive on the elbow in 40° elbow flexion and full forearm supination (Video 1). The assessment of instability of the elbow is often difficult in a non-sedated patient due to dynamic stability provided by the periarticular musculature, and an exam under anesthesia, including elbow arthrogram, is recommended (Messmer and Ruch 2007).


Video 1
Video demonstrating the pivot-shift test for elbow posterolateral instability (Video courtesy of Shriners Hospital for Children, Philadelphia)
Assessment of the hand and wrist follows a similar protocol, beginning with inspection to assess for subluxation of the thumb CMC joint or volar/ulnar sag of the wrist, palpation and ROM examination. The assessment of midcarpal instability is performed by placing the wrist in a pronated and ulnarly deviated position and applying volarly directed pressure on the hand, which can generate a palpable clunk (Fig. 3), which is relieved with supination and a dorsally directed force (Video 2). Additionally, assessment of scapholunate instability via the Watson test and luno-triquetral (LT) instability via the LT compression and ballottement tests is recommended to assess for pathologic single ligament wrist instability (Rizzo 2007; van Vugt et al. 1999). Assessment of CMC subluxation and apprehension is performed by placing a dorsally directed force on the trapeziometacarpal joint.
Video 2
Video demonstrating the clinical test for midcarpal instability (Video courtesy of Kevin J. Little, MD)
Overall, this assessment should be performed bilaterally to ensure that the examiner can deduce the patient’s state of hypermobility and infer the locations where additional pathologic laxity is present. For patients with an unclear diagnosis or who have failed physiotherapy treatments, further evaluation with advanced imaging is indicated. For patients with soft tissue pain about the wrist, ultrasound has been utilized as an effective technique in aiding diagnosis of subcutaneous injury, whereas bone scintigraphy is best for subtle osseous abnormalities (van Vugt et al. 1999). Additionally, magnetic resonance imaging, especially when supplemented by arthrography, has shown excellent sensitivity and specificity for intra-articular pathology in the shoulder, elbow, and wrist (Lomasney et al. 2013) .
Treatment
In patients with hypermobility syndromes, the diagnosis is easily missed or delayed, which can lead to worsening pain and dysfunction prior to diagnosis (Grahame and Hakim 2008). While hypermobility by itself does not impart musculoskeletal damage, complaints of pain and dysfunction are common, especially in patients with more severe forms of hypermobility including Marfans or EDS (Rombaut et al. 2010). The key to treatment is to quickly identify a patient with hypermobility and initiate prompt treatment. In most cases, emphasizing musculoskeletal health and core strengthening exercise programs provides the best pathway to recovery following injury (Russek 1999). Patients with fibromyalgia and hypermobility who exercised regularly and had improved general fitness were demonstrated to have improved outcomes compared to those who did not (Ferrell et al. 2004; Goldman 1991). A recent systematic review of patients with benign joint hypermobility syndrome demonstrated that there is limited evidence on therapeutic regimens, but that proprioceptive-based therapeutic exercises and general physiotherapy are beneficial to children with BJHS and musculoskeletal pain (Smith et al. 2014). For patients with shoulder multidirectional instability, focused rotator cuff rehabilitation to impart additional dynamic stability has been advocated as the primary treatment modality (Burkhead and Rockwood 1992; Cameron et al. 2010). Following injury, patients with hypermobility syndromes may have a prolonged course of therapy in order to recover to pre-injury levels of pain and sports participation (Collinge and Simmonds 2009; Simmonds and Keer 2007). Surgical treatment is rarely indicated in patients with joint hypermobility and is limited to cases where additional traumatic injuries or pathologic instability is present despite adequate rehabilitation (Burkhead and Rockwood 1992; Cameron et al. 2010; Neer and Foster 1980).
Nonoperative
Any patient that presents with chronic musculoskeletal pain or symptoms out of proportion to physical exam findings should be evaluated for generalized joint hypermobility using the Beighton score. Once the diagnosis of acute or chronic injury in the setting of ligamentous laxity has been made, focused therapeutic exercises towards the affected joint are prescribed in addition to general fitness and core strengthening exercises. These include joint proprioception, active strengthening about the affected joint, range-of-motion exercises, and desensitization if necessary. For the shoulder, rotator cuff strengthening, periscapular stabilization, and proprioception are recommended. In the wrist, a grip strengthening protocol is initiated. By focusing or grip strengthening, the forearm flexor and extensor musculature can perform isometric strengthening with minimal joint motion, whereas using traditional isotonic (lifting a weight) exercises places substantial stress on the wrist joint and may aggravate pain complaints.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


